INTRODUCTION
Pituitary apoplexy characterized by sudden onset of headache, nausea, vomiting, visual disturbances, ophthalmoplegia and decreased level of consciousness was described for the first time by Bailey
1) in 1898 and then by Bleibtreu
4) in 1905. However, the term 'pituitary apoplexy' was coined by Brougham et al.
5) later, in 1950. Pituitary apoplexy is an acute clinical syndrome caused by either hemorrhage or infarction of a pre-existing pituitary adenoma. Pituitary apoplexy after cardiac surgery is a very rare perioperative complication. Many factors have been implicated as its precipitating factors, including anticoagulants and major surgery that can cause fluctuations in blood pressure
3,
14). Here, we present a rare case of pituitary apoplexy after mitral valvuloplasty with missed pituitary macroadenoma before cardiac surgery, despite pre-operative brain magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA).
Go to :

CASE REPORT
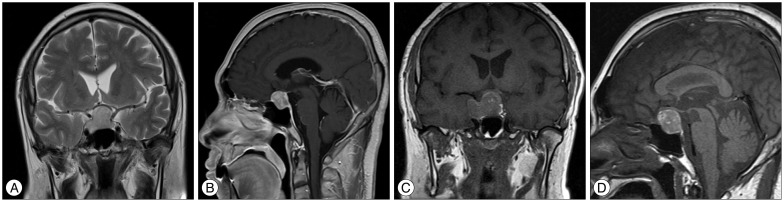
A 69-year-old man suffering from chest pain and dyspnea was diagnosed with severe non-rheumatic mitral regurgitation and was admitted to the department of cardiothoracic surgery. His past medical history revealed hypertension and cataract surgery on both eyes. There were no prior symptoms and signs that suggested neuro-ophthalmologic or endocrine disease. Brain MRI and MRA were performed preoperatively to rule out the cerebrovascular lesions. After conventional general anesthesia and systemic heparin administration, uncomplicated open heart mitral valvuloplasty was performed with the use of cardiopulmonary bypass (CPB). Upon awakening from the procedure, the patient reported a severe headache, a visual field defect, and double vision. In neurological examination, he was found drowsy with a right 3rd, 4th, and 6th cranial nerve palsy, and bitemporal hemianopsia. The retrospective review of the brain MRI showed a sellar mass with suprasellar extension suggestive of pituitary macroadenoma (
Fig. 1A, B). Upon suspicion of pituitary apoplexy, urgent pituitary MRI was performed. The lesion showed intermediate to high signal intensity in the T1-weighted images, mixed signal intensity in the T2-weighted images, and rim-enhancement after gadolinium administration, which suggested hemorrhage (
Fig. 1C, D). The pituitary function test results were within the normal limits. Pituitary apoplexy was presumptively diagnosed, and treatment with high-dose steroids was begun. Trans-sphenoidal resection of the tumor was performed 24 hours after the mitral valvuloplasty. The histopathologic examination revealed a necrotic pituitary adenoma with secondary hemorrhage, consistent with pituitary apoplexy (
Fig. 2). The patient showed an uneventful recovery. During the one-year follow-up, the patient showed complete recovery of ophthalmoplegia and improved visual field defect. The MRI revealed no residual tumor (
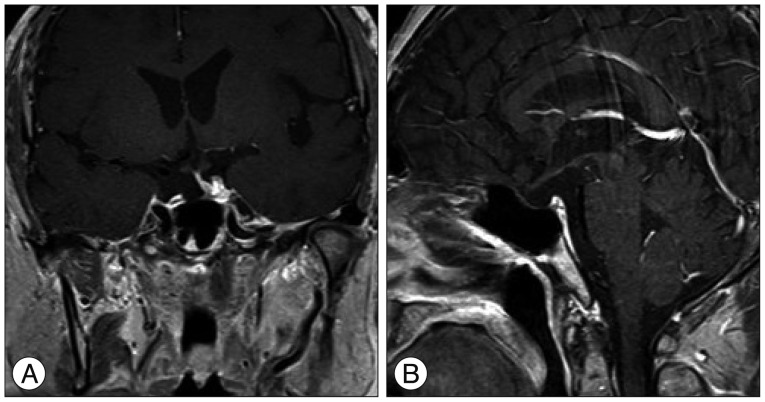
Fig. 3).
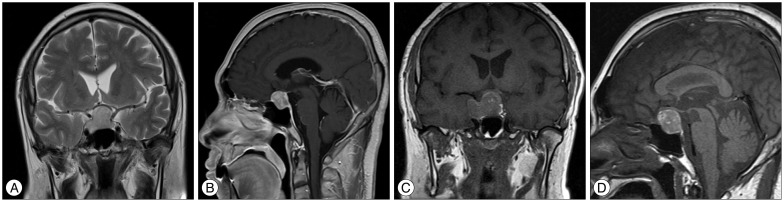 | Fig. 1Preoperative brain magnetic resonance (MR) images. The T2-weighted coronal (A) and T1-weighted gadolinium sagittal MR images (B) performed before the valvuloplasty demonstrated a 27×17×20 mm mass in the sella turcica with suprasellar extension. The non-contrast T1-weighted MR images (C and D) performed the day after the valvuloplasty revealed slight enlargement of the mass and increased signal intensity suggesting hemorrhage.
|
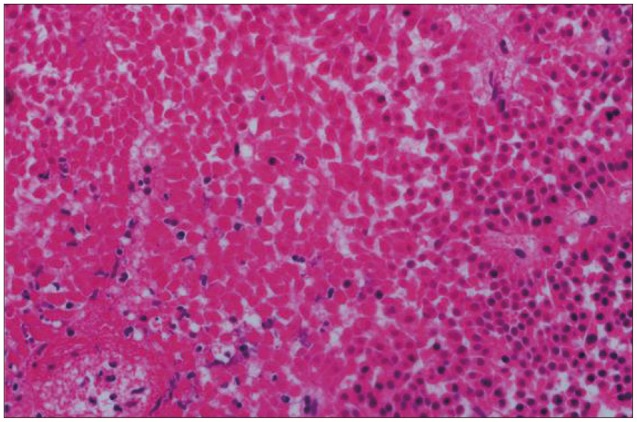
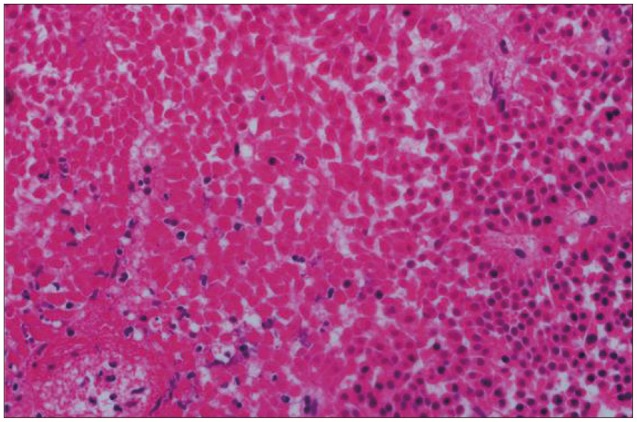 | Fig. 2Histopathological feature of the specimen. Photomicrograph showing tumor cells with coagulative necrosis suggesting pituitary apoplexy (H&E, ×400).
|
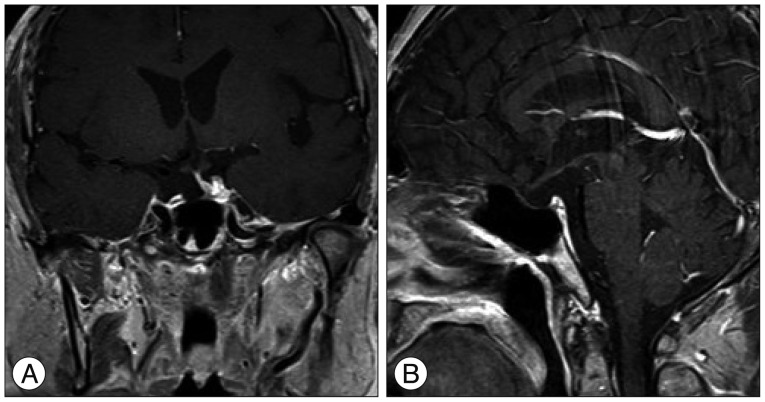 | Fig. 3Postoperative brain MR images. At the 1 year post-transsphenoidal resection of the tumor, there was no evidence of remnant tumor (A : coronal, B : sagittal).
|
Go to :

DISCUSSION
Pituitary apoplexy is a rare but potentially life-threatening clinical syndrome caused by the sudden enlargement of a pre-existing pituitary adenoma secondary to hemorrhage, hemorrhagic infarction or infarction
2,
6,
9). The pathophysiology of pituitary apoplexy is not precisely known, but many precipitating factors have been implicated, including head trauma, hypotension, a history of irradiation, cardiac surgery, pituitary dynamic testing, and anticoagulant therapy
14). Biousse et al.
3) categorized the pathogenesis of the pituitary apoplexy into four types : 1) reduced blood flow in the pituitary gland, 2) acute increase in blood flow in the pituitary gland, 3) stimulation of the pituitary gland by endogenous or exogenous hormones such as estrogen and steroid, and 4) an anticoagulated state.
The predisposing factors of pituitary apoplexy associated with cardiac surgery are more multifactorial and slightly differ from those of a normal pituitary gland. First, pituitary adenoma itself is predisposed to hemorrhage and necrosis. Most cases of pituitary apoplexy after cardiac surgery are associated with pituitary adenoma, especially macroadenoma. The blood vessels of adenomas have vasculopathic characteristics such as abnormal sinusoids, thin walls, and fibrinoid necrosis, which make adenomas susceptible to apoplexy
6,
15). Excessive stimulation of a pituitary adenoma by a large amount of steroids in response to surgical stress has also been postulated with respect to pituitary apoplexy
3).
Hemodynamic instability during cardiac surgery may contribute to pituitary apoplexy. Any cause of the reduction of cerebral perfusion pressure can contribute to infarction of adenomas and subsequent hemorrhage, such as positive pressure ventilation, hemodialysis, and major surgery
7,
8).
The CPB procedure during cardiac surgery may also predispose adenomas to apoplexy. During cardiac surgery, CPB-induced cerebral edema may contribute to the critical enlargement of silent pituitary adenomas
12). Indeed, systemic anticoagulation during CPB can make adenomas susceptible to hemorrhage
13). The absence of pulsatile flow during CPB and reperfusion injury with the restoration of the physiological circulation after CPB may also increase the risk of hemorrhage in a pre-existing adenoma
7).
Accordingly, Levy et al.
10) suggested that in patients with known pituitary adenomas, the performance of an 'off pump', also known as "beating heart surgery", should be considered. But, a case report of pituitary apoplexy even after off-pump coronary artery bypass grafting has been noted
11). However, it should be pointed out that the excessive anticoagulation might have caused the pituitary apoplexy in this case, as the authors mentioned.
The therapeutic strategy for patients with a known pituitary adenoma who require open heart surgery with CPB remains unclear. Once the pituitary adenoma is recognized before cardiac surgery, either known or revealed from preoperative imaging studies as in the present case, trans-sphenoidal resection of the adenoma should be considered
11). However, if the patient's condition is unstable, cardiac surgery should be performed first, on the 'off pump'
10). There are several reports of pituitary apoplexy after cardiac surgery. However, the present case is unique, because the cardiovascular surgeon and the neurologist did not recognize the pituitary macroadenoma before the cardiac surgery despite the performance of preoperative brain MRI and MRA to rule out cerebrovascular diseases. Since the pituitary macroadenoma was found in the preoperative brain MRI, 'off pump' cardiac surgery or trans-sphenoidal resection of the adenoma should have been considered first, as mentioned previously, to avoid the risk of pituitary apoplexy.
Pituitary apoplexy requires a high index of suspicion in any postoperative patients with neuro-ophthalmological symptoms, in which case urgent surgical decompression should be considered
16). Without strong contraindications after cardiac surgery, early surgical decompression is recommended not only to improve the neurological symptoms, but also to enhance the pituitary function, as in the present case
14).
Go to :

CONCLUSION
Neuroimaging should be required preoperatively to evaluate cerebrovascular diseases and pituitary adenomas before cardiac surgery, and it is essential to review images thoroughly because of the risk of pituitary apoplexy after cardiac surgery. Moreover, trans-shpenoidal resection of a tumor should be considered before open heart surgery when pituitary adenoma was identified during the preoperative evaluation if the patient's condition is stable.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download