Abstract
Objective
Pedicle screw fixation for spine arthrodesis is a useful procedure for the treatment of spinal disorders. However, instrument failure often occurs, and pedicle screw loosening is the initial step of a range of complications. The authors recently used a modified transpedicular polymethylmethacrylate (PMMA) screw augmentation technique to overcome pedicle screw loosening. Here, they report on the laboratory testing of pedicle screws inserted using this modified technique.
Methods
To evaluate pullout strengths three cadaveric spinal columns were used. Three pedicle screw insertion methods were utilized to compare pullout strength; the three methods used were; control (C), traditional transpedicular PMMA augmentation technique (T), and the modified transpedicular augmentation technique (M). After control screws had been pulled out, loosening with instrument was made. Screw augmentations were executed and screw pullout strength was rechecked.
Results
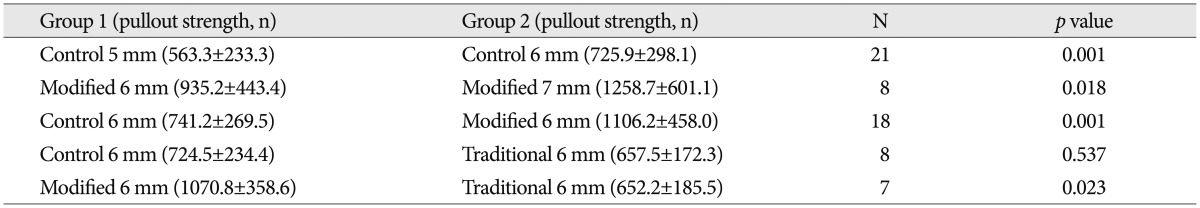
Pedicle screws augmented using the modified technique for pedicle screw loosening had higher pullout strengths than the control (1106.2±458.0 N vs. 741.2±269.5 N; p=0.001). Traditional transpedicular augmentation achieved a mean pullout strength similar to that of the control group (657.5±172.3 N vs. 724.5±234.4 N; p=0.537). The modified technique had higher strength than the traditional PMMA augmentation technique (1070.8±358.6 N vs. 652.2±185.5 N; p=0.023).
Conclusion
The modified PMMA transpedicular screw augmentation technique is a straightforward, effective surgical procedure for treating pedicle screw loosening, and exhibits greater pullout strength than traditional PMMA transpedicular augmentation. However, long-term clinical evaluation is required.
Pedicle screw fixation (PSF) for spine arthrodesis is a useful procedure for the treatment of spinal disorders. However, instrument failure often occurs, and pedicle screw loosening is the initial step of a range of complications9). If a pedicle screw loosens, it could cause other complications and be difficult to treat. In particular, if a problematic screw hole is larger than the biggest screw, it is difficult to achieve strong fixation during re-operation.
Traditionally, transpedicular screw augmentation with polymethylmethacrylate (PMMA) is used to overcome this problem. Traditional transpedicular screw augmentation (the traditional technique) exploits the anchoring properties of PMMA and achieves fixation strength than non-augmented screws2).
Recently, a modified transpedicular screw augmentation method was devised to recover loosened pedicle screws8,9); we refer to this modified technique as the transpedicular PMMA expandable anchor bolt screw (EABS) technique, which as its name implies, also utilizes the anchoring properties of PMMA. After filling the dead space of a problematic screw hole with 1-2 cc of PMMA, a small screw is inserted. After the PMMA has hardened, this screw is removed and a larger screw is then inserted to 'expand' the PMMA thread to achieve more strong fixation (Fig. 1). PMMA EABS could be applicable in cases of instrument failure caused by loosened pedicle screws or in cases of intraoperative pedicle screw loosening, which sometimes occurs in osteoporotic patients2,12).
Other PMMA screw augmentation techniques like intraoperative vertebroplasty can provide excellent screw fixation in difficult cases, but large amounts of PMMA are required to achieve strong fixation7). Furthermore, large amounts of PMMA increase the risk of extraosseous extravasation, which elevates complication rates4,17). On the other hand, the transpedicular PMMA EABS screw augmentation technique (the modified technique) is considered to provide strong fixation with a relatively small amount of PMMA.
In the present study, we assessed the pullout strengths of the traditional and modified techniques in the process of treating pedicle screw loosening, and sought to answer the following questions : 1) Does this modified technique increase the screw fixation power? 2) Is it suitable for use in osteoporosis patients? 3) Which provides stronger fixation, the modified or the traditional technique?
To evaluate and compare the pullout strengths of traditional and modified transpedicular screw augmentation, we used three cadaveric specimens. We extracted non-augmented control screws and then implanted screws using the two different augmentation processes; non-augmented control screws (C), traditional transpedicular PMMA augmented screws (T), and modified PMMA augmented screws (M).
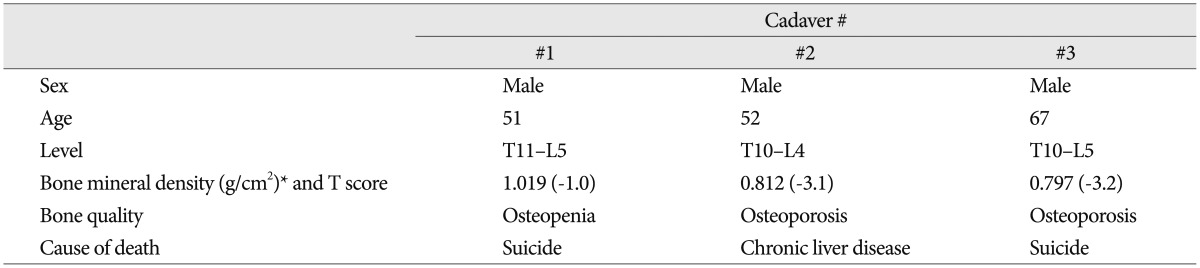
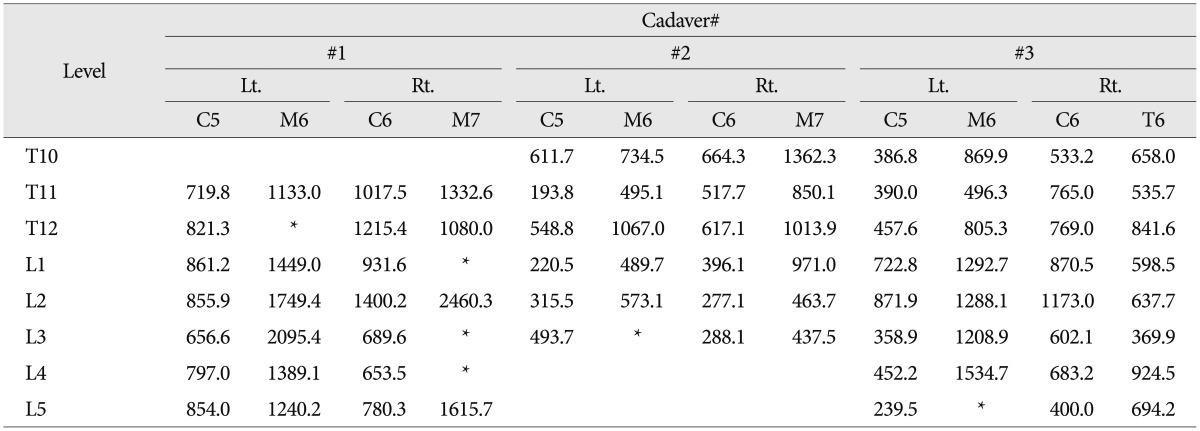
Twenty thoracolumbar vertebrae (T10-L5) from three human cadavers were harvested and separated in this study. The medical histories of specimens were investigated, and bone mineral densities (BMDs) of specimens were determined by dual X-ray absorptiometry (Lunar Prodigy Advance, GE Healthcare, Madison, WI, USA). Specimens were then classified as osteoporotic or non-osteoporotic using a BMD of -2.5 T score as a cutoff (Table 1). Soft tissue was removed, and portions of the transverse and spinous processes were removed to mount specimen to a jig. For convenience, long screws (USS fracture, Synthes, Oberdorf, Switzerland) were used for the screw pullout test. PMMA (Kyphx, Kyphon Europe, Zaventem, Belgium) was used for screw augmentation. Pullout strengths were measured using a universal testing machine (UTM) (858 Mini Bionix II, MTS systems, Minneapolis, MN, USA).
The three types of pedicle screw insertion techniques were compared. Control (C), non-augmented; traditional transpedicular augmentation (T); and modified transpedicular augmentation (M). Pullout failure strengths were measured.
1) Control pedicle screw insertion and followed by pullout strength measurements.
2) Screw loosening model making after Control screw removal using high speed drill : diameter 7 mm, depth 35 mm.
3) Group M, 6 mm diameter screw insertion followed by pullout strength measurements using the left pedicles of Cadavers #1, #2, and #3.
4) Group M, 7 mm diameter screw insertion followed by pullout strength measurements using the right pedicles of Cadavers #1 and #2.
5) Group T, 6 mm diameter screw insertion followed by pullout strength measurements using the right pedicles of Cadaver #3.
Control screws were inserted along the long axis of each pedicle using image-guided techniques under C-arm fluoroscopy6). Control screws were pulled out and pullout strengths were measured. Loosening holes were made using high speed drill fitted with a 7 mm burr along the long axis of pedicle. The PMMA mixture (1.0 g powder and 1 cc solvent) was applied to each prepared screw hole.
Group (T) and Group (M) were prepared as follows; Screws (6 mm diameter) were used in Group (T), and in Group (M), 5 mm pilot screws were replaced with a 6 mm permanent screw. Screws were inserted to a depth of 35 mm. Screw pullout strengths were evaluated using the same UTM-based method.
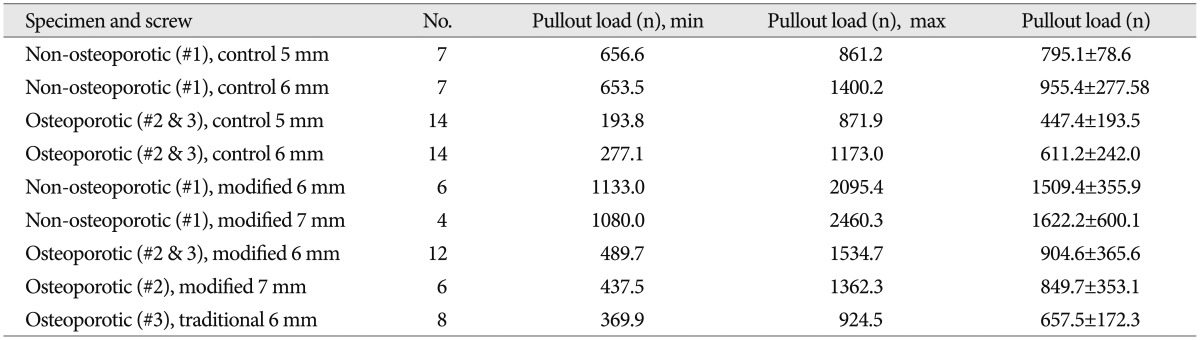
To obtain more data regarding osteoporosis in Group (M), augmentation was used with screws of different thicknesses (Cadavers #1 and #2) (Table 2).
Groups (T) and (M) were compared in only one osteoporotic specimen (Cadaver #3). Group (M) screw placements were done on left side and Group (T) placements on the right (Table 2).
All specimens were from males. The BMD of one cadaveric specimen was determined to be non-osteoporotic, but the other two were osteoporotic (Table 1).
In Group (C), 5 mm and 6 mm screws had mean pullout strengths of 563.3±233.3 N and 725.9±298.1 N, respectively. In Group (M), 6 mm and 7 mm screws had mean pullout strengths of 935.2±443.4 N and 1258.7±601.1 N, respectively, and in Group (T) 6 mm screws had a mean pullout strength of 657.5± 172.3 N (Table 3, 4).
Thicker screws in Group (C) had greater pullout strengths, regardless of BMD, and pullout strengths in non-osteoporotic specimens were greater than that in osteoporotic specimens (p<0.05) (Table 3).
After PMMA augmentation, Group (M) (1106.2±458.0 N) had a greater mean pullout strength than Group (C) (741.2±269.5 N) (p=0.001). Mean pullout strengths were similar in Group (T) (657.5±172.3 N) and Group (C) (724.5±234.4 N) (p=0.537), and mean pullout strength was greater in Group (M) (1070.8±358.6 N) than in Group (T) (652.2±185.5 N) (p=0.023) (Table 4, Fig. 2).
This study was undertaken to compare the pullout strength of modified transpedicular screw augmentation, named PMMA EABS with that of traditional transpedicular screw PMMA augmentation, especially in the context of pedicle screw loosening. It was found that PMMA EABS had greater pullout strengths than traditional PMMA screw fixation, especially in terms of achieving fixation to treat pedicle screw loosening. The traditional and the PMMA EABS techniques used were similar with the exception of; 1) the amount of PMMA used for screw augmentation, and 2) the expansile force produced by the thicker screw.
Due to the immediate strong fixation it provides, PSF is an essential surgical technique for the treatment of spinal disorders1,13). However, occasionally, complications associated with instrumentation require revision surgery. The incidence of pedicle screw loosening varies from 3.6% to 19%10,18), and in one report, 17% of revision surgeries were associated with pedicle screw failure5).
Biomechanically, pedicle screw loosening is associated with cyclic caudocephalad toggling at the bone-screw interface and low pedicle insertion torque in osteoporotic bone11,14,24). Recently, Choma et al.3) reported that a combined pullout/transverse force with a flexion bending moment better represents in vivo pedicle screw loosening.
The treatment options for screw loosening depend on clinical symptom. In one report, the presence of a radiolucent zone around screws showed no relationship to clinical results10), indicating that not all screw loosenings are associated with pseudoarthrosis. However, in another study, it was suggested that pedicle screw loosening is associated with pseudoarthrosis and back pain22). If screw loosening causes clinical symptoms, surgical treatment is required.
Several surgical strategies can be used to overcome screw loosening and associated instrument failure. One approach involves the replacement of loosened screws with thicker, longer screws, if possible12). Sometimes a laminar hook or sub-laminar wiring is used20). However, because pedicle screw loosening is usually associated with osteoporosis, surgical field extension of instrumentation and biomaterials that aid solid bone fusion should be applied. To achieve greater fixation strengths, PMMA transpedicular screw augmentation could be added2).
However, instrumented segment extension increases surgical morbidity and the possibility of complications. In the case of rescue screws, Pitzen et al.15) reported that thicker and longer rescue screws without augmentation did not produce any difference as compared with virgin screws for cervical plating.
PMMA screw augmentation guarantees strong screw fixation. Furthermore, complication rates associated with PMMA augmentation are acceptable. One limitation of PMMA augmentation is the large amount required to achieve strong fixation7), as large amounts of PMMA are associated with more extraosseous extravasation and higher complication rates4,17). Although the complication rates of PMMA augmentation are acceptable, several critical reports have been issued regarding its complications16). The ideal situation is to achieve a marked BMD improvement, but if this is not possible, the option would be to obtain strong fixation using less PMMA.
In this study, we measured the pullout strengths of modified PMMA transpedicular screw augmentation for loosened pedicle screws using the PMMA EABS technique, which is comparable to other expandable pedicle screws and devices that increase implant friction to bone using metal or interdigitated PMMA19,21,23). PMMA EABS is straightforward and economical, because it does not require new equipment. More importantly, it appears to require relatively small amounts of PMMA. In the present study, PMMA EABS achieved greater fixation strengths using small amounts of PMMA than the traditional method.
Interestingly, traditional transpedicular screw augmentation had weaker pullout results than expected. Burval et al.2) reported that traditional transpedicular PMMA augmentation provides greater pullout strengths than control non-augmented screws. However, they compared the pullout strengths of normal pedicle screws and not those of pedicle screws in loosened holes. We believe that traditional transpedicular PMMA augmentation is impractical for rescue purposes after screw loosening.
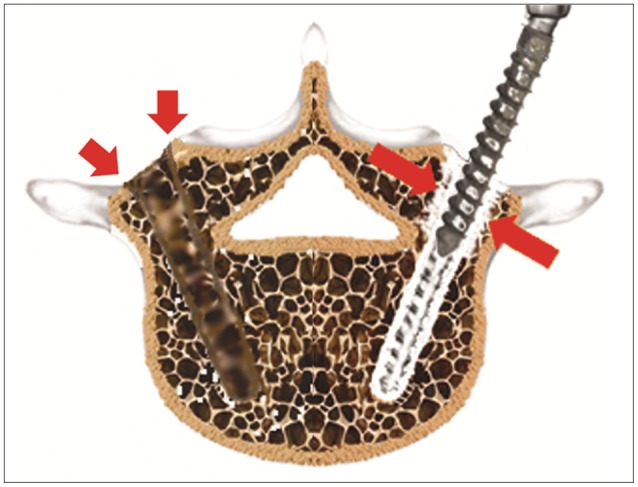
In our opinion, the absence of a cortical flange influences results. The interior surfaces of failed screw holes are usually smooth, and provide little scope for PMMA interdigitation. The overall appearance of failed holes is conical, and there is no flange to resist pullout (Fig. 3, left). For this reason, traditional transpedicular PMMA augmentation creates little adhesion between bone and PMMA, and the augmentation eventually slips. In the case of PMMA EABS, the insertion of a larger screw resulted in PMMA being impacted into cancellous bone, which we believe improves fixation strength (Fig. 3, right).
The possibility of pedicle breaches is a potential weakness of PMMA EABS when it is applied with a thicker screw to non-osteoporotic pedicles. In the present study, a 7 mm screw was applied to 2 specimens, one of which was osteoporotic. In the case of the non-osteoporotic specimen (#1), breaches occurred at 3 of 7 pedicles during PMMA EABS. However, no breach occurred during 7 mm screw insertion in the osteoporotic specimen (#2) (Table 2). BMD is related to pedicle breach during PMMA EABS, because in osteoporotic pedicles, there is some space within pedicles that might accommodate a thicker screw and the PMMA, whereas no space is available in non-osteoporotic pedicles.
In this study, PMMA EABS showed better pullout strengths for screws reinserted after loosening. However, the study is limited by the number of specimens used, a lack of BMD data for all vertebrae, and no pedicle morphometric data. Furthermore, only one mode of loading was used during testing. Nevertheless, we believe the modified EABS-based method offers the promise of successful rescue for pedicle screw loosening. Additional evidence should be obtained by clinical study on more cases with a long-term follow-up. Furthermore, in vivo studies are required of the PMMA-bone interface to help understand changes in osteoporotic bone after PMMA screw augmentation.
The described study shows that the PMMA EABS technique provides greater pullout strengths than traditional transpedicular screw PMMA augmentation for loosened pedicle screws. We believe that pedicle cancellous bone and PMMA are packed tightly by the thicker pedicle screw and that this improves screw holding power. We believe that the PMMA EABS approach could be used in osteoporosis patients with instrument failure.
Acknowledgements
This study was presented at the spring meeting of Korea Neurosurgical Society, 2011.
This article contains parts of a dissertation.
This study was supported by BioGreen21 Program (PJ01121401) of Rural Development Administration of ROK.
This work was supported by a grant from Hallym University Medical Center Research Fund (HURF 01-2012-24).
References
1. Bullmann V, Liljenqvist UR, Schmidt C, Schulte TL. [Posterior operative correction of idiopathic scoliosis. Value of pedicle screws versus hooks]. Orthopade. 2009; 38:198–200. 202–204. PMID: 19093095.
2. Burval DJ, McLain RF, Milks R, Inceoglu S. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae : biomechanical analysis of pedicle fixation strength. Spine(Phila Pa 1976). 2007; 32:1077–1083. PMID: 17471088.
3. Choma TJ, Frevert WF, Carson WL, Waters NP, Pfeiffer FM. Biomechanical analysis of pedicle screws in osteoporotic bone with bioactive cement augmentation using simulated in vivo multicomponent loading. Spine(Phila Pa 1976). 2011; 36:454–462. PMID: 20881517.

4. Denaro V, Longo UG, Maffulli N, Denaro L. Vertebroplasty and kyphoplasty. Clin Cases Miner Bone Metab. 2009; 6:125–130. PMID: 22461161.
5. Frankel BM, Jones T, Wang C. Segmental polymethylmethacrylate-augmented pedicle screw fixation in patients with bone softening caused by osteoporosis and metastatic tumor involvement : a clinical evaluation. Neurosurgery. 2007; 61:531–537. discussion 537-538. PMID: 17881965.
6. Fu TS, Wong CB, Tsai TT, Liang YC, Chen LH, Chen WJ. Pedicle screw insertion : computed tomography versus fluoroscopic image guidance. Int Orthop. 2008; 32:517–521. PMID: 17410363.

7. Jang JS, Lee SH, Kim KT, Kim BS, Lee WB. A Biomechanical Study on the Pull-Out Strength of Pedicle Screw Augmented with Polymethylmethacrylate(PMMA)- Cadaveric Study -. J Korean Neurosurg Soc. 2002; 31:45–49.
8. Jo JY, Kang SH, Park SW. Modified polymethylmethacrylate cervical plate and screw augmentation technique for intraoperative screw loosening. J Spinal Disord Tech. 2012; 25:235–239. PMID: 21423049.

9. Kang SH, Kim KT, Park SW, Kim YB. A case of pedicle screw loosening treated by modified transpedicular screw augmentation with polymethylmethacrylate. J Korean Neurosurg Soc. 2011; 49:75–78. PMID: 21494370.

10. Ko CC, Tsai HW, Huang WC, Wu JC, Chen YC, Shih YH, et al. Screw loosening in the Dynesys stabilization system : radiographic evidence and effect on outcomes. Neurosurg Focus. 2010; 28:E10. PMID: 20568916.
11. Law M, Tencer AF, Anderson PA. Caudo-cephalad loading of pedicle screws : mechanisms of loosening and methods of augmentation. Spine(Phila Pa 1976). 1993; 18:2438–2443. PMID: 8303446.
12. McLain RF, Fry MF, Moseley TA, Sharkey NA. Lumbar pedicle screw salvage : pullout testing of three different pedicle screw designs. J Spinal Disord. 1995; 8:62–68. PMID: 7711371.
13. Moore DC, Maitra RS, Farjo LA, Graziano GP, Goldstein SA. Restoration of pedicle screw fixation with an in situ setting calcium phosphate cement. Spine. 1997; 22:1696–1705. PMID: 9259778.

14. Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine(Phila Pa 1976). 2000; 25:858–864. PMID: 10751298.
15. Pitzen T, Franta F, Barbier D, Steudel WI. Insertion torque and pullout force of rescue screws for anterior cervical plate fixation in a fatigued initial pilot hole. J Neurosurg Spine. 2004; 1:198–201. PMID: 15347006.

16. Ploeg WT, Veldhuizen AG, The B, Sietsma MS. Percutaneous vertebroplasty as a treatment for osteoporotic vertebral compression fractures : a systematic review. Eur Spine J. 2006; 15:1749–1758. PMID: 16823557.

17. Shen Y, Ren H, Zhang Y, Zhi X, Ding W, Xu J, et al. [Correlative factor analysis of complications resulting from cement leakage after percutaneous kyphoplasty in treatment of osteoporotic vertebral body compression]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2010; 24:27–31. PMID: 20135966.
18. Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine : a multi-center study of a novel non-fusion system. Eur Spine J. 2002; 11(Suppl 2):S170–S178. PMID: 12384741.
19. Sugimoto Y, Tanaka M, Konishi H, Takigawa T, Nakanishi K, Misawa H, et al. Posterior spinal fusion using a pedicle nail system with polymethylmethacrylate in a paraplegic patient after vertebral collapse caused by osteoporosis. Spine J. 2009; 9:e5–e8. PMID: 18082464.

20. Sun E, Alkalay R, Vader D, Snyder BD. Preventing distal pullout of posterior spine instrumentation in thoracic hyperkyphosis : a biomechanical analysis. J Spinal Disord Tech. 2009; 22:270–277. PMID: 19494747.

21. Wan S, Lei W, Wu Z, Liu D, Gao M, Fu S. Biomechanical and histological evaluation of an expandable pedicle screw in osteoporotic spine in sheep. Eur Spine J. 2010; 19:2122–2129. PMID: 20577766.

22. Wetzel FT, Brustein M, Phillips FM, Trott S. Hardware failure in an unconstrained lumbar pedicle screw system. A 2-year follow-up study. Spine(Phila Pa 1976). 1999; 24:1138–1143. PMID: 10361664.
23. Wu ZX, Gao MX, Sang HX, Ma ZS, Cui G, Zhang Y, et al. Surgical treatment of osteoporotic thoracolumbar compressive fractures with open vertebral cement augmentation of expandable pedicle screw fixation : a biomechanical study and a 2-year follow-up of 20 patients. J Surg Res. 2012; 173:91–98. PMID: 21067776.

24. Zindrick MR, Wiltse LL, Widell EH, Thomas JC, Holland WR, Field BT, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986; 203:99–112. PMID: 3956001.

Fig. 1
Schematic illustrations of modified transpedicular polymethylmethacrylate (PMMA) screw augmentation. A : The vacant pedicle hole after loose pedicle screw removal is filled with PMMA of a toothpaste-like viscosity, the dead space was filled with 1 cc of PMMA for the biomechanical study. B : The inserted PMMA hardened after inserting a small pilot screw. C : An inner thread was left by the small screw after its removal. D : PMMA expansion (red arrows) caused by inserting the thicker permanent screw improved screw holding power (referred to as the anchor bolt effect). Adapted from Kang et al. J Korean Neurosurg Soc 49 : 75-78, 20119).
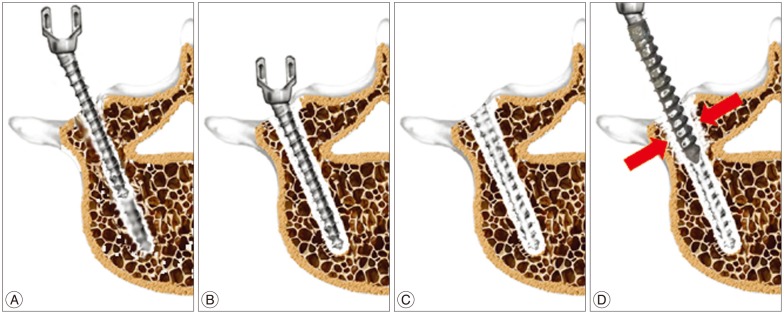
Fig. 2
Schematic diagram presenting pullout strengths (N) for the control (C), traditional (T), and modified (M) techniques. A 6 mm screw was used to measure pullout strengths. The paired t test was used for the statistical analysis. Lt. : left, Rt. : right.
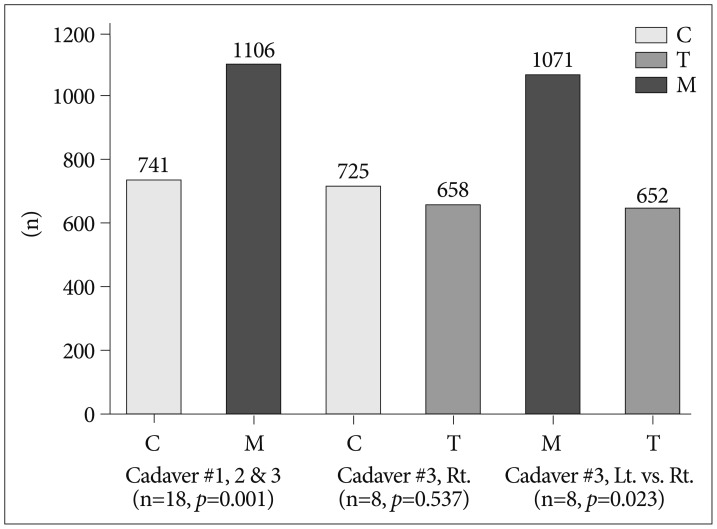
Fig. 3
Schematic illustrations of loosening holes, showing a loosened screw hole on the left side and modified transpedicular polymethylmethacrylate (PMMA) augmentation on the right. Loosened pedicle screw hole exhibits a conical shape with no flange (red arrows). Modified transpedicular screw augmentation increases screw holding power (short red arrows) even without a flange and with only slight PMMA interdigitation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download