Abstract
Objective
Posttraumatic cerebral infarction (CI) is a well-known complication of traumatic brain injury (TBI). However, the causation and apportionment of trauma in patients with CI after TBI is not easy. There is a scoring method, so-called trauma apportionment score (TAS) for CI, consisted with the age, the interval, and the severity of the TBI. We evaluated the reliability of this score.
Methods
We selected two typical cases of traumatic CI. We also selected consecutive 50 patients due to spontaneous CI. We calculated TAS in both patients with traumatic and spontaneous CI. To enhance the reliability, we revised TAS (rTAS) adding three more items, such as systemic illness, bad health habits, and doctor's opinion. We also calculated rTAS in the same patients.
Results
Even in 50 patients with spontaneous CI, the TAS was 4 in 44 patients, and 5 in 6 patients. TAS could not assess the apportionment of trauma efficiently. We recalculated the rTAS in the same patients. The rTAS was not more than 11 in more than 70% of the spontaneous CI. Compared to TAS, rTAS definitely enhanced the discriminating ability. However, there were still significant overlapping areas.
Posttraumatic cerebral infarction (CI) is a well recognized complication of traumatic brain injury (TBI) and is frequently associated with a poor outcome17). However, its frequency, timing, and risk factors are not well-defined17). Furthermore, few data are available to quantify risk factors related to the occurrence of CI following TBI. Medical consideration of the causation and apportionment of trauma in patients with CI has utmost importance in compensation or reparation. However, differentiation of spontaneous and traumatic CI is often almost impossible. Comprehensive analysis on the etiology of a certain case of CI may lack objectivity, even though the assumption is correct. Scoring system using risk factors may provide the possibility more objectively and quantitatively. There is a scoring method, so-called trauma apportionment score (TAS) for CI, which was consisted with three items, such as the age, the interval from injury to CI, and the severity of the TBI11). However, reliability of this method was not been verified. We evaluated the reliability of this score.
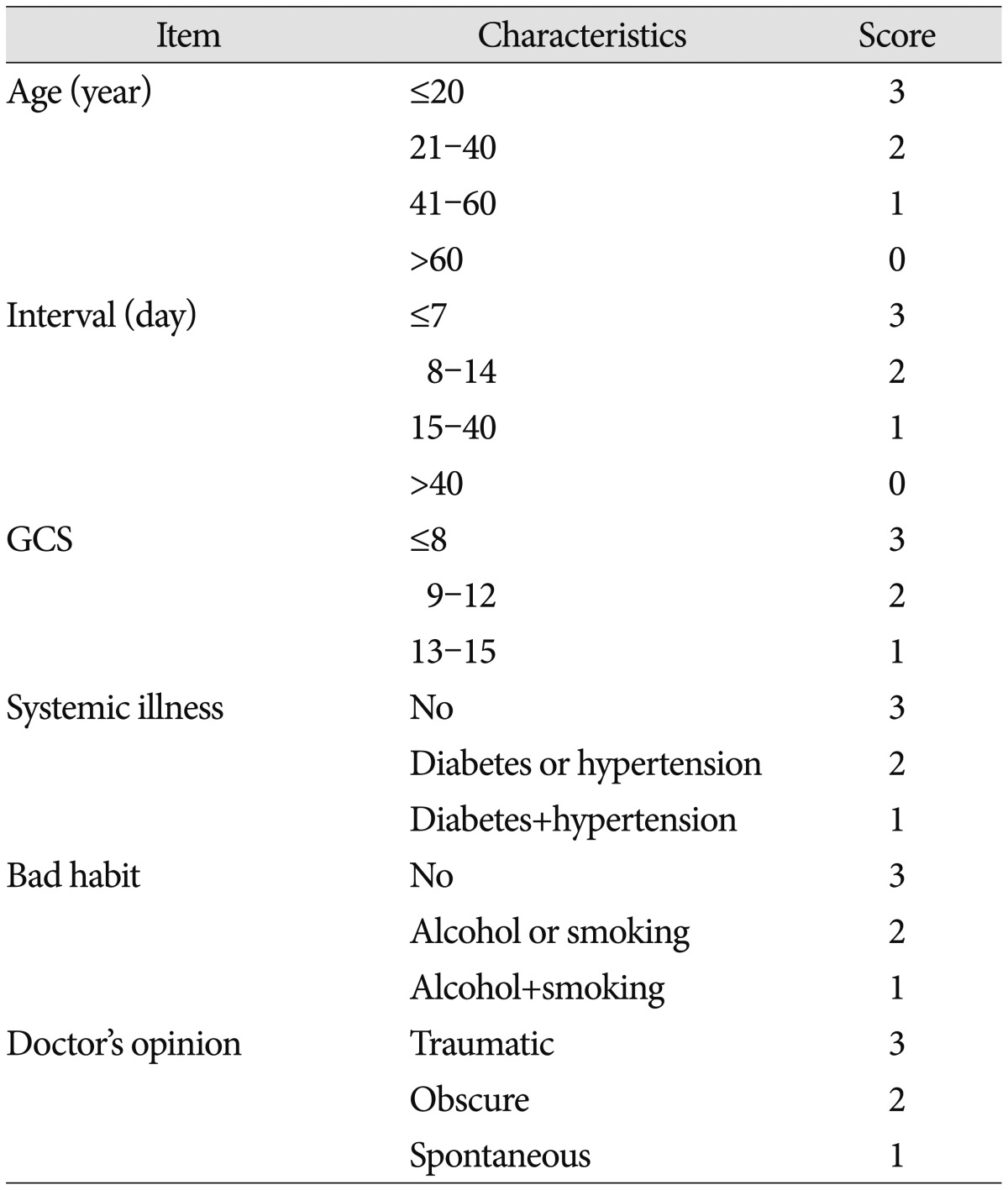
We calculated TAS in both patients with traumatic and spontaneous CI. We selected two typical cases of traumatic CI from the Korean literature. Both cases were reported as traumatic CIs9,15). We also selected consecutive 50 patients, who admitted this hospital in 2012 due to spontaneous CI. CI was confirmed by magnetic resonance imaging and/or computed tomography (CT). CI was classified into lacunar infarction (23 cases), territory infarction (22 cases), border-zone infarction (3 cases), and cerebellar infarction (2 cases) by the radiological findings. TAS for CI was consisted with three items, such as the age, the interval from injury to CI, and the Glasgow coma score (GCS) after the TBI (Table 1). When TAS was calculated in the patients with spontaneous CIs, the interval and GCS scores were supposed as 3 (within 7 days) and 1 (GCS 13-15).
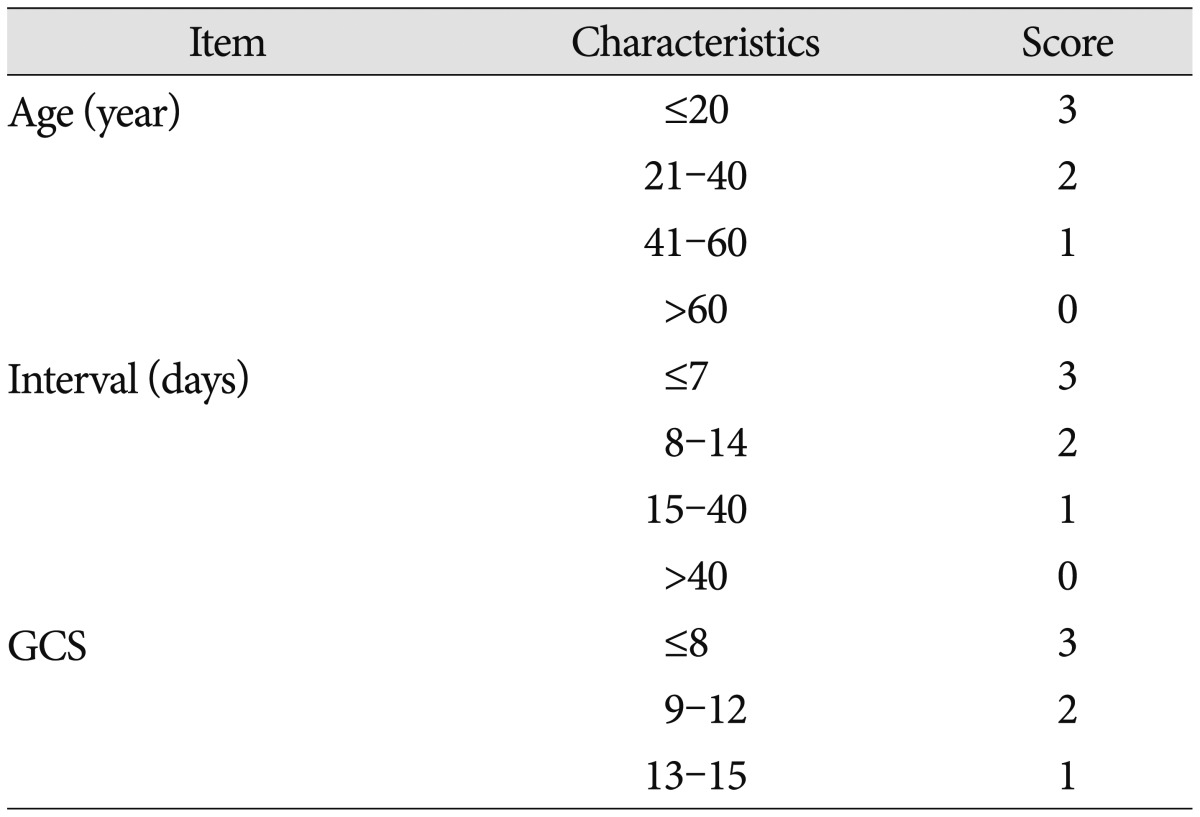
To enhance the reliability, we revised TAS (rTAS) adding three more items, such as systemic illness, bad health habits, and doctor's opinion (Table 2). We also calculated rTAS in selected patients with typical and spontaneous CIs. The doctor's opinion was supposed as 2 (obscure).
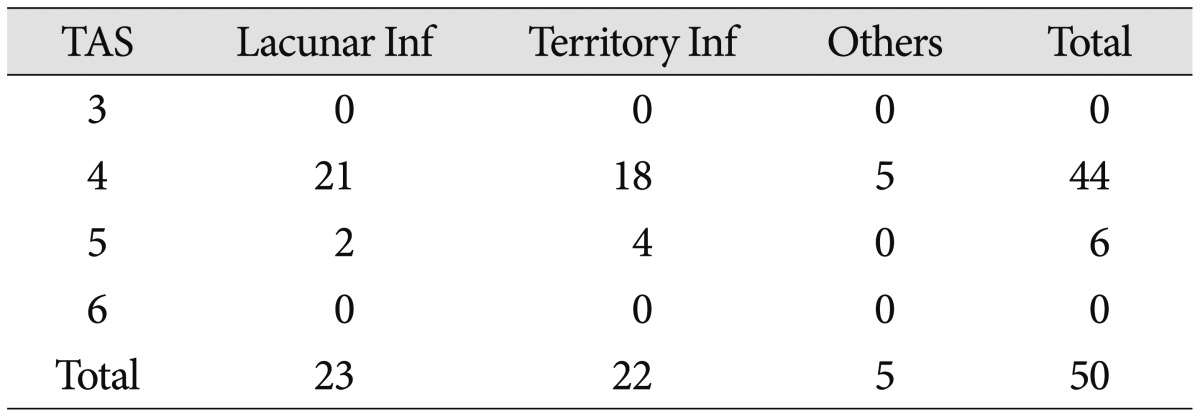
The TAS was 8 in the 26-year-old male15), which implied the apportionment ranged 80 to 100 percent. However, the TAS was only 4 in the 38-year-old male9), which implied the apportionment ranged 50 to 70 percent. Even in 50 patients with spontaneous CI, the TAS was 4 in 44 patients, and 5 in 6 patients (Table 3). TAS 4 or 5 meant the apportionment reached up to 70 percent. TAS with three items failed to differentiate the apportionment of trauma efficiently, especially when the age was young.
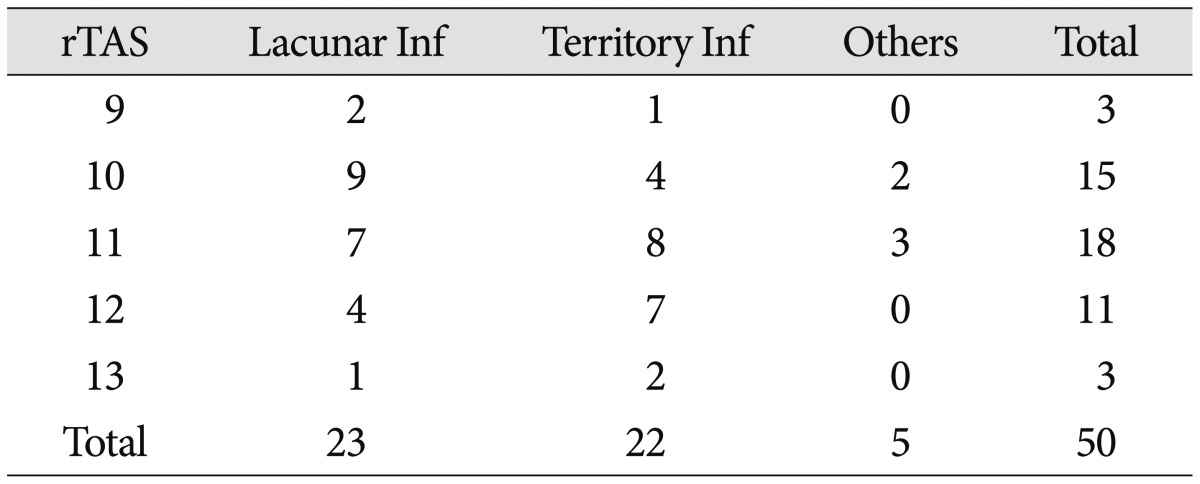
We recalculated rTAS in both patients with traumatic and spontaneous CI. In 50 patients with spontaneous CI, the rTAS was less than 12 in 36 patients, and 12 in 11 patients (Table 4). The rTAS was 17 in the 26-year-old male15), which implied the apportionment ranged 81 to 100 percent. The rTAS was still 12 in the 38-year-old male9), which implied the apportionment ranged only 21 to 40 percent. Although the rTAS may enhance the discriminating ability, there were still significant overlapping areas.
The TAS was only 4 even in a patient with traumatic CI. Furthermore the TAS 4 or 5 was quite common in patients with spontaneous CI. TAS with three items only failed to differentiate the traumatic CI from the spontaneous CI efficiently.
Posttraumatic CI is a well-known complication of TBI, with a frequency ranging from 1.9% to 10.4%2,6,12,14,16,17). Posttraumatic CI may occur secondary to focal mass effect, vascular impingement usually caused by herniation, cerebral vasospasm, thromboembolism, cerebrovascular injury, systemic hypoperfusion or venous congestion at craniectomy sites6,12,14,16). The multivariate analysis identified that low GCS, low systolic blood pressure (BP), brain herniation, and decompression craniotomy were risk factors for CI in patients with moderate or severe TBI17). To diagnose a traumatic CI, the following criteria should be satisfied : 1) there should be a radiological evidence, 2) there should be an acute onset of corresponding clinical signs and symptoms, and 3) patients should not have a history of cerebral infarction or low-density lesions as possible surgical or traumatic complications17). As a radiological evidence, there should be a distinctly low-density area within a defined cerebral vascular territory, involving the entire territory (complete) or part of it (incomplete), or situated in the terminal zones of perforating arteries within the deep white matter was identified on repeated CT scans, and the admission CT revealed no abnormality in same area17). However, these criteria cannot be sufficient to evaluate the causation of the CI after TBI. Since a spontaneous CI can be developed after a TBI, a CI after a TBI does not mean the cause is trauma. To evaluate the causation or apportionment of trauma on the CI, we should explore various risk factors of ischemic strokes and pathophysiological effects of TBIs. That is the reason that the TAS was proposed. TAS for CI was made using the following three items.
The incidence of stroke rises exponentially with age and is therefore low in young adults5). Only 3 % of CIs occur in patients under the age of 407), and about 10% of all strokes occur in patients <50 years of age8). In Korea, about 5% of spontaneous CIs including transient ischemic attacks, occurred in patients under the age of 404). Injury itself alters hemostasis, although the exact pathways remain elusive18). Platelet aggregation was not associated with injury severity, shock or severe brain injury18). TBI was independently associated with subsequent ischemic stroke1). It was associated with a 10.2-, 4.6-, and 2.3-fold increased risk of subsequent stroke during 3 months, 1 year, and 5 years of follow-up, respectively3). The risk of stroke among patients with skull fracture was more pronounced than among patients without skull fracture, both compared with those in the comparison cohort3). In addition, the risk of subarachnoid hemorrhage and intracerebral hemorrhage increased more considerably in patients with TBI, compared with individuals unaffected by TBI. The mechanism by which a TBI may influence the incidence of stroke is still vague. Yet, several possibilities such as direct damage to the vessels, clot formation at the site of injury and other parts of the head, or loosening of clots from an atherosclerotic blood vessel, could help explain the link between TBI and stroke3). Even in the aged victims, trauma can evoke platelet aggregation, which result CI. Although we cannot ignore the role of trauma in the aged, the apportionment of trauma will be more important in the young patients than in the aged patients. Traditionally, lacune infarctions were considered as spontaneous infarctions, since the 2 most common causes of them are atherosclerosis and lipohyalinosis in the adult population. However, ischemia of the basal ganglia may result from stretching or vasospasm of perforating arteries as an immediate consequence of minor head trauma in children and young adult10,21).
The interval from injury to CI can be an important clue to presume the apportionment of the trauma. Traumatic CI developed early in the clinical course (median 8.7 days, range 1-59 days), usually within 2 weeks after the injury17). It appeared within the first week in 31%, 8 days to 2 weeks in 43%, 2 to 3 weeks in 14%, 3 weeks to 1 month in 7%, and 1 to 3 months in 5%17). In pediatric ages, most (26/29) of the patients developed the neurological symptoms and signs within 72 hours after trauma, 51.7% within 30 minutes19). The risk of CI after TBI is highest within the first week, then rapidly diminished. Although TBI was independently associated with a 2.3-fold increased risk of subsequent stroke during up to 5 years of follow up3), the probability of causation would be decrease with time.
The severity of the TBI was also an important component of TAS. The occurrence of traumatic CI was significant correlated to low systolic BP, brain herniation, admission GCS, and decompressive craniectomy6,17). Infarction was primarily due to gross mass effects producing transfalcine and/or transtentorial herniation and occurred in a wide variety of vascular territories12). Brain herniations are more common in severe TBIs. The probability of CIs after mild TBIs will be very lower than CIs after severe TBIs. Anyway, TAS with these three items was not so useful.
Adding three items more, such as systemic illness, bad health habits, and doctor's opinion, rTAS was proposed. For ischemic stroke, nine risk factors, such as hypertension, smoking, abdominal obesity, diet, physical activity, diabetes mellitus, alcohol intake, psychosocial factors, and apolipoproteins, accounted for about 90% of the population-attributable risk13). Hypertension, diabetes, and cardiac disorders were present in 47%, 16%, and 8% of patients with CI in Korea, respectively4). We selected two most common disorders, hypertension and diabetes, as a component of the rTAS.
As bad health habits, smoking and drinking were added. Traditional risk factors for stroke such as hypertension and diabetes are not very frequent in young adults5). However, current smoking, and long-term heavy alcohol consumption are major risk factors for stroke in young adults, along with diabetes, hypertension, and heart disease20). Of course, there are some other permanent or transient risk factors such as oral contraceptives, migraine, use of illicit drugs, and pregnancy or puerperium5). We should consider all these risk factors along with any evidences of traumatic brain injury to determine the causation. However, it was hard to reflect all these factors to the scoring system.
Finally, doctor's opinion was added to the rTAS. The role of trauma cannot be fully assessed by the five components of the rTAS. There may be a direct evidence of trauma or sufficient evidences of spontaneous origin. The doctor may influence on the score, by careful considerations on the all other components related to the causation of the CI.
The interval and GCS scores were artificially supposed as 3 (within 7 days) and 1 (GCS 13-15) to simulate obscure CIs. If the interval was longer than 7 days, the rTAS would be low, which means the possibility of traumatic CI would be decrease. In this condition, differentiation of traumatic CIs from spontaneous CIs will be easy. Severe head injury may cause traumatic CIs. If the GCS was low (≤8), the rTAS will increase 2 points. Although differentiation of traumatic CIs from spontaneous CIs will be obscure, actually the possibility of traumatic CI would be increase. Traumatic origin would be accepted in severe head injuries. In practice, argument on the causation is more common in mild head injuries. In all patients with spontaneous CI, the TAS was 4 or 5. Although the interval and GCS scores were again supposed as 3 and 1, the rTAS was not more than 11 in more than 70% of the spontaneous CI. Compared to TAS, rTAS definitely enhanced the discriminating ability. However, there were still significant overlapping areas. When the doctor thought the causation was obscure, even in spontaneous CIs, the rTAS reached up to 13 in 3 patients, which implied trauma apportionment rate as 41-60%. Although the rTAS may enhance the reliability, it should be used with cautions. Final decision should not be made by the rTAS alone. Expert witness should provide probability based on the scientific facts and data.
References
1. Burke JF, Stulc JL, Skolarus LE, Sears ED, Zahuranec DB, Morgenstern LB. Traumatic brain injury may be an independent risk factor for stroke. Neurology. 2013; 81:33–39. PMID: 23803315.

2. Chen H, Xue LX, Guo Y, Chen SW, Wang G, Cao HL, et al. The influence of hemocoagulation disorders on the development of posttraumatic cerebral infarction and outcome in patients with moderate or severe head trauma. Biomed Res Int. 2013; 2013:685174. PMID: 23984395.

3. Chen YH, Kang JH, Lin HC. Patients with traumatic brain injury : population-based study suggests increased risk of stroke. Stroke. 2011; 42:2733–2739. PMID: 21799162.
4. Korean Neurological Association. Epidemiology of cerebrovascular disease in Korea : a Collaborative Study, 1989-1990. J Korean Med Sci. 1993; 8:281–289. PMID: 8198765.
5. Ferro JM, Massaro AR, Mas JL. Aetiological diagnosis of ischaemic stroke in young adults. Lancet Neurol. 2010; 9:1085–1096. PMID: 20965437.

6. Ham HY, Lee JK, Jang JW, Seo BR, Kim JH, Choi JW. Post-traumatic cerebral infarction : outcome after decompressive hemicraniectomy for the treatment of traumatic brain injury. J Korean Neurosurg Soc. 2011; 50:370–376. PMID: 22200021.

7. Hart RG, Miller VT. Cerebral infarction in young adults : a practical approach. Stroke. 1983; 14:110–114. PMID: 6337424.

8. Janssen AW, de Leeuw FE, Janssen MC. Risk factors for ischemic stroke and transient ischemic attack in patients under age 50. J Thromb Thrombolysis. 2011; 31:85–91. PMID: 20532956.

9. Jo GR, Kim KH. Traumatic carotid artery thrombosis : an autopsy case. Korean J Leg Med. 2001; 25:48–52.
10. Landi A, Marotta N, Mancarella C, Marruzzo D, Salvati M, Delfini R. Basal ganglia stroke due to mild head trauma in pediatric age-clinical and therapeutic management : a case report and 10 year literature review. Ital J Pediatr. 2011; 37:2. PMID: 21210991.

11. Lee KS, Chang JC, Jung DS, Jung JH, Hwang SC. Medical considerations in reparation and compensation. ed 5. Seoul: ML Communication;2011. p. 95–134.
12. Mirvis SE, Wolf AL, Numaguchi Y, Corradino G, Joslyn JN. Posttraumatic cerebral infarction diagnosed by CT : prevalence, origin, and outcome. AJR Am J Roentgenol. 1990; 154:1293–1298. PMID: 2110744.

13. O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study) : a case-control study. Lancet. 2010; 376:112–123. PMID: 20561675.
14. Server A, Dullerud R, Haakonsen M, Nakstad PH, Johnsen UL, Magnaes B. Post-traumatic cerebral infarction. Neuroimaging findings, etiology and outcome. Acta Radiol. 2001; 42:254–260. PMID: 11350282.

15. Suh BS, Lee JS, Hwang GC, Lee SJ, Park HI. A case of traumatic cerebral infarction due to injury of the petrosal internal carotid artery resulting from head trauma. J Korean Neurosurg Soc. 1998; 27:114–117.
16. Tawil I, Stein DM, Mirvis SE, Scalea TM. Posttraumatic cerebral infarction : incidence, outcome, and risk factors. J Trauma. 2008; 64:849–853. PMID: 18404047.
17. Tian HL, Geng Z, Cui YH, Hu J, Xu T, Cao HL, et al. Risk factors for posttraumatic cerebral infarction in patients with moderate or severe head trauma. Neurosurg Rev. 2008; 31:431–436. discussion 436-437. PMID: 18704527.

18. Windeløv NA, Sørensen AM, Perner A, Wanscher M, Larsen CF, Ostrowski SR, et al. Platelet aggregation following trauma : a prospective study. Blood Coagul Fibrinolysis. 2014; 25:67–73. PMID: 23945060.
19. Yang FH, Wang H, Zhang JM, Liang HY. Clinical features and risk factors of cerebral infarction after mild head trauma under 18 months of age. Pediatr Neurol. 2013; 48:220–226. PMID: 23419473.

20. You RX, McNeil JJ, O'Malley HM, Davis SM, Thrift AG, Donnan GA. Risk factors for stroke due to cerebral infarction in young adults. Stroke. 1997; 28:1913–1918. PMID: 9341695.

21. Zwank MD, Dummer BW, Danielson LT, Haake BC. Lacunar stroke in a teenager after minor head trauma : case report and literature review. J Child Neurol. 2014; 29:NP65–NP68. PMID: 24072020.
Table 2
Revised trauma apportionment score (rTAS) for cerebral infarction
rTAS=sum of 6 scores; rTAS -8=trauma apportionment rate 0%; rTAS 9-10=trauma apportionment rate 1-20%; rTAS 11-12=trauma apportionment rate 21-40%; rTAS 13-14=trauma apportionment rate 41-60%; rTAS 15-16=trauma apportionment rate 61-80%; rTAS 17-18=trauma apportionment rate 81-100%. GCS : Glasgow coma score




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download