INTRODUCTION
Studying the development of the pediatric cervical spine is very challenging for several different reasons. Firstly, the pediatric cervical spine is widely variable between individuals due to the ossification process and synchondroses, which make deciding on the most accurate anatomic features to measure very difficult for physicians. Additionally, morphological changes in the cervical spine may not be consistent in all pediatric populations according to age, gender or ethnicity. Moreover, physicians should consider the growing potency of the pediatric cervical spine whenever pathological conditions are encountered. Therefore, a more comprehensive understanding of the cervical spine during early childhood would provide physicians with better tools to properly deal with pediatric spinal diseases. However, documentation of the normal variation and the timing of developmental changes of the pediatric cervical spine is very limited.
Developmental morphologic changes of the superior cervical spine (atlas and axis), and the ossification patterns of the pediatric spine are relatively well understood. However, the growth pattern of the middle and lower cervical spine has not been well explained, especially with regard to the vertebral body and spinal canal dimensions. Thus, the acquisition of data explaining cervical spine development will provide better opportunity to cope with congenital or developmental spinal diseases, such as mucopolysaccharidosis type IVA (Morquio A syndrome).
To provide normal values of the growth pattern of the pediatric cervical spinal canal and vertebral body, the present study used computed tomography (CT) scans of the cervical spine with 318 normal young children ranging in age from infants to 10 years old.
MATERIALS AND METHODS
Three hundred eighteen CT scans of the neck or cervical spine were available for study, 190 of which were from boys and 128 from girls. All patients were younger than 10 years of age at the time of admission during the 8-year study period (April 2006 to October 2013). All patients underwent a CT evaluation for other reasons (e.g., minor trauma : 17 cases or otorhinolaryngological problems : 301 cases). The average age of the patient group was 60.7±30.8 months (range : 1-119 months). Patients with bony or ligament injury, deformity, intraosseous pathology, or congenital anomalies were excluded. All CT scans were performed on a 64-slice CT scanner with 1.5-mm or 2-mm sagittal image thickness (Siemens Medical Solutions, Erlangen, Germany) and measurements were made using m-view 5.4 software (Marosis Technologies, Inc., Seoul, Korea).
The cohorts were divided into four age groups as follows : infancy (I) (zero to two years), very early (VE) childhood (older than two years to five years), early (E) childhood (older than five years to eight years), and childhood (C) (older than eight years). In addition, to assess size and growth patterns of individual patients, the weight for age percentile growth chart for Korean pediatrics population was used. Pediatric patients were classified into an abnormal-weight (low or over-weight) group and normal-weight group (cutoff value for normal-weight group was between 10 and 90 percentile) in all age groups. Not all patients had measured their body weight on the day of cervical CT evaluation (1 case : I group, 4 cases : VE group, 8 cases : E group, and 4 cases : C group), so 301 cases were confirmed with an electrical medical chart review. The local research ethics committee waived the need for formal ethics approval for this retrospective study.
Measurements
For measurements of the vertebral body height and antero-posterior (AP) diameter of the sub-axial spine (C3-7), the mid-body was used as the reference (
Fig. 1). Vertebral body height 2015(VBH) and vertebral body AP diameter (VBAP) was measured in the mid-vertebral level. Spinal canal AP diameter (SCAP) was measured as the distance between the middle of the posterior margin of the vertebral body to a line parallel to the posterior margin of the vertebral body and tangential to the base of the spinous process. The Torg ratio (TR) was calculated by dividing the SCAP by the vertebral body AP diameter. All patients were classified into a low TR group and a high TR group according to a cutoff value of 1.0. To account for spinal curvature, the C3-7 angle (in degrees) was measured. The C3-7 angles were measured using Cobb's method between the inferior line of the C3 body and the inferior margin of the C7 body. To assess the effects of spinal curvature on the spinal canal space, pediatric patients were classified into groups as follows : 1) kyphosis group (less than -2° of curvature), 2) neutral group (from -2° to 18°), and 3) lordosis group (more than 18° of curvature). In addition, to assess the effects of spinal curvature by the traumatic event, all cohorts were classified into traumatic group (n= 17 cases) and non-traumatic group (n=301 cases).
Statistical analysis
The data were analyzed according to gender and according to age (I, VE, E, and C). Scheffe's multiple comparison tests were used to compare the statistical significance between the I, VE, E, and C age groups. Analysis of variances, chi-square tests, unpaired t-tests, contrast tests (orthogonal polynomial) and Pearson correlation coefficient tests were performed using the SAS (System for Windows Version 9.3). Statistical significance was set at p<0.05.
RESULTS
There were 45 cases (14.2%) included in the I group and 120 cases (37.7%) included in the VE group. The E group included 100 cases (31.4%), and 53 cases (16.7%) were included in the C group. The mean ages of the I, VE, and E groups were 14.1±5.9 months, 44.4±10.1 months, and 78.3±9.7 months, respectively. The mean age of the C group was 107.4±7 months. The mean value of VBH/VBAP/SCAP were 6.8/11.8/12 mm at C3, 7/11.8/ 11.9 mm at C4, 7.1/11.9/12.3 mm at C5, 7.2/12.3/12.6 mm at C6, and 8.1/12.6/12.8 mm at the C7 vertebral level in all 318 cases. Seven patients were included as the abnormal-weight group (15.6%) in the I group, and 19 patients (15.8%) were included as the abnormal-weight group in the VE group. Seventeen (17%) and 8 cases (15.1%) were included as the abnormal-weight group in the E and C group, respectively. The distribution of normal weight population was almost even among the four age groups (p>0.05).
Table 1 showed the measured value of VBH, VBAP, and SCAP according to the age groups. The VBH dimensions continuously increased with age, irrespective of vertebral level. The mean value of VBH ranged from 5.4 mm (C3, I group) to 9.8 mm (C7, C group) and the difference value between the adjacent age groups was relatively even (range, 0.8-1.2 mm). The VBH dimensions gradually increased from the C3 to the C7 level irrespective of age group (
p<0.0001) and the growth of C7 VBH was slightly larger than other sub-axial spines (3.2 mm). The mean value of VBAP ranged from 9.9 mm (C3, I group) to 14.3 mm (C7, C group). The VBAP dimensions also continuously increased with age, irrespective of vertebral level. Boys had larger VBAP values than girls at every cervical level (
p<0.001). The mean VBAP value also gradually grew from the C3 to the C7 level, irrespective age group (
p<0.0001). The SCAP dimensions gradually increased from the C3 to the C7 level, similar to the dimensions of the vertebral body. The narrowest region of the canal was the C3 level (E group) or the C4 level (I, VE, and C group) in the four different age groups, according to our results. The broadest region of the canal was at the C7 level, irrespective of age group. The mean SCAP value ranged from 10.6 mm (C4, I group) to 13.3 mm (C7, C group), and considerable expansion of the canal happened during the very early period (between the I and VE groups, range : 0.9-1.3 mm).
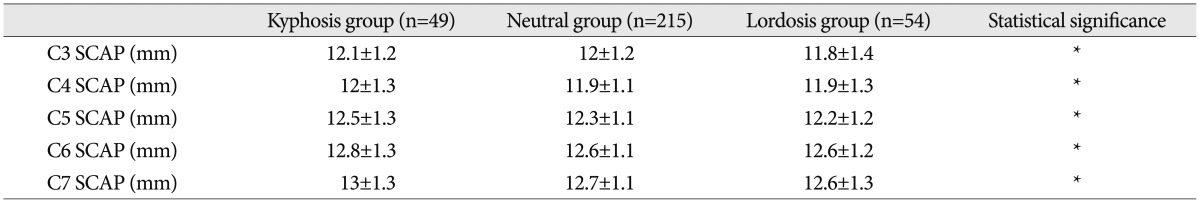
The mean sub-axial angle (C3-7) was 7.9±10.6° (range : -17-47°). Statistically significant differences in the SCAP were not found between the three spinal curvature groups at any spinal level (
Table 2). Moreover, traumatic event did not influence the spinal curvature in our study (traumatic group : 8.4°, non-traumatic group : 7.8°,
p>0.05). The mean TR values were 1.03±0.14 at the C3 vertebral level, 1.02±0.13 at C4, 1.05±0.13 at C5, 1.04±0.13 at C6, and 1.02±0.12 at C7 in all patients. The variation between levels was not statistically significant. Notably, a smaller number of cohorts were classified as being part of the low TR group at the C5 and C6 level than at other spinal levels (C3, C4, and C7) (
Table 3). The low TR group had a significantly larger VBH than the high TR group (
p<0.0001). The TR value of the sub-axial spine was larger than 1.02 at all levels (largest C5, smallest C7, statistically insignificant), and the TR value generally decreased with age (
Table 4).
In
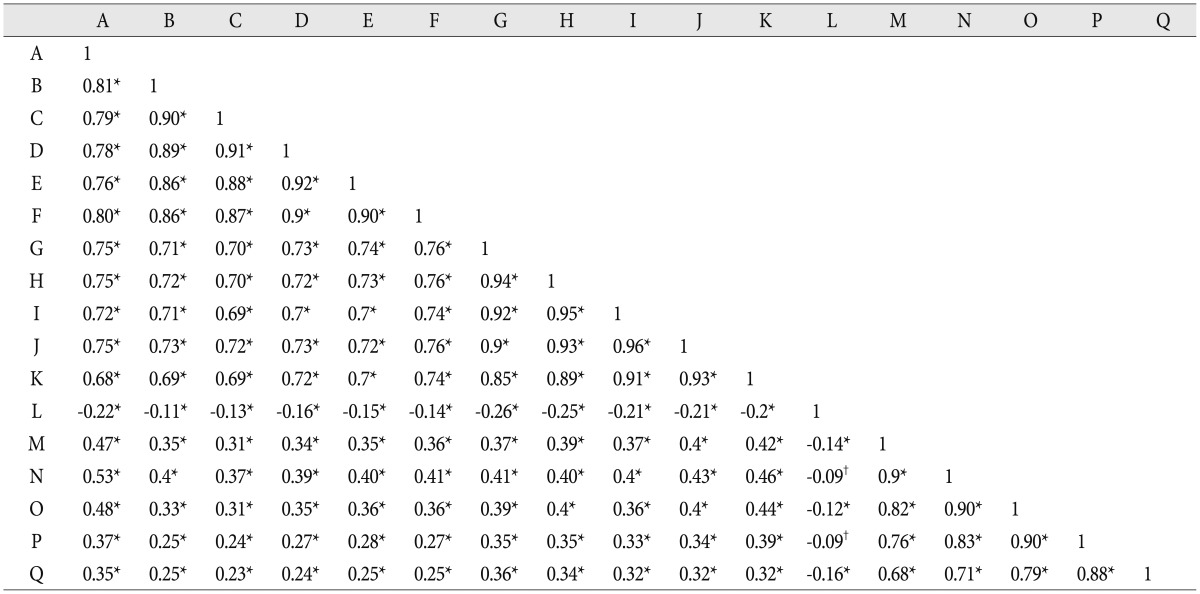
Table 5, the Pearson correlation coefficient scores between the multiple variables in our study are presented. All dimensions related to VBH and VBAP showed a strong correlation to age (r>0.6), irrespective of vertebral level. Additionally, all dimensions associated with SCAP were weakly to moderately correlated to age (r=0.23-0.53), irrespective of vertebral level. Generally, the VBH measure showed a strong correlation to VBAP and was weakly correlated to SCAP. All dimensions related to VBAP were weakly to moderately correlated to SCAP (r=0.32-0.46), according to our results. In addition, the C3-7 angle was negatively correlated to age (r=-0.22).
DISCUSSION
The morphometric analysis of the adult cervical spine has been well described in the literature
5,
9,
22). Although some previous reports addressed the pediatric cervical spine, these reports were almost always confined to the subject of surgical feasibility, and the cohorts studied spanned a very wide age range
1,
10,
16,
19). This current study focuses on cohorts who are younger than 10 years of age and used CT scans to analyze growth patterns. Because spinal growth generally matures by about 8 years of age, we found the under-ten age group to be of particular interest
4,
6,
24).
The middle and lower cervical vertebrae (C3-7) have similar anatomical features, except the 7th vertebra has a long, non-bifid spinous process. To avoid measurement error, we measured VBH from the middle of the vertebral body because the body shape of the sub-axial spine changes with age. Specifically, the spine changes from a wedge shape in younger children to a square shape in older children. Generally, the VBH dimension increased about 2.9 mm (2.7-3.2 mm) through the developmental time frame we measured (from infancy to 10 years of age) at all sub-axial levels. The results presented above show that the VBH of the sub-axial spine contributes much less to the whole-body height than we initially believed (sum of all levels=14.5 mm). The difference between the C3 and C7 vertebrae increased very slightly with age (I group=1.2 mm, VE group=1.3 mm, E group=1.4 mm, and C group=1.5 mm). In addition, VBH growth occurred in a straight fashion, in which considerable changes in VBH were observed, and these changes were relatively even among the four age groups (
Fig. 2). Vertical growth of the sub-axial body was very closely related to vertebral body axial expansion according to the Pearson correlation coefficient scores (r=0.69-0.74). VBH values at sub-axial levels were not statistically different between boys and girls (
p=0.529-0.767), and, in another study of ours, we found similar results between boys and girls at the superior cervical level (occipital and C1 lesions). To conclude, vertical growth of the entire cervical column was not significantly different between boys and girls.
According to our results, the growth of VBAP was slightly larger than the growth of VBH (about 3.4 mm). The mean difference between the C3 and C7 levels decreased slightly with age (1.1 mm : I group, 0.9 mm : VE group, 0.8 mm : E group, and 0.8 mm : C group). Contrary to VBH results, the VBAP dimension in boys was larger than that in girls, and similar results were also reported in adults and children alike
11,
16). The VBAP dimensions were increased approximately 3.4 mm (3.2-3.6 mm) throughout the age groups (from infancy to 10 years) at all sub-axial levels. According to several reports, vertebral body axial growth may continue steadily, and the difference between spinal levels will be reduced
11,
13,
16). Comparing our results to other reports (diagnostic techniques in a report by Kasai et al.
11) were most similar to the present study), our mean VBAP value was larger than what was found in the other study. Such results can be explained by the different ethnic makeup of the study population or by differences in body build due to the age ranges studied. VBAP growth occurred as the reversed-W type, in which considerable changes in VBAP were minimized between the VE and the E groups.
Previously, many reports have described normal and abnormal SCAP values from lateral radiographs, CT scans and MRI
8,
14,
16,
20,
21,
23). However, these reports were restricted to the adult population or had a small number of pediatric patients.
According to Sasaki et al.
20), the pattern of change in SCAP on lateral radiographs can be divided into four categories : the straight type, in which SCAP decreased gradually from C1 to C7, the V type, in which the SCAP was minimized at the middle cervical level, the W type, in which the SCAP was minimized at two cervical levels, and all other types. Moreover, some reports showed that other SCAP types change in the adult population (lowest at C7, but relatively constant from C3 to C6 or reversed-funnel shape from C1 to C6)
15,
20,
23). The SCAP dimension increased from C3 to C7 in the present study, irrespective of age. Therefore, the pattern of change in the SCAP was most similar to the straight type in young children. The differences in SCAP between the smallest and largest cervical vertebrae continuously decreased with age (I group=1.1 mm, VE group=1.1 mm, E group=0.8 mm, C group=0.6 mm). The SCAP increments at each cervical level were about 1.8 mm (range : 1.6-2.1 mm) from the infant stage through the pediatric stage (less than 10 years). Canal expansion in the middle upper cervical vertebrae (C3, 4) continuously increased after 8 years of age, but the SCAP in the lower cervical vertebrae (C5, 6, and 7) reached its peak growth at a younger age (>5 years old) (
Table 1). When assessing the relationship between VBH and VBAP, the Pearson correlation scores showed that the canal expansion was less intimately associated with the dimension of the vertebral body (VBH and VBAP). Similar to VBAP dimensions, the spinal canal measurement in boys was also larger than in girls at all sub-axial spinal levels, which may induce a non-significant difference between boys and girls in the TR value.
In patients undergoing surgery for symptomatic myelopathy in the adult population, some previous data showed that the mean SCAP value was 12.8 mm
12). Another cutoff value for symptomatic myelopathy was reported by Penning
18), who emphasized that dynamic canal stenosis induced by backward slippage of the upper body segment upon extension was less than 12 mm (a jaw diameter). When we consider these reports, children in the C group (>8 years) had canal space measurements that were close to what is measured in adults. Generally, SCAP values are closely related to the height of the entire build of the body. Therefore, younger generations of Koreans may have a wider spinal canal space than the older generation when they are full-grown
7,
23).
Prior to beginning this study, we expected that cervical curvature may contribute to changes in SCAP. Although the lordosis group had a narrower SCAP than the neutral and kyphosis groups, there were no statistically significant differences between the three curvature groups. Some contributing factors may explain our results more fully. Firstly, CT-base images showed only bony anatomy and excluded any soft tissue bulking effects (posterior longitudinal ligament or ligamentum flavum). Secondly, a jaw diameter method was not used in our study. If we adopted a jaw diameter method, the SCAP value may have been inaccurate when analyzing the present results. Notably, a considerable number of patients were included in the neutral curvature group (n=215, 67.6%). It is common for there to be absent lordosis of the lateral cervical spine when the neck is held in the neutral position in children up to age 16
2,
3). Cervical spinal curvature, as assessed from CT scans (supine position), did not directly contribute to dynamic change in the spinal canal in pediatric patients.
The ratio of the sagittal diameter of the cervical canal to that of vertebral body was first proposed by Pavlov et al.
17) as an indicator of the degree of developmental canal narrowing. Though Lim and Wong
13) insisted that TR is not a consistent and reliable method to confirm cervical canal stenosis, a TR less than 0.80 has generally been known to be a strong predictor for the induction of symptomatic change in the adult population
17). No significant changes in the TR were found at any point from infancy to early childhood in the present study. Rather, dynamic changes in the TR were observed to occur after 8 years of age, according to statistical analyses at the C4, C6, and C7 spinal levels. Of note, the low TR group showed larger VBH dimensions than the high TR group. As previously mentioned, the VBAP dimension showed a strong correlation to the VBH dimension, which explains the above results.
Limitation and interpretation
Although CT-based studies have some advantages in their ability to precisely depict bony anatomy, CT imaging is not sufficient to assess soft tissue effects in the spinal canal. This study is retrospective with a cross-sectional cohort approach, which limits our ability to determine actual time-related development for any one individual. If we add the whole-body height of cohorts, the results of the spinal body and canal space data may be influenced. In addition, this study was performed with a relatively large number of pediatric patients, focusing more on the younger age group than other reports have in the past.







 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download