Abstract
Objective
For improving the drawbacks of previous thoracolumbar spine trauma classification, the Spine Trauma Study Group was developed new classification, Thoracolumbar Injury Classification and Severity Score (TLICS). The simplicity of this scoring system makes it useful clinical application. However, considering criteria of Korean Health Insurance Review and Assessment Service (HIRA), the usefulness of TLICS system is still controversial in the treatment decision of thoracolumbar spine injury.
Methods
Total 100 patients, who admitted to our hospital due to acute traumatic thoracolumbar injury, were enrolled. In 45, surgical treatment was performed and surgical treatment was decided following the criteria of HIRA in all patients. With assessing of TLICS score and Denis's classification, the treatment guidelines of TLICS and Denis's classification were applied to the criteria of Korean HIRA.
Results
According to the Denis's three-column spine system, numbers of patients with 2 or 3 column injuries were 94. Only 45 of 94 patients (47.9%) with middle column injury fulfilled the criteria of HIRA. According to TLICS system, operation required fractures (score>4) were 31 and all patients except one fulfilled the criteria of HIRA. Conservative treatment required fractures (score<4) were 52 and borderline fracture (score=4) were 17.
Conclusion
The TLICS system is very useful system for decision of surgical indication in acute traumatic thoracolumbar injury. However, the decision of treatment in TLICS score 4 should be carefully considered. Furthermore, definite criteria of posterior ligamentous complex (PLC) injury may be necessary because the differentiation of PLC injury between TLICS score 2 and 3 is very difficult.
The management of traumatic thoracolumbar spinal fractures remains controversial. Many classification systems have been developed to guide clinical management and strategy of surgical treatment about thoracolumbar spinal trauma. Several classification systems have been proposed, the most commonly used is the Denis's classification, based on the "three-column concept"1). Recently, the Vaccaro et al.13) proposed a new classification system, which is based on the three most important injury characteristics : radiographic morphology of injury, integrity of the posterior ligamentous complex (PLC), and neurological status of the patient5). The Thoracolumbar Injury Classification and Severity Score (TLICS) can guide surgical decision-making in managing thoracolumbar spinal trauma. The simplicity of this scoring system makes it useful clinical application.
Although reliability and validity of the TLICS system have been suggested2,3,4,10,11,12), but considering through the boundaries of our governing disciplines, such that criteria of Korean Health Insurance Review and Assessment Service (HIRA), the usefulness of TLICS system is still controversial in the treatment decision of thoracolumbar injury. It is important therefore that new classification is reliable for both spine surgeons and governmental policy to reduce treatment variability in an already controversial treatment territory. Therefore, the purpose of our study was asses the applicability of TLICS system to criteria of Korean HIRA in treatment decision of thoracolumbar injury.
A retrospective review was performed to identify conservatively and surgically managed patients with acute thoracolumbar spine trauma. All patients were treated between 2010 and 2013 in our institute. Before the consequently management, all case descriptions were prepared, including age and gender, the mechanism of injury, level of fracture, preoperative neurologic status and radiographic studies consisting plane films, a computed tomography and sagittal T2 magnetic resonance images of thoracolumbar spine. The neurologic status was classified using the American Spinal Injury Association (ASIA) classification. Using available radiographic studies, injuries were classified according to both the Denis's classification and the TLICS system at the most severely damaged level of thoracolumbar spine.
The TLICS system is based on a numerical score for each of the three specific categories : 1) injury morphology, 2) neurologic involvement, and 3) integrity of the PLC (Table 1). Furthermore the assigned points are calculated by summing the individual scores and a management recommendation for nonoperative treatment is given for injuries scoring 3 or fewer points and operative for those with 5 or more points. Injuries scoring 4 points are intermediate and can be managed either way.
Inclusion criteria included adult patients (age≥18), thoracolumbar spine trauma (from T1 to L5), and complete clinical and radiographic date. Exclusion criteria included inadequate clinical and radiographic data, patients with pathologic fractures (cancer or infection), simple transverse or spinous process fractures, and chronic thoracolumbar spine injuries.
Our guideline for surgical treatment of patients with thoracolumbar spine injuries in accordance with Korean HIRA, included the following criteria : 1) 3 column injury, 2) burst fracture with kyphotic angle 30°> or height loss 40%> or spinal canal encroachment 50%>, 3) injury of PLC, 4) neurologic damage with muscle weakness, and 5) despite appropriate conservative treatment, severe pain occurs or neurologic symptoms with further kyphotic change (Table 2).
Clinical and radiographic results of treatment were recorded such as postoperative neurologic status, surgical approach, number of fixation levels and complications.
There were 100 patients diagnosed and treated as having thoracolumbar spine trauma during the study period. Patient's age ranged from 18 to 101 years (mean age of 55.9). Fifty-four patients were male and forty-six were female. Slipped down and fall from height were the main injury mechanism of our study (64%) followed by motor vehicle collisions (26%). Sixty-four patients had thoracolumbar spine fracture (T11-L2), 24 thoracic (T1-10), and 12 in lumbar spine fracture. Fifty-one patients had vertebral body burst fractures, 41 had compression fractures, and 8 had fracture with dislocations or subluxations.
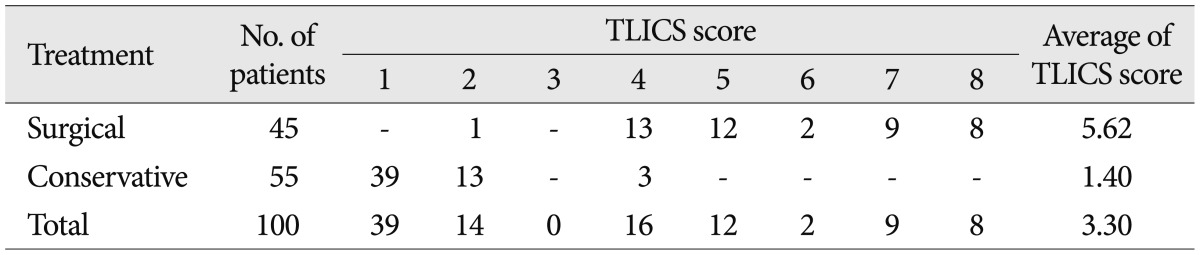
Fifty-five patients were initially treated conservatively method and 45 were surgically treated (according to criteria of Korean HIRA). All of conservatively treated patients were neurologically intact at diagnosed time and maintained their neurologic status after nonsurgical treatment (from ASIA E to E). Fracture classification according to the Denis classification system included 6 patients with 1 column injury, 46 patients with 2 columns, and 36 patients with 3 columns injuries. A statistically association was not found using the chi-square between the surgical criteria of Korean HIRA and middle vertebral column injury (p=0.22) (Table 3). The TLICS score ranged from 1 to 4 in non-surgically treated group, all of these patients management corresponded with the TLICS recommended guideline (TLICS score≤4) (Table 4).
In surgically treated group, all patients were operated through a posterior approach and a transpedicular posterolateral fixation was performed. Two patients (4.4%) underwent an anterior decompression and interbody fusion with posterior fixation. Preoperatively, 9 (20%) were ASIA A, 2 (4.4%) were ASIA B, 2 (4.4%) were ASIA C, 9 (20%) were ASIA D, and 23 (51.1%) were ASIA E. Preoperatively, 8 patients improved in ASIA score, fortunately any patient had not neurological deterioration. Complications related to surgery included 3 patients with wound infections, 1 of a them required revision surgery for debridement of infectious tissue without elimination of instruments.
Fracture classification according to the TLICS system, all cases had a TLICS score of 4 or more (mean score of 5.62) (Table 4), except 1 patient with burst fracture without neurological deficit (TLICS score of 2) was treated surgical method because of progressive kyphotic change with severe back pain (Fig. 1).
Radiographic study and physical examination revealed the all of these cases a statistically significant association was found between the surgical criteria of Korean HIRA with intact of PLC (p< 0.05) and absence of neurological deficit (p<0.05).
A classification of thoracolumbar spine injuries is necessary in order to develop to unify the language for understand of traumatic mechanism and suggest treatment guideline. Several classifications of thoracolumbar spine injuries have been proposed based on fracture anatomy and different stability concepts, the most frequently used is the Denis classification system1,6,7,8,9). The middle column became a most important part of the classification of spinal injuries according to Denis, therefore a significant injury to the middle column was the fundamental principle for define of instability. Denis underlined that 3 column theory is consisted by bony and ligamentous structures, however he did not make to further the diagnosis of ligamentous injuries and evaluate about unstable fractures.
To supplement these shortcomings, some authors to make public various hypotheses and classification, McAfee et al.7) described the instability of the burst fracture were summarized as follows : 1) progressive neurologic deficit, 2) posterior element disruption, 3) kyphosis progressing 20° or more, 4) greater than 50% of vertebral body height with facet joint subluxation, and 5) free bony fragments within a compromised spinal canal. According to several classifications, most surgeons agree that neurological status, spinal stability, deformity of the injured lesion, degree of canal compromise, and associated general problems are the most significant factors that need to be considered when deciding on operative or non-operative treatment for patients with a thoracolumbar spine fracture 2,4,10).
Thus, in spite of a large number of classification systems accounted for thoracolumbar spine injuries, there is still no classification system that has fulfilled general acknowledge and clinical usefulness. Recently, the TLICS system described by Vaccaro et al.5,13) were created to address the shortcomings that have frustrated these systems. The brevity of TLICS system makes it helpful clinical utilization. Furthermore, the TLICS can be calculated and patients are then divided into surgical and conservative treatments.
To assemble advantages of many classifications that above-mentioned 1,5,7,13), the HIRA, organization under the Government of the Republic of Korea proposed new surgical criteria of thoracolumbar spine injuries. This criteria conforms to the traditional indications for surgical treatment, such as incomplete paraparesis, progressive neurological deficit, spinal cord compression without neurological deficit, fracture dislocation, severe segmental kyphosis (>30°) and predominant ligamentous injuries.
Most Korean surgeons agree on absolute indications for surgery and criteria of HIRA whereas indications by TLICS system are still debatable. One of the important point raised about this study is that to determine the presence of PLC injuries. Vaccaro et al.13) has been suggested that assessment of PLC integrity can be made from plain film, CT, and MR images. In addition, it is typically indicated by splaying of the spinous processes, diastasis of the facet joints, and facet perch or subluxation. However, radiologic picture and physiologic findings of some cases were indistinguishable from that of categorized as intact, indeterminate, or disrupted. Therefore, we cannot deny the fact that, the integrity of PLC was scored a little bit of subjectively. Therefore definite criteria of PLC injury may be necessary because the differentiation of PLC injury between TLICS score 0, 2, and 3 is very difficult.
Another sticking point was that treatment strategy of patients with total TLICS score of 4 was unclear. A score of 4 points remains an ambiguous zone where either surgical or conservative management may be applied according to other variables, such as a patient's age, comorbidities, physical status, and patient or surgeon's individual preference. However the TLICS system is designed only as a guideline for surgeons and non surgeons to help determine possible treatment options; it is not meant to be an absolute end-all in decision-making12,13). To decide the management of thoracolumbar spine injuries, it is important to appreciate the other various factors.
This study demonstrates the clinical application of the TLICS system. TLICS system is easily applied and have been shown to matched prior criteria of surgical management. TLICS system is very useful system for decision of surgical indication in acute traumatic thoracolumbar spine injury and may be very reasonable in Korean HIRA system in most cases. However, there remain a number of problems which need to be solved, such as the decision of treatment in TLICS score 4, it should carefully considered. The presence of ligament damage and it is also necessary to observe very closely. Furthermore the damage of PLC damage of the PLC should be closely observed.
References
1. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 817–831. PMID: 6670016.

2. Joaquim AF, Daubs MD, Lawrence BD, Brodke DS, Cendes F, Tedeschi H, et al. Retrospective evaluation of the validity of the Thoracolumbar Injury Classification System in 458 consecutively treated patients. Spine J. 2013; 13:1760–1765. PMID: 23602328.

3. Joaquim AF, Fernandes YB, Cavalcante RA, Fragoso RM, Honorato DC, Patel AA. Evaluation of the thoracolumbar injury classification system in thoracic and lumbar spinal trauma. Spine (Phila Pa 1976). 2011; 36:33–36. PMID: 20479700.

4. Joaquim AF, Ghizoni E, Tedeschi H, Batista UC, Patel AA. Clinical results of patients with thoracolumbar spine trauma treated according to the Thoracolumbar Injury Classification and Severity Score. J Neurosurg Spine. 2014; 20:562–567. PMID: 24605999.

5. Lee JY, Vaccaro AR, Lim MR, Oner FC, Hulbert RJ, Hedlund R, et al. Thoracolumbar injury classification and severity score : a new paradigm for the treatment of thoracolumbar spine trauma. J Orthop Sci. 2005; 10:671–675. PMID: 16307197.

6. Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994; 3:184–201. PMID: 7866834.

7. McAfee PC, Yuan HA, Lasda NA. The unstable burst fracture. Spine (Phila Pa 1976). 1982; 7:365–373. PMID: 7135069.

8. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994; 19:1741–1744. PMID: 7973969.

9. Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Joint Surg Br. 1949; 376–394. PMID: 18148776.

10. Patel AA, Vaccaro AR, Albert TJ, Hilibrand AS, Harrop JS, Anderson DG, et al. The adoption of a new classification system : time-dependent variation in interobserver reliability of the thoracolumbar injury severity score classification system. Spine (Phila Pa 1976). 2007; 32:E105–E110. PMID: 17268253.
11. Raja Rampersaud Y, Fisher C, Wilsey J, Arnold P, Anand N, Bono CM, et al. Agreement between orthopedic surgeons and neurosurgeons regarding a new algorithm for the treatment of thoracolumbar injuries : a multicenter reliability study. J Spinal Disord Tech. 2006; 19:477–482. PMID: 17021410.

12. Vaccaro AR, Baron EM, Sanfilippo J, Jacoby S, Steuve J, Grossman E, et al. Reliability of a novel classification system for thoracolumbar injuries : the Thoracolumbar Injury Severity Score. Spine (Phila Pa 1976). 2006; 31(11 Suppl):S62–S69. discussion S104. PMID: 16685239.
13. Vaccaro AR, Lehman RA Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, et al. A new classification of thoracolumbar injuries : the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005; 30:2325–2333. PMID: 16227897.
Fig. 1
Axial CT (A), CT sagittal reconstruction (B), and MR-T2 sagittal (C) showing an T8 burst fracture with lamina fracture in a patient without neurologic deficit. There was no evidence of posterior ligamentous complex (PLC) injury on plain radiographs, CT, or MRI. As a result, this would equal a total Thoracolumbar Injury Classification and Severity Score of 2 (2 points of burst fracture, 0 point of intact neurologic status, 0 of PLC status). We decided to perform surgery because of severe local pain with further kyphotic change and 3 column injured. D and E : The patient underwent posterior T6-10 instrumentation and fusion as seen on plane films. The patient noted back pain improvement and no further kyphotic change after surgical intervention.

Table 1
The Thoracolumbar Injury Classification and Severity Score system*
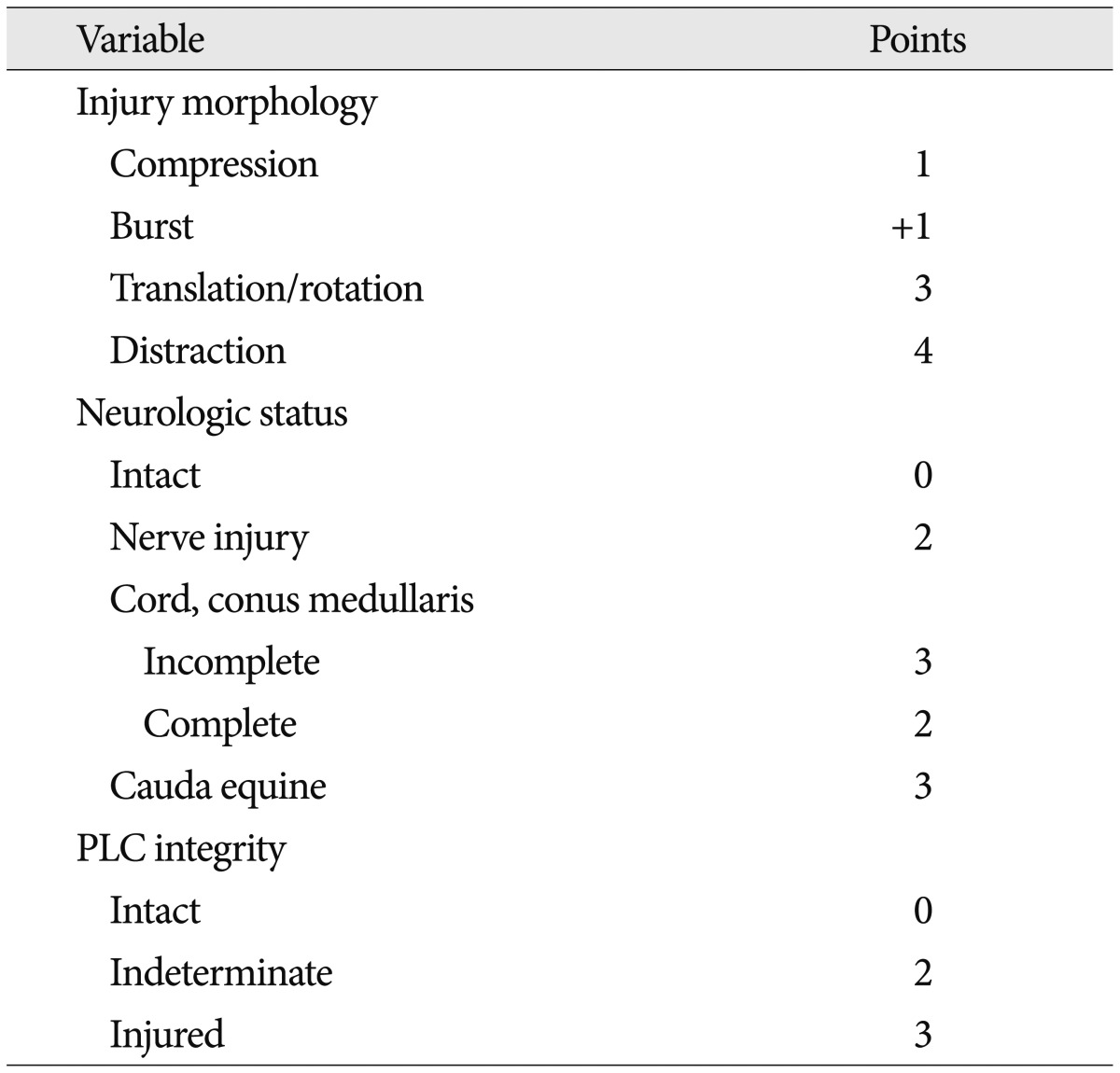
*As reported by Vaccaro et al.5). PLC : posterior ligamentous complex
Table 2
The treatment criteria of patients with thoracolumbar trauma in Korean government based on the Health Insurance Review & Assessment Service*





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download