Abstract
Objective
Venous thromboembolism (VTE) after spinal surgery affects a patients' postoperative recovery and also carries a mortality risk. Some studies recommended chemical prophylaxis for high-risk patients and for those after complex spinal surgeries. However, chemoprophylaxis for VTE in spinal surgery is underemployed and there is no agreement on the use of VTE prophylaxis in spinal surgery. The aim of this study was to document the incidence of VTE after an elective instrumental spinal surgery, among those receiving preoperative chemoprophylaxis as compared with patients who did not receive it.
Methods
This study was carried out on eighty-nine patients allocated randomly to receive either low molecular weight heparin (LMWH) or no prophylaxis before elective instrumental spinal surgery. All patients received postoperative compression stockings. A compression Doppler ultrasonography was performed for all patients to detect postoperative deep vein thrombosis. In addition, further imaging studies were performed for patients suspected of VTE.
Results
Three (3.3%) patients were diagnosed with VTE. One of them had received preoperative chemoprophylaxis. There were no significant difference in incidence of VTE between the two groups (p>0.95; 95% confidence interval, 0.06-8.7). Laterality of gender and postsurgical recumbence duration were all independent predictors of VTE (p=0.01 and p<0.001, respectively).
Conclusion
The difference in the incidence of thromboembolic complications between the two groups was not significant. Moreover, we found that preoperative prophylactic LMWH injection has no major bleeding complications altering postoperative course; still, the issue concerning the initiation time of chemoprophylaxis in spinal surgery remains unclear.
Venus thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is reported as the third most common cause of death in the United States14). According to various studies, the prevalence of VTE in patients who underwent spinal surgery ranges from 0.29% to 31%13,17,18,22) and it depends on the VTE screening method and type of surgery16,18,19). Moreover, these patients are prone to VTE because of several factors, including the clinical setting, prolonged immobility, hospitalization, type of anesthesia used, and methods used for VTE chemoprophylaxis2,13,15,20,22).
Regardless of the fact that various methods are used to prevent VTE following spinal surgery, including mechanical and chemical prophylaxis, the choice of prophylaxis in patients undergoing elective spinal surgeries is still a matter of debate1,2,3,8,9,15). In some studies of chemoprophylaxis, low molecular weight heparin (LMWH) has been used as prophylaxis in decreasing the incidence of DVT in patients after neurological and spinal surgeries7,21). However, as the studies reveal, VTE chemoprophylaxis in spinal surgery is underemployed because of the fear of bleeding complications and spinal epidural hematoma (SEH)3,11,12). Nevertheless, the reported incidence of hemorrhagic disorders and SEH after using chemoprophylaxis is 0-1%4,10). Hence insufficient published data is available to define the safety of chemoprophylaxis; likewise, there is no data about which VTE chemoprophylaxis works best or about the ideal time to begin the use of chemical prevention strategy in patients who undergo spinal surgeries.
The present study aimed to assess the incidence of VTE after an elective instrumental spinal surgery, among those receiving preoperative LMWH prophylaxis in comparison to patients who do not receive it.
A prospective double blind randomized controlled study approved by the institutional review board, was carried out in 2011 with 89 patients, aged between 18 to 75 year old who underwent an elective instrumental spinal surgery by a single neurosurgeon in the authors' center.
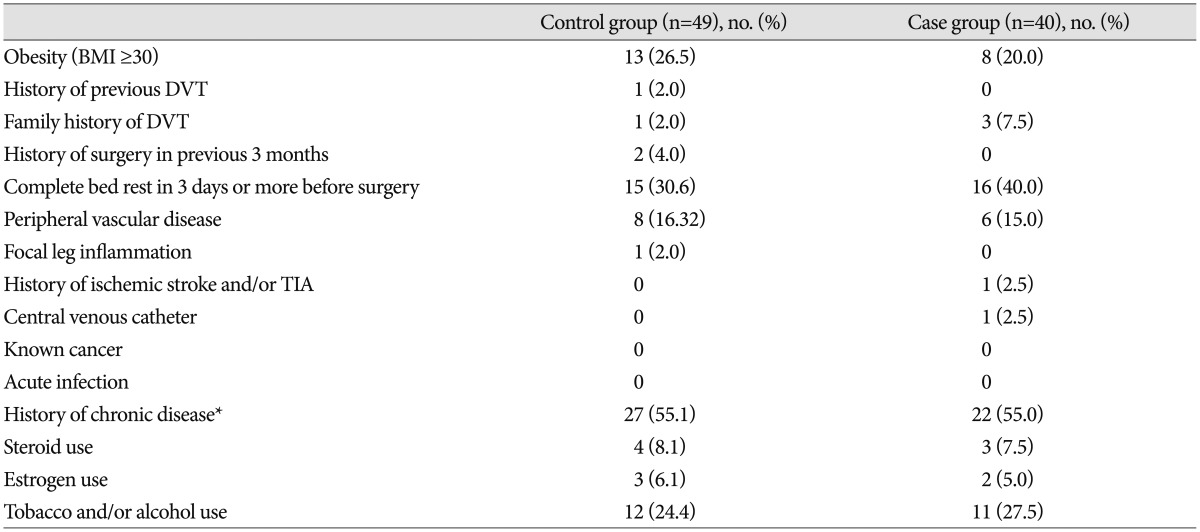
The baseline data, admitting diagnosis and risk factors including history of previous DVT, family history of DVT, history of surgery in the last 3 months, use of central venous catheter, and bed confinement for 3 days or more before surgery were recorded. History of any chronic disease, known malignancy and history of ischemic stroke were collected separately. Patients were excluded before randomization if they had a history of recent active or major bleeding, hemophilia, low platelet count (<100000/mL) or platelet dysfunction, LMWH hypersensitivity, esophageal varices, hepatic impairment, renal insufficiency, uncontrolled hypertension, anemia (Hb<13 g/dL for men, Hb<12 g/dL for women), acute infective endocarditis, active tuberculosis, history of chemotherapy prior to surgery, history of IV drug use, presence of spinal cord injury and history of spinal tumors. All exclusions were documented. Those patients who did not have any exclusion criteria were selected to enter the study before the surgical procedure. Blood samples were drawn for biomarker analysis before and during 72 hours after surgery.
All surgeries were performed under general anesthesia. Level of surgery, types of approach, patient positions, intraoperative transfusion and blood loss were recorded immediately after the operation. Subfascial drains were used for all patients routinely. Then, the number of transfused packed-cell units and drainage blood measurement were also calculated.
Patients were randomly selected to receive either LMWH or not. The case group received one dose per day of subcutaneous LMWH (Enoxaparin, 40 mg/day) within 12 hours before the surgery. All patients received compression stockings as mechanical prophylaxis after the surgery. A daily physical evaluation was performed for early onset acute neurological deficits, symptomatic epidural/wound hematoma and DVT symptoms (evaluated with the Wells score system) during hospitalization. A compression Doppler ultrasonography (CDUS) was performed for all patients. All patients were enrolled in a daily assessment program; calf swelling, pitting edema and daily assessment were used to measure, evaluate and detect early signs and symptoms of SEH and DVT up to two weeks after surgery, then the patients were scheduled for a follow-up eight months after the surgery. All clinical suspicions of a thromboembolic events during this period were documented.
The primary efficacy outcome was a definite or probable symptomatic or asymptomatic DVT detected on a screening CDUS or SEH/PE confirmed by imaging during hospitalization. The secondary outcome measure was defined as symptomatic DVT/SEH detected on screening CDUS or PE confirmed by imaging or autopsy within the follow-up period.
A stepwise logistic regression was performed to identify factors that were predictive of VTE. To assess the efficacy of preoperative chemoprophylaxis on VTE, SEH, and severity of blood loss, the Fisher's exact and Mann-Whitney U tests were performed. The SPSS software version 21 (SPSS Inc., Chicago, IL, USA) was used, and a p value less than 0.05 was considered statistically significant.
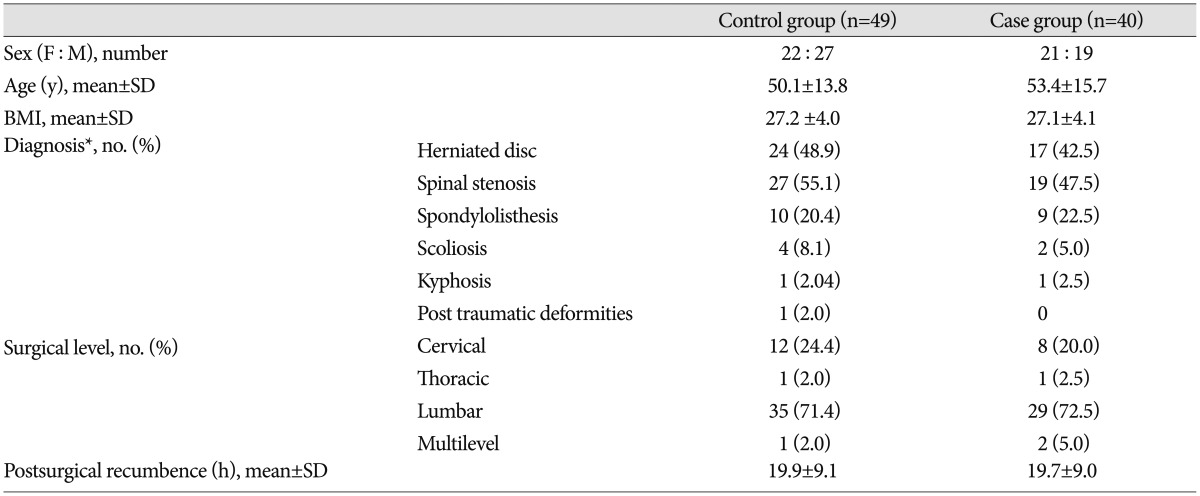
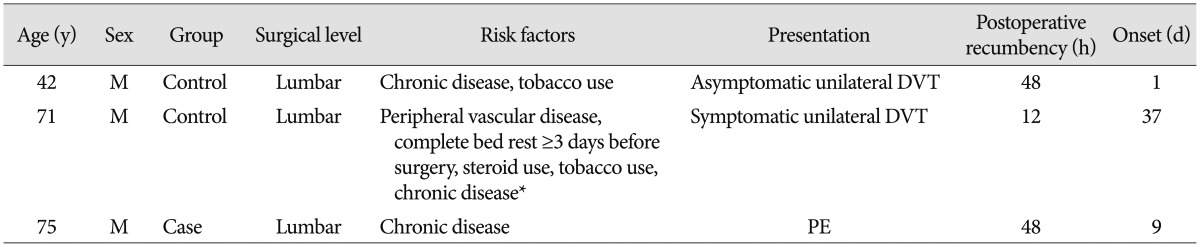
From one-hundred patients who were initially considered for inclusion, in eleven patients following could not be done. Therefore, a total of eighty-nine patients [46 male, mean age±standard deviation (SD)=51.6±14.7 y] formed the study population (demographic and patients risk factor data in each group are summarized in Table 1, 2). A total of seventy-six (85.4%) patients were considered at higher risk. Three (3.3%) postoperative VTE were recorded among 89 patients. Two (4.08%) of those VTE occurred in control group (n=49) and the other one (2.5%) occurred in case group who received chemoprophylaxis according to the protocol (n=40). All patients had CDUS study before they were out of the bed (mean±SD=19.8±9.0 h). Also, more imaging study were performed for seven suspected patients to detect VTE event. During hospitalization, there was only one confirmed asymptomatic DVT event. Also, time of VTE diagnosis was within follow up period (mean±SD=9.4±1.2 m) in two cases. One patient in case group died from fatal PE without prior clinical signs and symptoms of DVT one month after surgery (Table 3). The statistical analysis of the data revealed that patients receiving or not receiving preoperative LMWH did not disclose any relationship between preoperative chemoprophylaxis and VTE because there was no statistically significant difference [Fisher's exact test, p>0.95; 95% confidence interval (CI), 0.06-8.7]. Moreover, logistic regression showed that gender (p=0.01) and postsurgical recumbence duration (p<0.001) were significant independent risk factors for VTE.
No bleeding complications were found in any group except for one patient in the control group with cervical anterior one-level discectomy suffered postoperative hematoma that produced a tense wound and increasing pain for 8 next hours. This hematoma required reoperation. It was clarified the bleeding was due to laceration of external jugular vein during wound closure and drain insertion. None of the patients developed symptomatic SEH and no new neurological sequel onset was observed. Both intraoperative and postoperative blood loss in case group were found to be significantly lower than control group (Mann-Whitney U test, p<0.001 and p=0.017 respectively, 95% CI).
DVT with subsequent pulmonary embolism is a probable likely complication after spinal surgery, which can lead to morbidity and death3). The risk factors associated with VTE are the male gender, aging, obesity, smoking and presence of varicose veins20). In addition to the patient's clinical setting, other factors that might increase the risk of thromboembolism are : the type of spinal surgery, level and length of the operation, type of procedure, surgical approach, duration of postoperative immobilization and the presence of motor neurologic deficits6,20). The objective of this study was to investigate and compare VTE incidence in two groups of patients who underwent elective instrumental spinal surgery as implant and use of pedicle screw fixation inclusion can increase the VTE risk16,22). DVT cannot be reliably diagnosed only by a clinical examination; therefore, screening methods are important to determine the DVT expansion rate3,13). Due to the varied range of DVT in different studies and difficulties in the clinical diagnosis, a baseline CDUS was performed in this study. DVT and PE were detected in 2.2% and 1.1% of patients respectively over the eight month period; this is similar to results reported in literature when venography or CDUS were used to evaluate deep venous thrombosis13,23,24). The use of CDUS in these studies may lead neurosurgeons to underestimate the higher prevalence of VTE complications, as most surgeons estimate a lower risk of DVT11).
The use of DVT incidence in deciding the type of prophylaxis in spinal surgery is an issue that emerges here. To prevent VTE following spinal surgery, different methods have been used including mechanical and chemical prophylaxis6,20). In a previous study, mechanical prophylaxis was compared with chemoprophylaxis. It reported that the use of chemoprophylaxis was associated with the lowest prevalence of DVT incidence in spinal surgeries13). LMWH is the most effective anticoagulant chemical prophylaxis regimen, which is preferred by most orthopedic and neurological surgeons7,11,12,22). A rate of 3.3% (n=3) thromboembolic complications was seen in this study. In this series, VTE was seen in 4.08% (n=2) of the control group. Moreover, despite application of mechanical and preoperative chemical prophylaxis, a 2.5% (n=1) incidence of VTE was found in the case group. Therefore, there was no significant difference in the incidence of VTE between the two groups. In fact, this clinical context does not provide a sufficient number of research participants for a definitive conclusion. Although these results are in agreement with previous study that was performed on VTE risk in two groups of spine surgery patients, of which one group had received LMWH prophylaxis before spinal surgery and the other group had not5). In addition, there is evidence demonstrating that postoperative LMWH prophylaxis does not affect VTE risk after spinal surgery23). Of course, it should be noted that one patient who received chemoprophylaxis before surgery died one month after the operation and autopsy showed PE as the primary cause. From this study we can conclude that probably medication of LMWH as a prophylaxis has not adversely significant hemorrhagic complications. Therefore, further studies are warranted to investigate pre-operative plus post-operative prophylaxis. Hence, the necessity of the use of chemoprophylaxis, its initiation time and length, particularly in high risk patients, must be investigated. Bleeding complications, SEH and wound hematoma were not seen within 10 months follow-up in this study, yet a very critical question was whether chemical anticoagulation increases the risk of symptomatic SEH. Fears of major bleeding, SEH, wound hematoma or infection are the primary reasons why there is no global consensus over a single method for deep venous thrombosis chemoprophylaxis1,11). However, the rate of SEH in the majority of studies in which LMWH was used as a postoperative chemoprophylaxis in patients who had undergone spinal surgery have been reported to be approximately 1%5,12,21,23); on the other hand, this study was not large enough to estimate risk of SEH with the combination of chemoprophylaxis with mechanical prophylaxis because the study population was too small to prove a difference in the incidence of SEH. Additionally, this study had more limitations. CT angiography was not performed to detect PE for all patients because of the side effects and medical costs. Moreover, most patients who were visited by a surgeon and underwent an elective surgery, suffered from lumbar disease. Thus, most operations in this study were done in this anatomical region.
Despite instant initiation of mechanical and chemical prophylaxis after spinal surgeries, VTE is still a postoperative complication with a significant morbidity and mortality rate. Since the past two decades, spinal surgery has become one of the most advanced major surgeries and the incidence and prevalence of VTE with these surgeries has increasingly become an issue of concern. There are different methods of prophylaxis in the prevention of VTE incidence for this group of patients and they should be administered based on the clinical condition of the patient, associated risk factors, surgical techniques, etc. It can be performed by chemoprophylaxis and/or mechanical prophylaxis; however, the question concerning the initiation time and duration of chemoprophylaxis in spinal surgery is still not clearly answered. Consequently, further studies are warranted to investigate this. Also, as subgroup data especially in high-risk patients and instrumental operations were not sufficiently reported. Because spinal surgeries today are more complex, more extensive clinical trials are needed to find out about the complications of VTE and its prophylaxis due to the fact that chemoprophylaxis is not commonly used in the prevention of postoperative VTE because of the fear of bleeding complications and epidural hematoma.
References
1. Agnelli G, Piovella F, Buoncristiani P, Severi P, Pini M, D'Angelo A, et al. Enoxaparin plus compression stockings compared with compression stockings alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med. 1998; 339:80–85. PMID: 9654538.

2. Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003; 107(23 Suppl 1):I9–I16. PMID: 12814980.

3. Bono CM, Watters WC 3rd, Heggeness MH, Resnick DK, Shaffer WO, Baisden J, et al. An evidence-based clinical guideline for the use of antithrombotic therapies in spine surgery. Spine J. 2009; 9:1046–1051. PMID: 19931184.

4. Cabana F, Pointillart V, Vital J, Sénégas J. [Postoperative compressive spinal epidural hematomas. 15 cases and a review of the literature]. Rev Chir Orthop Reparatrice Appar Mot. 2000; 86:335–345. PMID: 10880933.
5. Cunningham JE, Swamy G, Thomas KC. Does preoperative DVT chemoprophylaxis in spinal surgery affect the incidence of thromboembolic complications and spinal epidural hematomas? J Spinal Disord Tech. 2011; 24:E31–E34. PMID: 20975599.

6. Davidson HC, Mazzu D, Gage BF, Jeffrey RB. Screening for deep venous thrombosis in asymptomatic postoperative orthopedic patients using color Doppler sonography : analysis of prevalence and risk factors. AJR Am J Roentgenol. 1996; 166:659–662. PMID: 8623645.

7. Epstein NE. A review of the risks and benefits of differing prophylaxis regimens for the treatment of deep venous thrombosis and pulmonary embolism in neurosurgery. Surg Neurol. 2005; 64:295–301. discussion 302. PMID: 16181995.

8. Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, et al. Prevention of venous thromboembolism : American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133(6 Suppl):381S–453S. PMID: 18574271.
9. Geerts WH, Heit JA, Clagett GP, Pineo GF, Colwell CW, Anderson FA Jr, et al. Prevention of venous thromboembolism. Chest. 2001; 119(1 Suppl):132S–175S. PMID: 11157647.

10. Gerlach R, Raabe A, Beck J, Woszczyk A, Seifert V. Postoperative nadroparin administration for prophylaxis of thromboembolic events is not associated with an increased risk of hemorrhage after spinal surgery. Eur Spine J. 2004; 13:9–13. PMID: 14615928.

11. Glotzbecker MP, Bono CM, Harris MB, Brick G, Heary RF, Wood KB. Surgeon practices regarding postoperative thromboembolic prophylaxis after high-risk spinal surgery. Spine (Phila Pa 1976). 2008; 33:2915–2921. PMID: 19092624.

12. Glotzbecker MP, Bono CM, Wood KB, Harris MB. Postoperative spinal epidural hematoma : a systematic review. Spine (Phila Pa 1976). 2010; 35:E413–E420. PMID: 20431474.
13. Glotzbecker MP, Bono CM, Wood KB, Harris MB. Thromboembolic disease in spinal surgery : a systematic review. Spine (Phila Pa 1976). 2009; 34:291–303. PMID: 19179925.
14. Jaffer AK. An overview of venous thromboembolism : impact, risks, and issues in prophylaxis. Cleve Clin J Med. 2008; 75(Suppl 3):S3–S36. PMID: 18494222.
15. Johns JS, Nguyen C, Sing RF. Vena cava filters in spinal cord injuries : evolving technology. J Spinal Cord Med. 2006; 29:183–190. PMID: 16859222.
16. Khan I, Nadeem M, Rabbani ZH. Thoracolumbar junction injuries and their management with pedicle screws. J Ayub Med Coll Abbottabad. 2007; 19:7–10. PMID: 18693586.
17. Leon L, Rodriguez H, Tawk RG, Ondra SL, Labropoulos N, Morasch MD. The prophylactic use of inferior vena cava filters in patients undergoing high-risk spinal surgery. Ann Vasc Surg. 2005; 19:442–447. PMID: 15864473.

18. Oda T, Fuji T, Kato Y, Fujita S, Kanemitsu N. Deep venous thrombosis after posterior spinal surgery. Spine (Phila Pa 1976). 2000; 25:2962–2967. PMID: 11074685.

19. Piasecki DP, Poynton AR, Mintz DN, Roh JS, Peterson MG, Rawlins BA, et al. Thromboembolic disease after combined anterior/posterior reconstruction for adult spinal deformity : a prospective cohort study using magnetic resonance venography. Spine (Phila Pa 1976). 2008; 33:668–672. PMID: 18344861.

20. Platzer P, Thalhammer G, Jaindl M, Obradovic A, Benesch T, Vecsei V, et al. Thromboembolic complications after spinal surgery in trauma patients. Acta Orthop. 2006; 77:755–760. PMID: 17068706.

21. Schizas C, Neumayer F, Kosmopoulos V. Incidence and management of pulmonary embolism following spinal surgery occurring while under chemical thromboprophylaxis. Eur Spine J. 2008; 17:970–974. PMID: 18421483.

22. Smith JS, Fu KM, Polly DW Jr, Sansur CA, Berven SH, Broadstone PA, et al. Complication rates of three common spine procedures and rates of thromboembolism following spine surgery based on 108,419 procedures : a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976). 2010; 35:2140–2149. PMID: 20581760.

23. Strom RG, Frempong-Boadu AK. Low-molecular-weight heparin prophylaxis 24 to 36 hours after degenerative spine surgery : risk of hemorrhage and venous thromboembolism. Spine (Phila Pa 1976). 2013; 38:E1498–E1502. PMID: 23873245.
24. Takahashi H, Yokoyama Y, Iida Y, Terashima F, Hasegawa K, Saito T, et al. Incidence of venous thromboembolism after spine surgery. J Orthop Sci. 2012; 17:114–117. PMID: 22222443.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download