Abstract
Objective
To report a minimally invasive treatment option using percutaneous pedicle screw fixation with adjuvant treatment for metastatic thoraco-lumbar and lumbar spinal tumors.
Methods
This is a retrospective study of charts of patients with spinal metastases. All were older than 18 years of age and were considered to have more than 3 months of life expectancy. The patients had single or two level lesions, and compression fracture or impending fracture. Exclusion criterion was metastasis showing severe epidural compression with definite neurological symptoms. Usually spinal segments from one level above to below pathology were stabilized. Visual analog scale (VAS) score for pain assessment and Frankel scale for neurological deficit were used, while pre- and post-operative performance status was evaluated using the Eastern Cooperative Oncology Group (ECOG).
Results
Twelve patients (nine men, three women; median age 54.29 years) underwent surgery. All patients presented with back pain with/without radicular pain. There were no early complications and perioperative mortalities. Following surgery, a significant difference between average pre- and post-operative VAS scores was found (p=0.003). Overall, 91.8% of patients (11/12) experienced improvement in their ECOG score post-operatively. The mean ambulation time was 196.9 days [95% confidence interval (CI), 86.2-307.6 days; median, 97 days]. During follow-up, nine patients died and the mean overall survival time in enrolled twelve patients was 249.9 days (95% CI, 145.3-354.4 days; median, 176 days).
The primary surgical goal for spinal metastasis is usually pain relief and preservation of ambulatory functions1). In the last two decades, developments of surgical methods have resulted in improved outcomes of postoperative quality of life. Direct decompressive surgery followed by radiotherapy (RT) is reportedly superior to RT alone for ambulatory function and survival3). This landmark study, along with subsequent studies showing a benefit to patient quality of life and cost-effectiveness with surgery, provide strong evidence for a paradigm shift in the management of metastatic epidural spinal disease5,9,18). However, conventional open surgeries are associated with high morbidity and mortality rates21). For these reasons, minimally invasive techniques have become increasingly popular in spinal metastatic patients.
In the literature, many authors have used minimally invasive techniques in an effort to decrease the rate of complications of open surgical method. Firstly, some investigator have tried vertebroplasty (VP) for potentially collapsed or fragile vertebral body augmentation. However, this procedure may not be indicated if there is concern of cement leakage or tumor retropulsion. Althought other surgeons have reported their surgical techniques using mini-open surgery with percutaneous instrumentation, they were relatively less invasive for obvious collapsed and cord compression in spinal metastasis8,16,17,23).
In this retrospective study, we present preliminary clinical results of percutaneous pedicle screw fixation for impending instability in thoraco-lumbar and lumbar spine metastasis.
This is a retrospective study using the medical charts of patients harboring lumbar spinal metastases, who underwent surgery. From June 2010 to December 2012, 12 patients underwent percutaneous pedicle screw fixation for spinal metastasis involving the lumbar spine, at a single center by three surgeons (two neurosurgeons and one orthopedic surgeon). All of the patients were older than 18 years of age. The patients had single or two level lesions involving T11 to L5, and compression fracture or impending fracture invading 50% of the vertebral body. They were allocated to the palliative surgery group by using a prognostic scoring system. The patients were considered to have a life expectancy of more than 3 months according to the medical oncologist. Exclusion criteria were metastasis showing poor general condition or definite epidural compression with severe neurological deficites including paraplegia and bladder/bowel symptom.
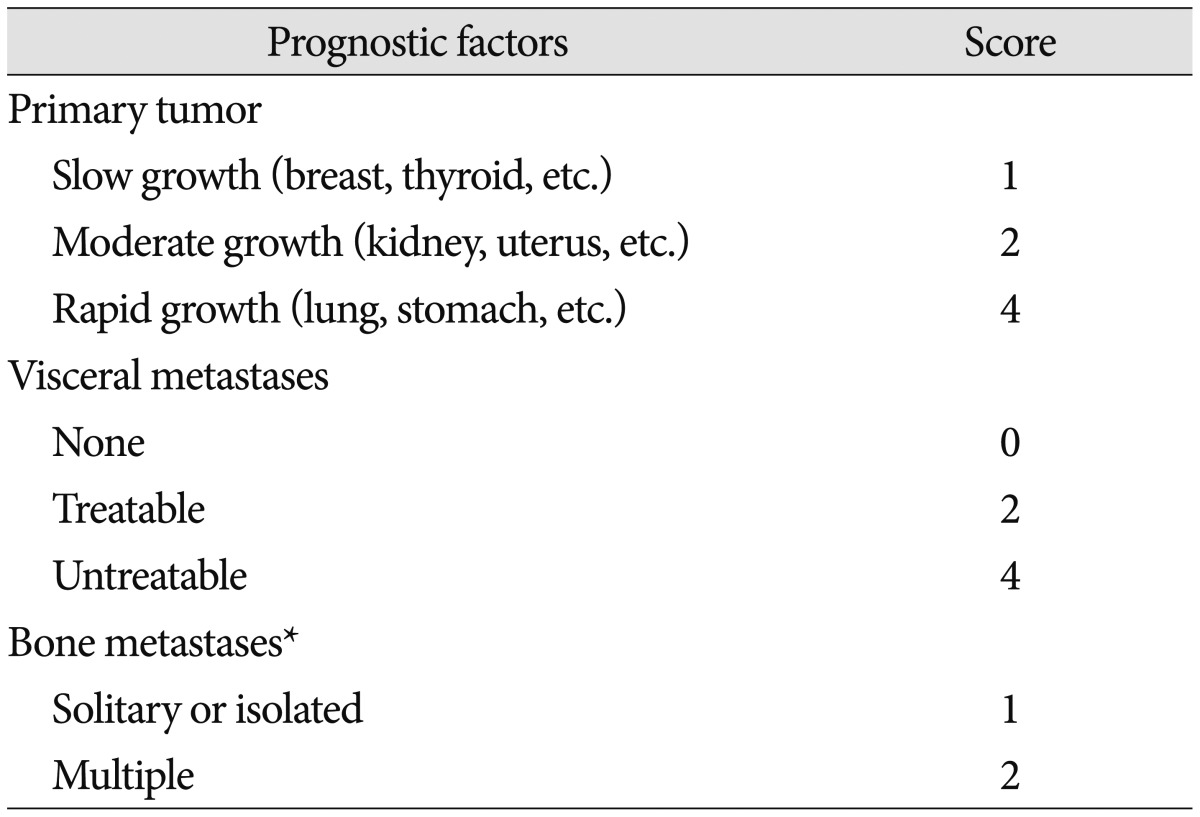
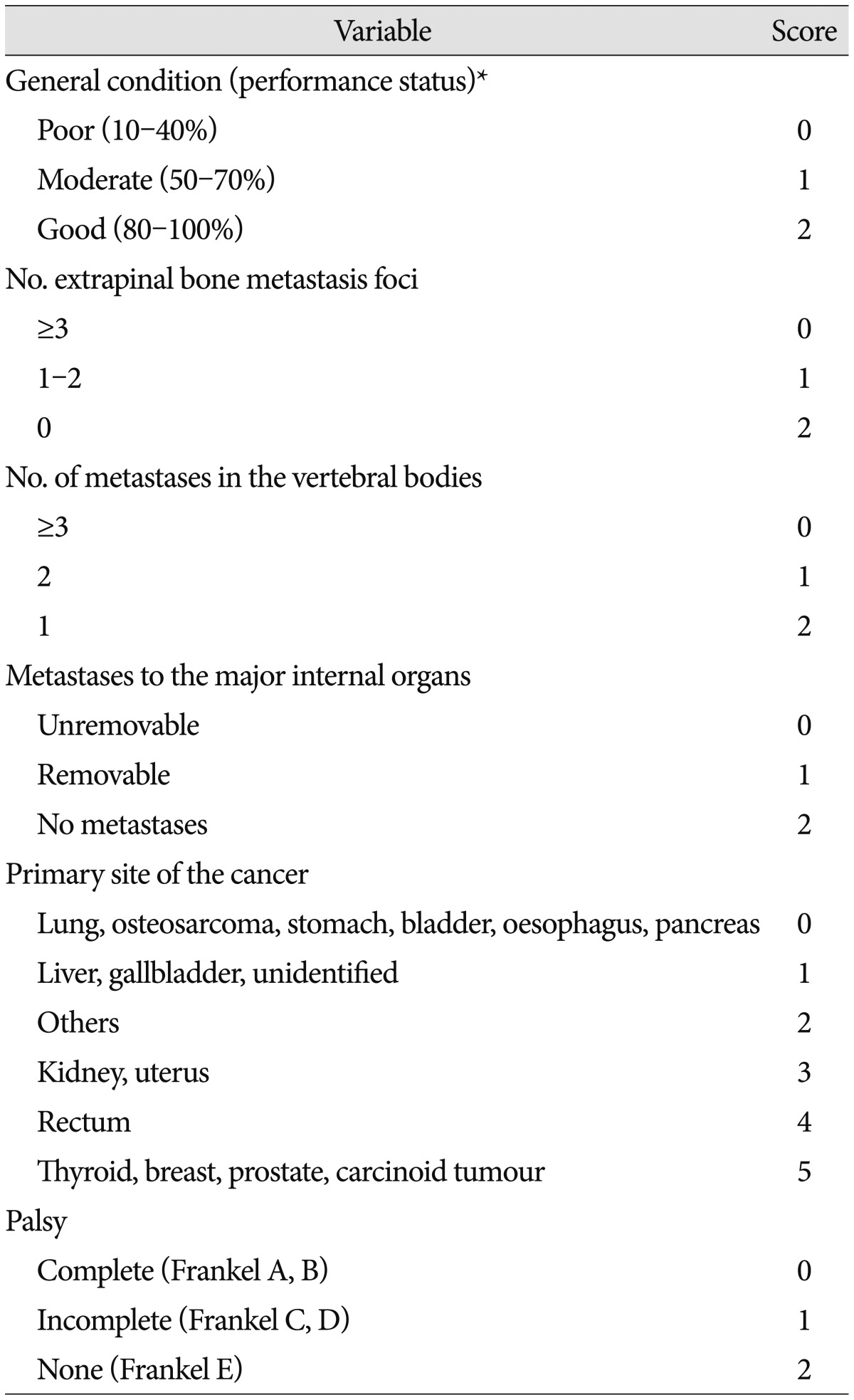
Preoperative work-up included routine laboratory test, plain X-ray, computed tomography (CT), and magnetic resonance imaging (MRI). For the assessment of tumor spread, Tomita scoring system was used (Table 1)20). This is the prevalent prognostic scoring system, which primarily considers tumor type, visceral metastases, and bone metastases. The revised Tokuhashi scoring system was also used; the Tokuhashi score has 2 additional considerations, performance status and spinal cord palsy (Table 2)19). Spinal instability neoplastic score (SINS) system was used for the assessment of spinal instability (Table 3)6). The overall SINS scores of 0-6, 7-12, and 13-18 corresponded to stable, potentially unstable, and unstable spines, respectively.
The goal of surgery was to stabilize the motion segment and/or realign the spinal column, according to the needs of individual patients. Usually, spinal segments from one level above and below the pathology were stabilized by a percutaneous pedicle screw using CD Horizon Sextant System or Longitude System (Medtronics, Minneapolis, MN, USA). The patient was placed in a prone position on a radiolucent table. Pedicles were cannulated using a Jamshidi needle under fluoroscopic guidance. K-wires were inserted down the center of needles, in which all other instruments were safely passed into the pedicle and vertebral body. The pedicle screws were advanced over the K-wires under fluoroscopic guidance via small stab incisions. Once the pedicle screws and screw extensions were placed, rods were passed through small stab incisions into the screw heads through channels in the extensions. Once appropriately positioned, the construct was tightened to provide rigid internal fixation. Adjuvant treatments consisted of RT and various systemic chemotherapies according to primary pathology, disease status, and preoperative treatment.
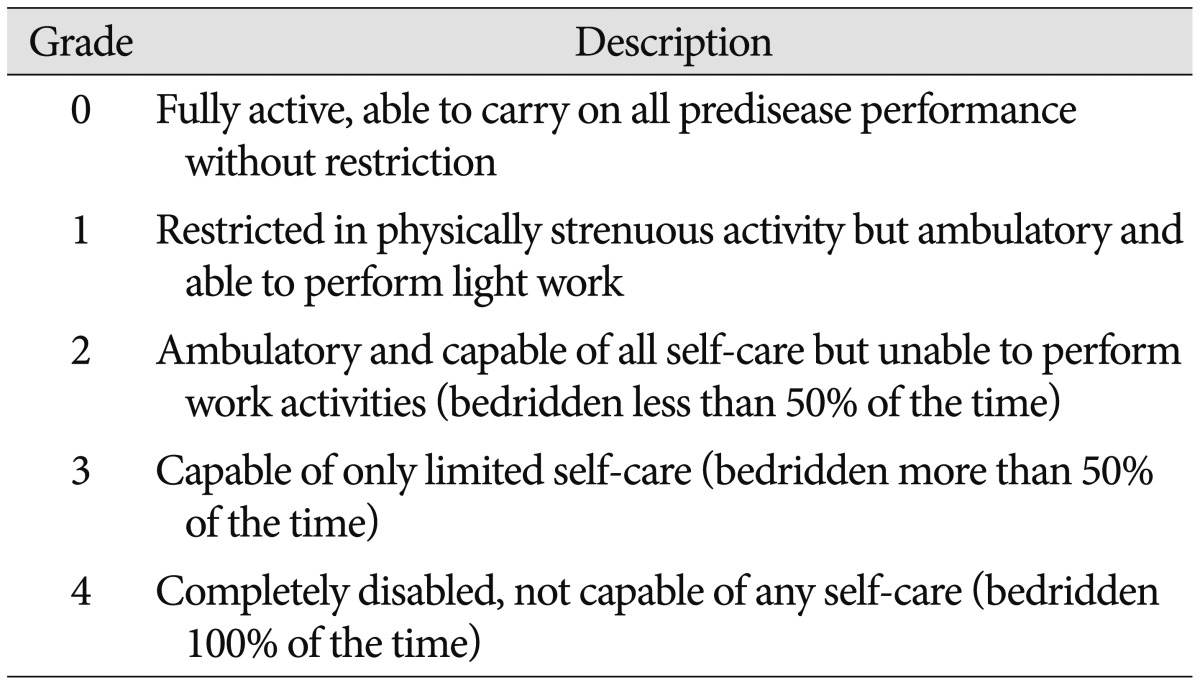
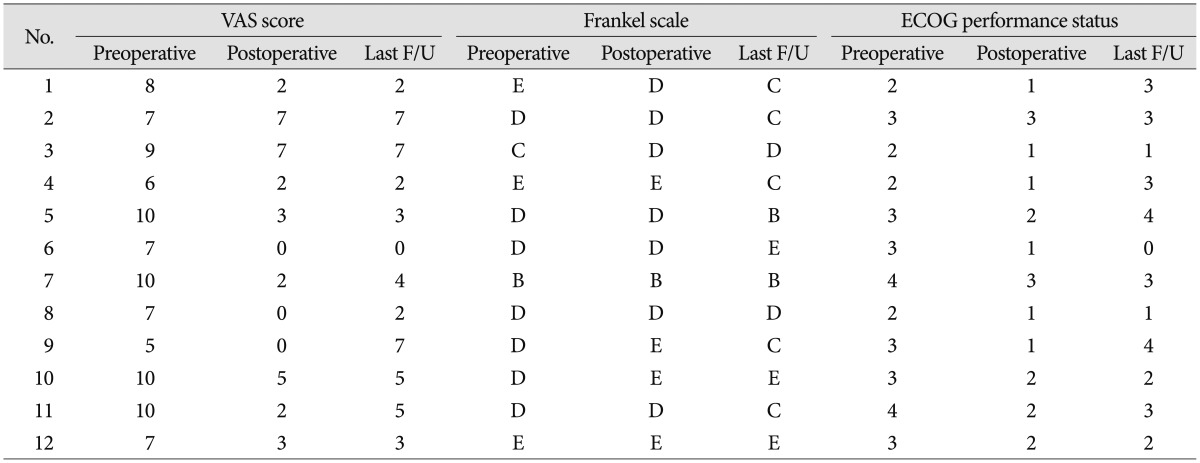
Data on operative time, blood loss, length of hospital stay, and complications were collected during hospitalization. All patients underwent postoperative X-ray to check abnormal screw placement. All intraoperative complications and those that occurred within the first 30 days postoperatively were considered as early complications. Perioperative mortality was defined as death within 30 days after surgery. The primary outcome in this study was improvement of pain and preservation of ambulation function. Patients were assessed for neurological deficit preoperatively and post-operatively at discharge and every month after discharge, using a visual analog scale (VAS) score and Frankel scale (A-E). In order to account for the nonlinear relationship in pain progression, as previously described, we defined VAS score of 1-4 as mild, 5-7 as moderate, and 8-10 as severe pain. Performance status was evaluated as secondary outcome, and it was assessed using the Eastern Cooperative Oncology Group (ECOG) scale (Table 4).
For investigation of the baseline characteristics of patients, descriptive statistics were used. Comparison of the pain score between preoperative and postoperative status was analyzed by Wilcoxon signed rank test. Ambulation time and survival time were analyzed by using Kaplan-Meier method. Statistical analyses were performed using IBM SPSS 21.0 statistical software (IBM Corp., Armonk, NY, USA). A probability value of less than 0.05 was accepted as statistically significant.
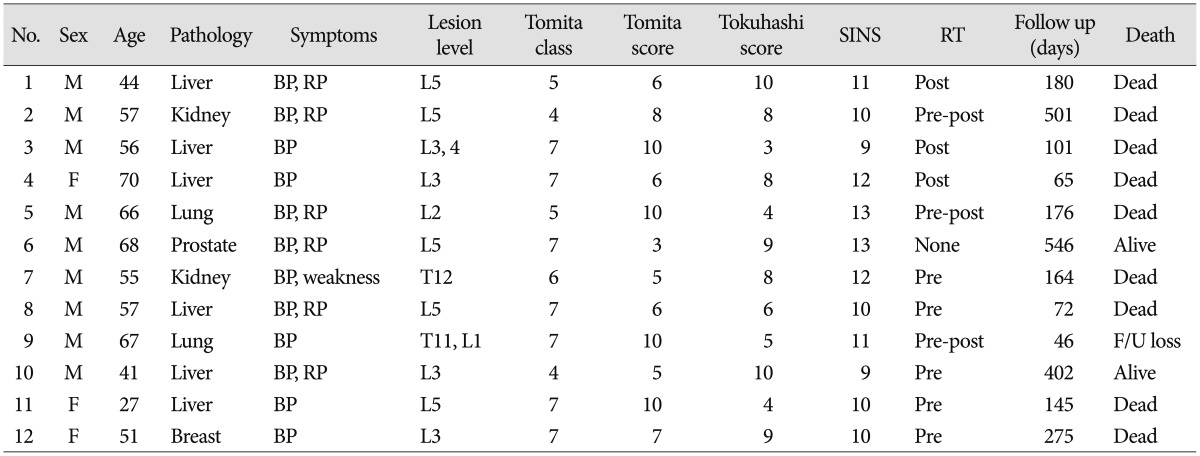
Twelve patients (nine men, three women; 27-70 years of age, median 54.29 years) underwent percutaneous pedicle screw fixation of the thoraco-lumbar and lumbar spine. The mean follow-up duration was 222.75±171.6 days (range, 46-546 days) after surgery. Baseline characteristics of patients are recorded in Table 5. Most of the patients presented with back pain with/without radicular pain except one patient with intractable pain and paraparesis due to spinal metastasis on T12. Various primary cancers were metastasized to the spine. Common pathologies were hepatocellular carcinoma in six cases. Lung cancer and renal cell carcinoma followed as in two cases respectively. There was one case each of prostate cancer, and breast cancer. According to Tomita classification, all of the spine metastases were type 4 or higher. Applying Tomita score system, ten patients had a Tomita score >5, and seven patients had a score >7. Applying revised Tokuhashi score system, eight patients were expected to survive <6 months (Tokuhashi score <9). According to SINS-criteria, all of patients were deemed unstable (2 out of 12 patients) or potentially unstable (10 out of 12 patients). As initial treatment modalities, RT was performed in six patients preoperatively. One patient received VP at the metastatic level 3 month before surgery.
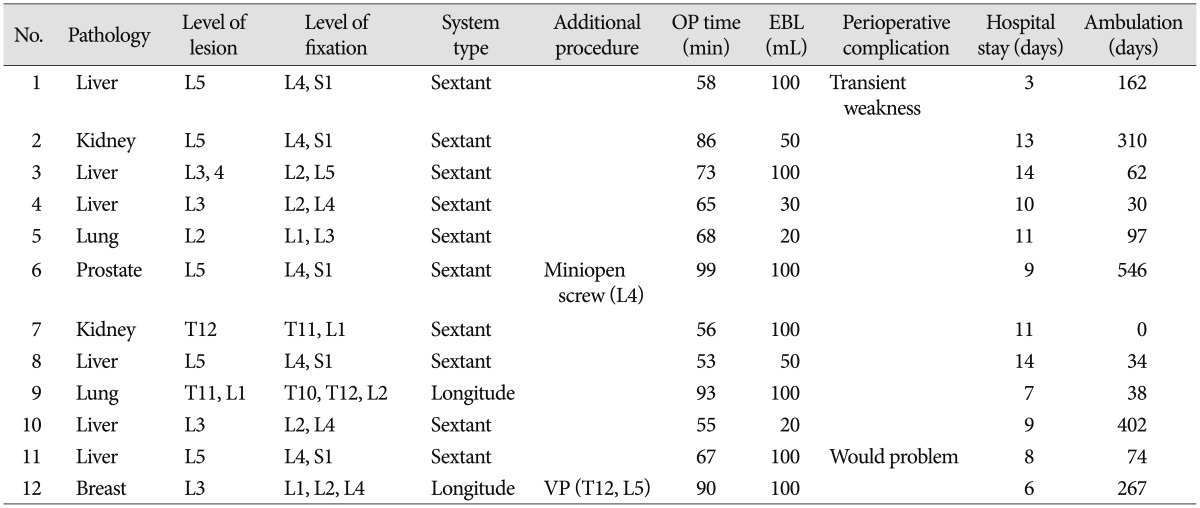
Operative data including estimated blood loss and surgical times are shown in Table 6. Although more than half of the patients (8/12, 66.7%) had multiple metastases, ten patients had one metastatic lesion at the lumbar spine. Two patient having two thoracolumbar or lumbar lesions. In ten patients, 2 level lumbar pedicle screw fixation were performed above and below metastatic lesion site. In two patients, 3 level pedicle screw fixation were used. One patient (case 12) underwent VP at T12, L1, and L5 during the same operation simultaneously. In another case, two screw fixations on L4 were converted to open method using paramedian incision due to deep position. Mean operation time was 71.9 minutes (range, 55-99 minutes), and mean blood loss was 72.5 mL (range, 20-100 mL).
There have been no technical issues with the surgical procedures and no surgical complications. On postoperative CT, there is no cortex breach and spinal canal or neural foramen invasion. However, one patient developed transient dorsiflexion weakness of big toe after surgery, which resolved completely in 4 weeks using steroid. None of the patients required blood transfusion or admission to the Intensive care unit. Postoperative RT was performed in six patients including three patients who underwent RT before surgery. RT was initiated between postoperative 5-10 days. As a result, eleven patients underwent RT at pre and/or postoperative period except on patient with prostate cancer who was managed with hormone therapy.
Most of the patients (11/12, 91.8%) had reduced pain after surgery (Table 7). Of these eleven patients, three patients became pain-free. Comparison of pain before and after surgery showed significant improvement (p=0.03). Average pre- and post-operative VAS scores for the cohort were 8.0 and 2.75 respectively. The pain decreased by more than 33% in 91.6% (11/12) of patients and by greater than 66% in 58.3% (7/12) of patients. More than half the patients (7/12) maintained improved VAS score for back pain until the last follow-up. Before surgery, ten patients had ambulatory ability whether mild neurologic symptom was apparent or not. All of these patients preserved ambulatory function after surgery, although one patient (case 5) changed from Frankel scale E to D. Another patient (case 2) who was unable to walk before surgery improved ambulatory function after surgery (Fig. 1). In ECOG performance scores, four patients (33.3%) were ECOG 2, six (50%) were ECOG 3 and two (16.7%) were ECOG 4. In all of patients, the ECOG either improved or remained unchanged postoperatively. Specifically, no change between the pre- and post-operative ECOG scores was found for one patient. Eight patients experienced an improvement in their ECOG score by one-grade, while three patients experienced an improvement of two-grades.
Mean ambulation start date was 3.67±1.58 days after surgery (range, 2-7 days) except for one patient who was unable to walk before surgery. This non-ambulatory patient was capable of wheel-chair ambulation 4 days and could walk 8 days after surgery. The mean ambulation time was 196.9±56.5 days [95% confidence interval (CI), 86.2-307.6 days; median, 97 days]. During follow-up, nine patients died and the mean overall survival time in enrolled twelve patients was 249.9±53.3 days (95% CI, 145.3-354.4 days; median, 176 days) (Fig. 2).
The treatment strategy for metastatic spinal tumors are most often palliative rather than curative, due to the short life expectancy of most spinal cancer patients2). The main aims of surgery are pain control, functional preservation, and restoration of stability. A previous study reported that operative treatment of symptomatic spinal metastases in patients with good general health status improves quality of life4). However, conventional surgery is anticipated to involve massive blood loss during surgery and have many risks including excessive muscle manipulations and visceral and neurovascular injury. For these reasons, various minimally invasive surgical techniques including VP, endoscopy-assisted surgery, and mini-open surgery have been introduced and shown to have acceptable clinical outcomes in metastatic spine tumor11,12,23).
In metastatic spinal fracture, VP already showed a benefit for pain reduction. Additionally, VP are able to augment an unstable vertebral body7,15). However, this procedure may not be indicated if there is concern of cement leakage or tumor retropulsion. Therefore, VP for metastatic spinal compression fracture requires meticulous patient selection. In our experience, percutaneous cement augmentation does not seem to relieve the radicular pain caused by mechanical instability with spinal metastases. If there already is a vertebral collapse, like in case 4 who was previously treated by VP, cement augmentation has a limited role for mechanical supporting of metastatic instability. Although the cement is injected into the vertebral body and thus adequately stabilizes it, it is not injected into the pedicle or the joint and does not stabilize the posterior elements.
Our surgical procedure consists of percutaneous and minimally invasive technique such as VP or kyphoplasty. The goal of percutaneous posterior instrumentation is to stabilize the spinal column in order to prevent pressure on vertebral body and the nerve root, and to ultimately provide palliation of back pain and radicular pain. Due to the rather simple surgical procedure, the operation time is short and there is less blood loss. These factors enable early ambulation and short hospitalization, as well as a low complication rate. In addition, the skin incision is small and there is less muscular dissection compared to open surgery. These attributes permit early wound healing, less wound complication, and early initiation of RT.
Among various adjuvant treatment modalities, RT is the most commonly used treatment. However, recent studies demonstrated the possibility of vertebral collapse after RT or stereotactic radiosurgery3,14). In the cases with a high risk of vertebral collapse and impending or overt vertebral collapse, our technique would be performed with RT or stereotactic radiosurgery to prevent collapse or some restoration of vertebral body height. Recently published data showed some restoration of sagittal angle after percutaneous pedicle screw fixation10). Although the surgical results of decompressive surgery followed by RT was superior to those of RT alone in a randomized prospective study, this option generally indicates only 10-15% of metastatic spinal cord compression13). In addition, lumbar region is more tolerable to epidural compression than thoracic region. In cases of breast and prostate cancer having effective adjuvant therapies, palliative surgery may play an important role in the stability22).
Even though all of our patients did not undergo open surgery, significant pain reduction (91.7%, 11/12) and functional preservation (100%, 11/11) were achieved. Stability was gained from pedicle screw fixation along with RT assisting pain reduction for metastasis-originated instability. Most of the patients had preserved ambulatory function after surgery. This was partly helped by pain reduction and regained stability. Especially, a preoperative non-ambulatory patient (case 3) was capable of ambulation after surgery, perhaps due to significant reduction of mechanical back pain and radicular pain. We postulate that most patients were not debilitated by neurologic dysfunction, but rather incapacitated by pain caused by mechanical radiculopathy due to spinal instability. This improvement in functional capacity supports that surgical intervention is a reasonable option for pain management in patients with mechanical radiculopathy secondary to metastatic disease.
In our study, survival after surgery varied widely. This was partly due to various primary pathologies and limited number of patients. Considering that most of our patients were advanced cases, the survival periods were comparable to the other palliative surgery study. In addition, our study showed considerable amount of ambulation time during follow-up period. Although patient have poor prognosis according to prognostic scoring systems, percutaneous pedicle screw fixation with radiation therapy would help to improve survival as well as pain and neurologic status.
Our preliminary results have demonstrated that the procedure can be safely performed. Even though the study period was short, there were no intervention-related complications and instrumentation failure until the last follow-up. A proper comparative evaluation with larger series of the patients will be required to definitively compare the results of our technique with other open and minimally invasive procedures in the patients with metastatic spinal tumors.
A minimally invasive technique using percutaneous pedicle screw fixation would be a good alternative treatment option for impending instability or instability caused by metastasis, especially when considering RT.
Other intensive treatment including chemotherapy and hormone therapy as well as surgery would improve patient's quality of life in terms of pain and ambulatory function. Furthermore, the decrease in functional performance these patients experience appears to be secondary to pain, rather than true neurological dysfunction.
References
2. Bartels RH, Feuth T, van der Maazen R, Verbeek AL, Kappelle AC, André Grotenhuis J, et al. Development of a model with which to predict the life expectancy of patients with spinal epidural metastasis. Cancer. 2007; 110:2042–2049. PMID: 17853394.

3. Cunha MV, Al-Omair A, Atenafu EG, Masucci GL, Letourneau D, Korol R, et al. Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT) : analysis of predictive factors. Int J Radiat Oncol Biol Phys. 2012; 84:e343–e349. PMID: 22658511.
4. Di Martino A, Vincenzi B, Denaro L, Barnaba SA, Papalia R, Santini D, et al. 'Internal bracing' surgery in the management of solid tumor metastases of the thoracic and lumbar spine. Oncol Rep. 2009; 21:431–435. PMID: 19148519.

5. Falicov A, Fisher CG, Sparkes J, Boyd MC, Wing PC, Dvorak MF. Impact of surgical intervention on quality of life in patients with spinal metastases. Spine (Phila Pa 1976). 2006; 31:2849–2856. PMID: 17108840.

6. Fourney DR, Frangou EM, Ryken TC, Dipaola CP, Shaffrey CI, Berven SH, et al. Spinal instability neoplastic score : an analysis of reliability and validity from the spine oncology study group. J Clin Oncol. 2011; 29:3072–3077. PMID: 21709187.

7. Gerszten PC, Monaco EA 3rd. Complete percutaneous treatment of vertebral body tumors causing spinal canal compromise using a transpedicular cavitation, cement augmentation, and radiosurgical technique. Neurosurg Focus. 2009; 27:E9. PMID: 19951062.

8. Huang TJ, Hsu RW, Li YY, Cheng CC. Minimal access spinal surgery (MASS) in treating thoracic spine metastasis. Spine (Phila Pa 1976). 2006; 31:1860–1863. PMID: 16845365.

9. Ibrahim A, Crockard A, Antonietti P, Boriani S, Bünger C, Gasbarrini A, et al. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2007. J Neurosurg Spine. 2008; 8:271–278. PMID: 18312079.

10. Kim CH, Chung CK, Sohn S, Lee S, Park SB. Less invasive palliative surgery for spinal metastases. J Surg Oncol. 2013; 108:499–503. PMID: 23982866.

11. Le Huec JC, Lesprit E, Guibaud JP, Gangnet N, Aunoble S. Minimally invasive endoscopic approach to the cervicothoracic junction for vertebral metastases : report of two cases. Eur Spine J. 2001; 10:421–426. PMID: 11718197.

12. Mobbs RJ, Nakaji P, Szkandera BJ, Teo C. Endoscopic assisted posterior decompression for spinal neoplasms. J Clin Neurosci. 2002; 9:437–439. PMID: 12217675.

13. Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer : a randomised trial. Lancet. 2005; 366:643–648. PMID: 16112300.

14. Rodríguez-Ruiz ME, San Miguel I, Gil-Bazo I, Perez-Gracia JL, Arbea L, Moreno-Jimenez M, et al. Pathological vertebral fracture after stereotactic body radiation therapy for lung metastases. Case report and literature review. Radiat Oncol. 2012; 7:50. PMID: 22455311.

15. Schneider F, Greineck F, Clausen S, Mai S, Obertacke U, Reis T, et al. Development of a novel method for intraoperative radiotherapy during kyphoplasty for spinal metastases (Kypho-IORT). Int J Radiat Oncol Biol Phys. 2011; 81:1114–1119. PMID: 20934272.

16. Singh K, Samartzis D, Vaccaro AR, Andersson GB, An HS, Heller JG. Current concepts in the management of metastatic spinal disease. The role of minimally-invasive approaches. J Bone Joint Surg Br. 2006; 88:434–442. PMID: 16567775.
17. Tancioni F, Navarria P, Pessina F, Marcheselli S, Rognone E, Mancosu P, et al. Early surgical experience with minimally invasive percutaneous approach for patients with metastatic epidural spinal cord compression (MESCC) to poor prognoses. Ann Surg Oncol. 2012; 19:294–300. PMID: 21743979.

18. Thomas KC, Nosyk B, Fisher CG, Dvorak M, Patchell RA, Regine WF, et al. Cost-effectiveness of surgery plus radiotherapy versus radiotherapy alone for metastatic epidural spinal cord compression. Int J Radiat Oncol Biol Phys. 2006; 66:1212–1218. PMID: 17145536.

19. Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 2005; 30:2186–2191. PMID: 16205345.

20. Tomita K, Kawahara N, Murakami H, Demura S. Total en bloc spondylectomy for spinal tumors : improvement of the technique and its associated basic background. J Orthop Sci. 2006; 11:3–12. PMID: 16437342.

21. Weber BR, Grob D, Dvorák J, Müntener M. Posterior surgical approach to the lumbar spine and its effect on the multifidus muscle. Spine (Phila Pa 1976). 1997; 22:1765–1772. PMID: 9259789.

22. Yamashita T, Aota Y, Kushida K, Murayama H, Hiruma T, Takeyama M, et al. Changes in physical function after palliative surgery for metastatic spinal tumor : association of the revised Tokuhashi score with neurologic recovery. Spine (Phila Pa 1976). 2008; 33:2341–2346. PMID: 18827700.

23. Zairi F, Arikat A, Allaoui M, Marinho P, Assaker R. Minimally invasive decompression and stabilization for the management of thoracolumbar spine metastasis. J Neurosurg Spine. 2012; 17:19–23. PMID: 22607222.

Fig. 1
A 57-year-old man with intractable back pain and radiculopathy due to spinal metastasis from renal cell carcinoma. A and B : Preoperative plain X-ray and sagittal reconstruction lumbar spine computed tomography reveals an osteolytic lesion of L5 body and compression fracture. C and D : Preoperative axial and sagittal T2 weighted magnetic resonance (MR) imaging show metastatic tumor with mild epidural compression. E : Follow-up plain X-ray 6 month after percutaneous screw fixation and radiation theraphy shows no further vertebral collapse canal compromise. F and G : Follw-up axial and sagittal T2 weighted MR imaging show the improvement of epidural compression.
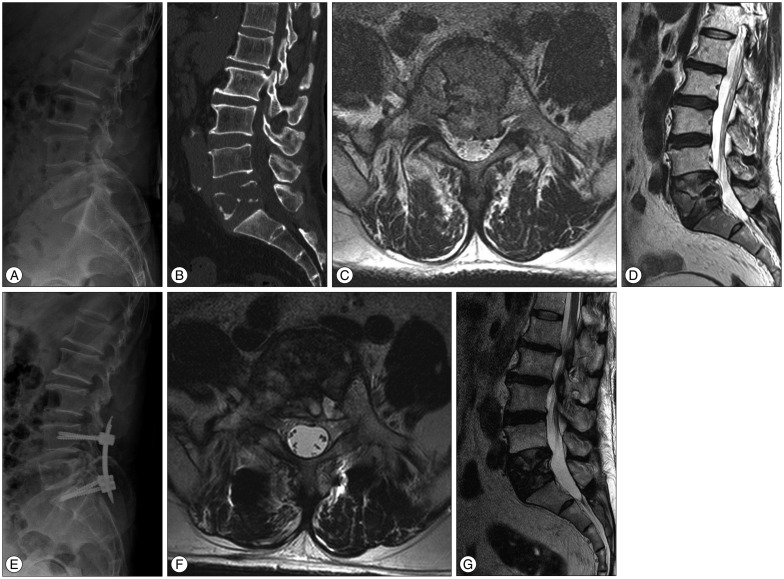
Fig. 2
Progression free survival (A) and overall survival (B) analysis. During follow-up, the mean ambulation time was 196.9±56.5 days [95% confidence interval (CI), 86.2-307.6 days; median, 97 days] and the mean overall survival time was 249.9±53.3 days (95% CI, 145.3-354.4 days; median, 176 days).
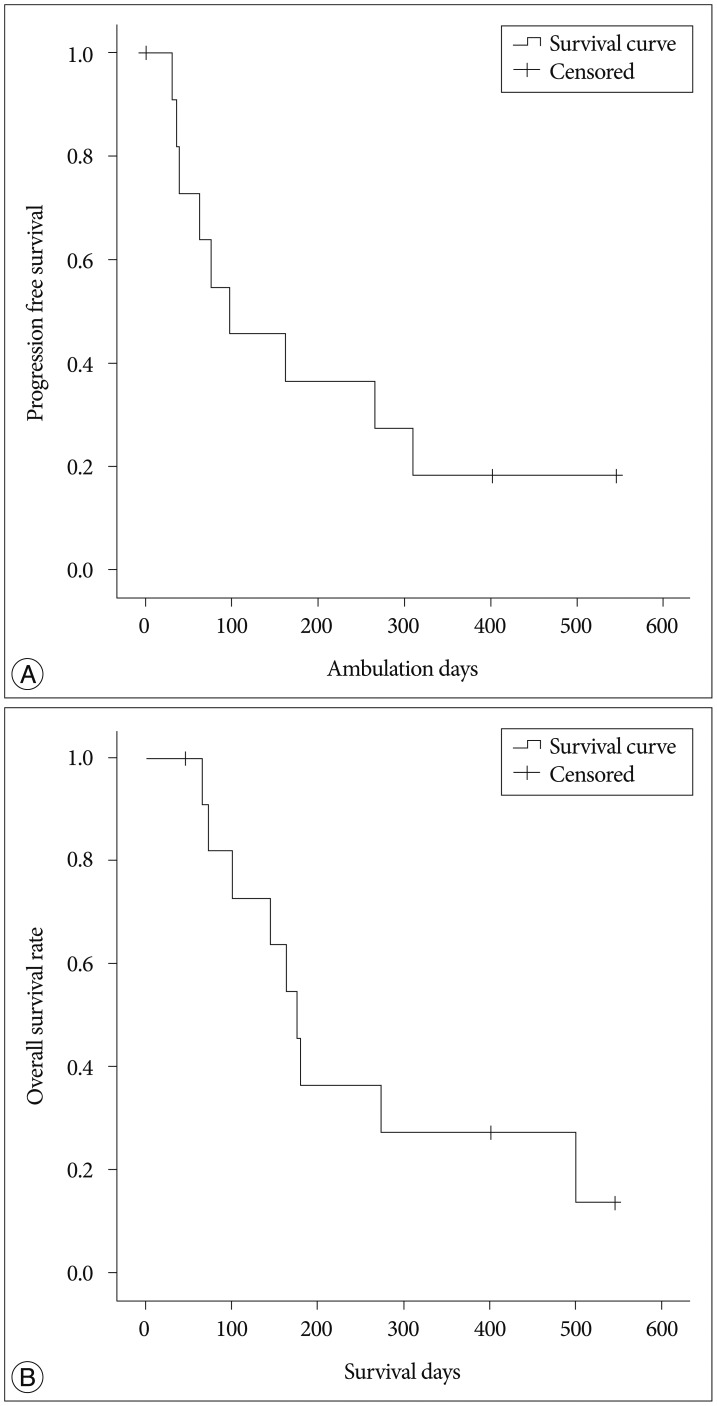
Table 3
Spine instability neoplastic score (SINS)
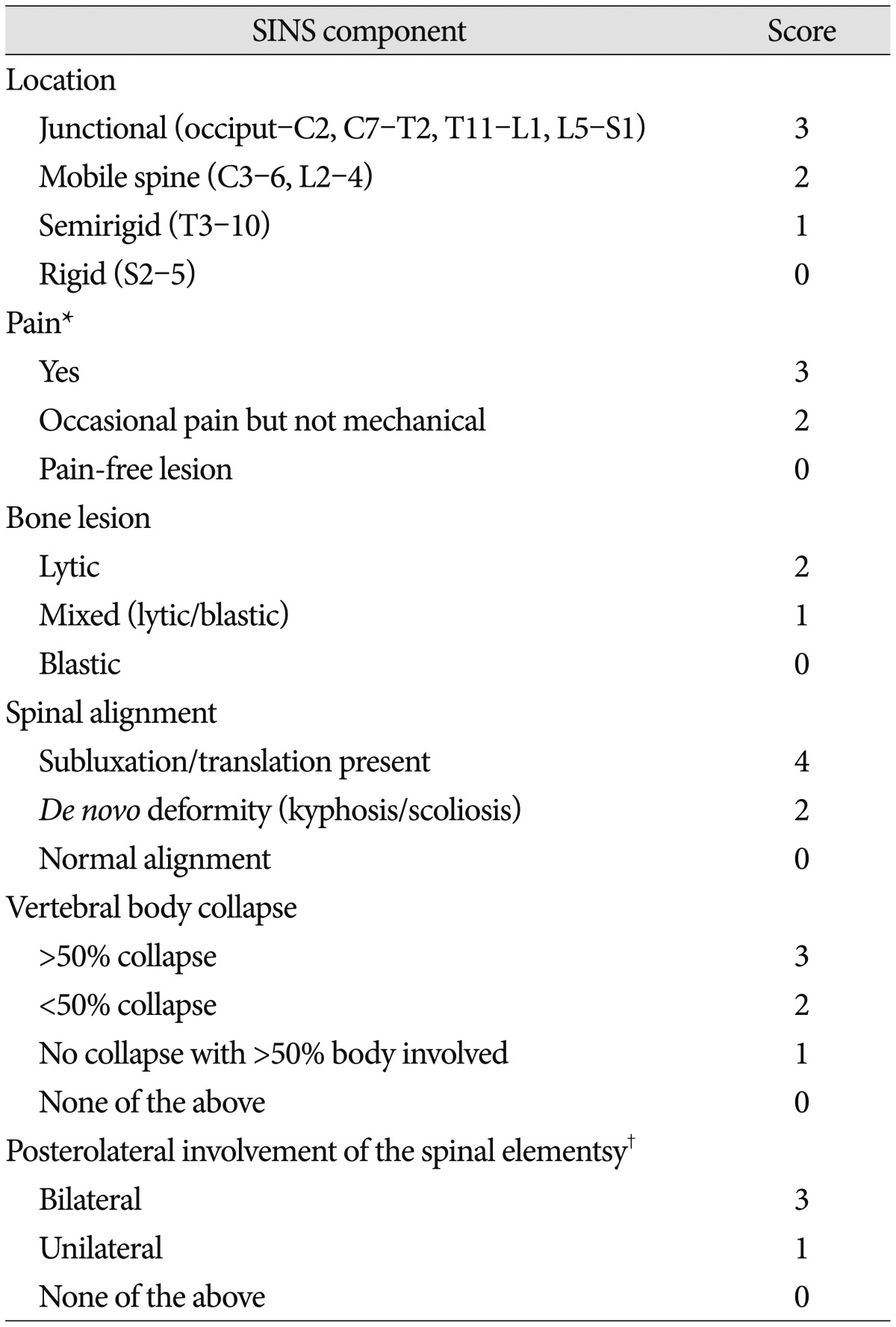
Criteria of instability. Total score (TS) 0-6 : stable spine, TS 7-12 : potential unstable spine, TS 13-18 : unstable spine. Recommendation : TS ≥7, consider surgical intervention. *Pain improvement with recumbency and/or pain with movement/loading of the spine, †Facet, pedicle, or costovertebral joint fracture or replacement with tumor




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download