Abstract
Synovial cysts of the cervical spine, although they occur infrequently, may cause acute radiculopathy or myelopathy. Here, we report a case of a cervical synovial cyst presenting as acute myelopathy after manual stretching. A 68-year-old man presented with gait disturbance, decreased touch senses, and increased sensitivity to pain below T12 level. These symptoms developed after manual stretching 3 days prior. Computed tomography scanning and magnetic resonance imaging revealed a 1-cm, small multilocular cystic lesion in the spinal canal with cord compression at the C7-T1 level. We performed a left partial laminectomy of C7 and T1 using a posterior approach and completely removed the cystic mass. Histological examination of the resected mass revealed fibrous tissue fragments with amorphous materials and granulation tissue compatible with a synovial cyst. The patient's symptoms resolved after surgery. We describe a case of acute myelopathy caused by a cervical synovial cyst that was treated by surgical excision. Although cervical synovial cysts are often associated with degenerative facet joints, clinicians should be aware of the possibility that these cysts can cause acute neurologic symptoms.
Synovial cysts with neurologic symptoms are common in the lumbar spine, but rare in the cervical spine. Most cervical synovial cysts are found incidentally, but may cause cervical radiculopathy or myelopathy due to compression of the spinal cord or nerve roots. A review of the literature revealed only 31 cases of synovial cysts of the cervical spine; in most of these cases, the cysts had a non-traumatic origin10). Only two cases were associated with major trauma presenting as myelopathy1,8). Here, we present a patient who presented with acute paraparesis after manual stretching due to a cervical synovial cyst, and we discuss the clinical aspects of this disease. Although a cervical synovial cyst is often associated with degeneration of facet joints, clinicians should be aware that cervical synovial cysts can cause acute neurologic presentations.
A 67-year-old man with a 10-year history of lower back pain presented with abrupt onset gait disturbance and paresthesia in his lower limbs after manual stretching 3 days prior. On admission, neurological evaluation revealed weakness of both legs (hip flexion : G4/5, Knee extension : G4/5, foot plantarflexion and dorsiflexion : G4/5), and the patient showed diminished touch sensation with increased sensitivity to pain below the level of the T12 dermatome. On deep tendon reflex examination, the patient's right patellar tendon reflex was diminished; the other reflexes were increased.
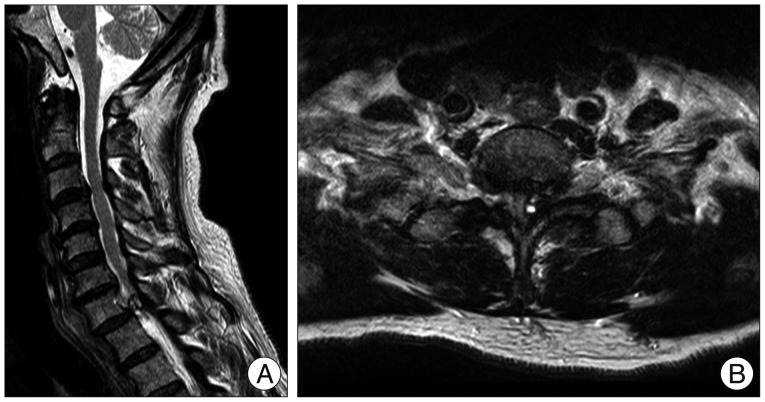
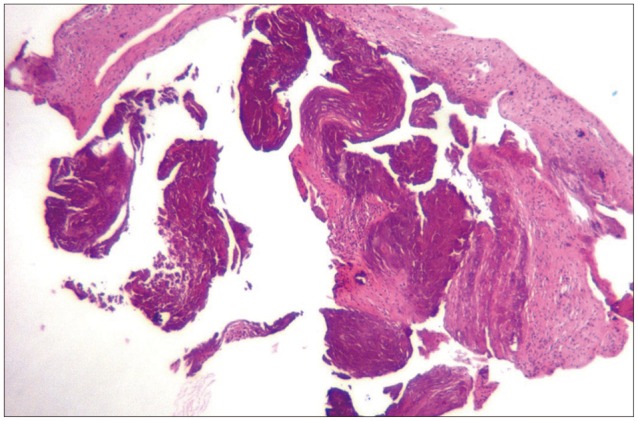
We performed magnetic resonance imaging (MRI) of his whole spine to accurately assess spinal cord lesion. Cervical MRI identified a 1 cm diameter extradural cystic lesion in the spinal canal with cord compression at the left C7-T1 level (Fig. 1). We performed a left partial laminectomy of C7 and T1 using a posterior approach and completely removed the cystic mass under the intraoperative neurophysiologic monitoring. Histological examination of the resected mass showed fibrous tissue fragments with amorphous materials and granulation tissue, consistent with a synovial cyst (Fig. 2). The patient's neurologic symptoms were markedly improved after surgery.
Synovial cysts of the spinal column arise from the lining of defective facet joints or those with degenerated articulations5). Synovial cysts usually occur in patients aged 50-60 years and there is no gender bias2,6,8). Most cases are asymptomatic and are detected incidentally, but may cause pain, radiculopathy, or myelopathy. Synovial cysts with neurologic presentations usually occur in the lumbar spine4,8,10).
A cervical synovial cyst can also induce severe neurologic deterioration. However, this condition is very rare; only 31 previous studies have reported an association between a cervical synovial cyst and neurologic changes10). A review of literature revealed that 10 of these cysts occurred at the upper cervical level (peri-odontoid process, C1-C2 articulations related to rheumatoid arthritis, only one case in C3-C4) and 21 cases in C6-C7 or C7-T1 facet joints. Most cases presented with acute or progressive myelopathy induced by a non-traumatic origin. Only two cases of a cervical synovial cyst presenting as myelopathy associated with trauma have been described. One patient developed spastic paraplegia after spine fracture1), while the other case of posttraumatic myelopathy was related to cyst enlargement due to intra-cystic acute hemorrhage8). In the case presented here, there was no acute formation of a synovial cyst or hematoma by microscopic examination and no evidence of a fracture.
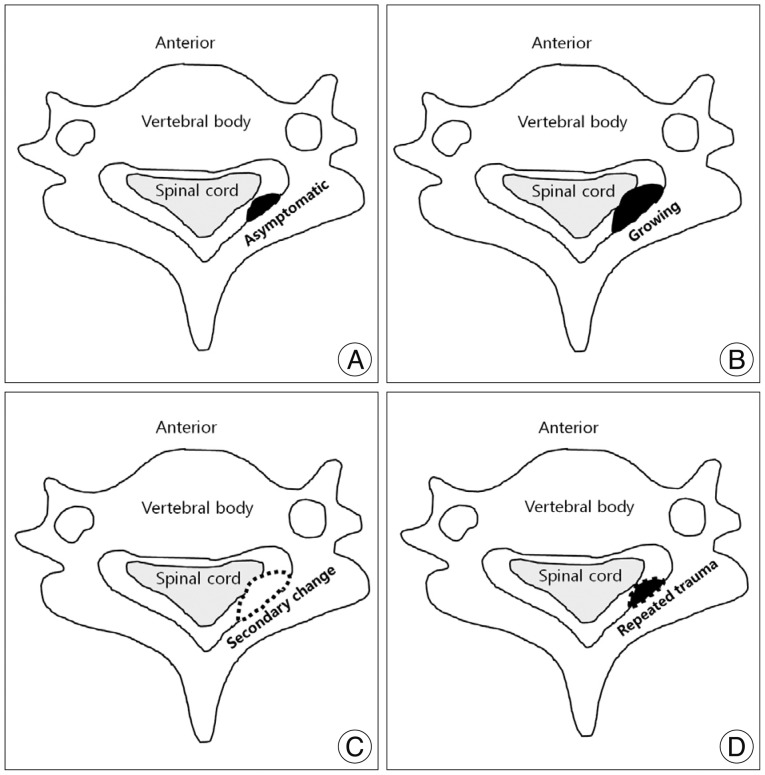
The pathogenesis of synovial cysts with symptoms remains unclear. There are some possible pathophysiologic mechanisms that could induce neurologic deterioration. (Fig. 3) First, synovial cysts may grow due to motion resulting in a mass effect over time. In these cases, neurologic deterioration could develop progressively. As was reported previously8), secondary changes of the cyst, such as intra-cystic hematoma after trauma, presence of a calcified cystic wall, or an inflammatory response can induce neurologic changes7). Third, regardless of changes in cyst size, patients with degenerative static synovial cysts may undergo direct trauma or hyperextension resulting in spinal cord or nerve root damage. In our patient, acute myelopathy resulted from pressure to his posterior neck applied by a massage therapist; he reported that he felt as if an electric shock flowed from his thoracic to his lower extremities. At that moment, his degenerative cervical synovial cyst seemed to give rise to direct spinal cord injury. Even in the absence of a traumatic event, a synovial cyst may aggravate spinal cord ischemia resulting from direct static compression.
In the past, cervical myelography was performed to diagnose a cervical synovial cyst1,8). Nowadays, T2-weighted MR and CT scanning allow excellent visualization of cystic lesions with high signal and confirmation of proximity to the spinal cord or nerve root10,11). Other extradural spine tumors in the posterior column, including meningiomas, perineural cysts, dermoid cysts, lymphoma, abscess and metastases, should be considered in the differential diagnosis2,9). Recently, it was reported that facet arthrography allowed preoperative determination of the continuity between the extradural lesion and the facet joint, leading to confirmation of a synovial cyst11).
The prognosis of a symptomatic cervical synovial cyst varies; some patients recover after surgical removal of the cyst, while others experience spontaneous resolution without surgery3,6). In lumbar synovial cysts, CT-guided percutaneous needle aspiration or corticosteroid injection have been attempted as non-surgical treatments, but these approaches have not been used to treat cervical synovial cyst7). In cervical synovial cysts, a percutaneous needle procedure may worsen the patient's neurologic state if the cyst ruptures. Hence, surgical excision is generally accepted as the treatment of choice for cervical synovial cysts, as it results in early neurological improvement and there have been no reports of the recurrence of a cervical synovial cyst after surgical excision.
We described a case of acute myelopathy caused by a cervical synovial cyst that was treated successfully by surgical excision. Although a cervical synovial cyst is often associated with degenerative facet joints, clinicians should be aware that cervical synovial cysts can cause acute neurologic symptoms.
Acknowledgements
This study was supported by BioGreen 21 (PJ009051) of Rural Development Administration.
References
1. Cartwright MJ, Nehls DG, Carrion CA, Spetzler RF. Synovial cyst of a cervical facet joint : case report. Neurosurgery. 1985; 16:850–852. PMID: 4010912.
2. Cho BY, Zhang HY, Kim HS. Synovial cyst in the cervical region causing severe myelopathy. Yonsei Med J. 2004; 45:539–542. PMID: 15227744.

3. Colen CB, Rengachary S. Spontaneous resolution of a cervical synovial cyst. Case illustration. J Neurosurg Spine. 2006; 4:186. PMID: 16506489.
4. Epstein NE. Lumbar synovial cysts : a review of diagnosis, surgical management, and outcome assessment. J Spinal Disord Tech. 2004; 17:321–325. PMID: 15280763.
5. Epstein NE, Hollingsworth R. Synovial cyst of the cervical spine. J Spinal Disord. 1993; 6:182–185. PMID: 8504232.

6. Hénaux PL, Hamlat A, Riffaud L, Guégan Y, Morandi X. Spontaneous regression of a symptomatic atlanto-occipital joint cyst. Case report. Neurochirurgie. 2011; 57:129–132. PMID: 21907363.

7. Hsu KY, Zucherman JF, Shea WJ, Jeffrey RA. Lumbar intraspinal synovial and ganglion cysts (facet cysts). Ten-year experience in evaluation and treatment. Spine (Phila Pa 1976). 1995; 20:80–89. PMID: 7709284.
8. Jabre A, Shahbabian S, Keller JT. Synovial cyst of the cervical spine. Neurosurgery. 1987; 20:316–318. PMID: 3561742.

9. Lunardi P, Acqui M, Ricci G, Agrillo A, Ferrante L. Cervical synovial cysts : case report and review of the literature. Eur Spine J. 1999; 8:232–237. PMID: 10413351.
10. Seo HY, Chung JY, Park GH, Shin YJ. Cervical facet cyst causing progressive paraplegia : a case report and review of literature. J Korean Soc Spine Surg. 2011; 18:29–33.

11. Tofuku K, Koga H, Komiya S. Facet arthrography of a cervical synovial cyst. J Neurointerv Surg. 2012; 4:e17. PMID: 21990488.

Fig. 1
Preoperative cervical T2-weighted MRI revealed (A : sagittal, B : axial) a 1-cm sized, small extradural multilocular cystic lesion occupying the spinal canal with cord compression at the left C7-T1 level.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download