Abstract
Owing to the focal wall defect covered with thin fibrous tissues, an aneurysm arising from the dorsal wall of the internal carotid artery (ICA) is difficult to manage either surgically or endovascularly and is often associated with high morbidity and mortality. Unfortunately, the definitive treatment modality of such highly risky aneurysm has not yet been demonstrated. Upon encountering the complex intracranial pathophysiology of such a highly precarious aneurysm, a neurosurgeon would be faced with a challenge to decide on an optimal approach. This is a case of multiple paraclinoid aneurysms including the ICA dorsal wall aneurysm, presented with spontaneous subarachnoid hemorrhage. With respect to treatment, direct clipping with a Sundt graft clip was performed after multiple endovascular interventions had failed. This surgical approach can be a treatment modality for a blood blister-like aneurysm after failed endovascular intervention(s).
Blood blister-like aneurysms (BBAs) at non-branching sites of the supraclinoid portion of internal carotid artery (ICA) are rare but important cause of subarachnoid hemorrhage (SAH)1,10,14,16). It is very imperative to recognize this lesion as a different type of aneurysm than ordinary berry aneurysms. BBAs of the ICA are very fragile thin-walled aneurysms that lack an identifiable neck1,14). In this report, the authors summarized the clinical course of a patient, harboring multiple paraclinoid aneurysms including an ICA dorsal wall aneurysm, who presented with spontaneous SAH.
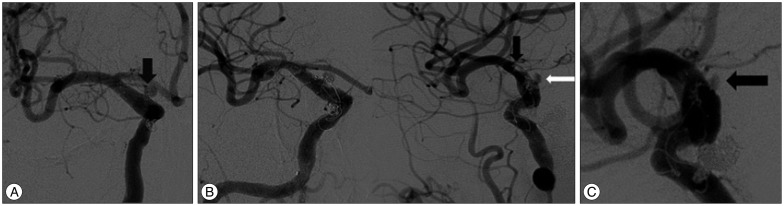
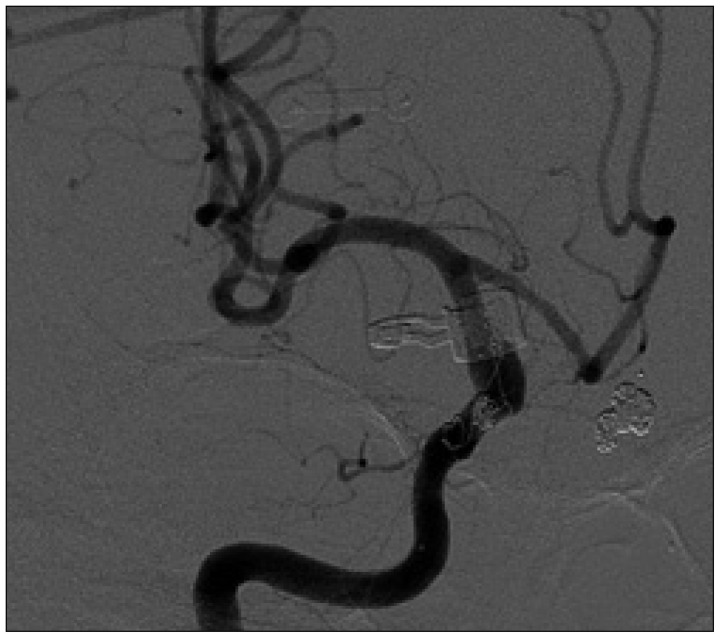
A 56-year-old woman presented with a sudden onset of a bursting headache. She was drowsy without other focal neurologic deficits. Her clinical SAH rating was Hunt Hess grade III, while her radiologic classification corresponded to Fisher Grade III (Fig. 1A). Cerebral angiography on the day of admission revealed three aneurysms. The right carotid angiogram revealed two aneurysms, one of which on the dorsal wall of the ICA and the other on the ventral wall of the ICA (Fig. 1B). The left carotid angiogram revealed a saccular aneurysm in the origin site of the left superior hypophyseal artery (Fig. 1C). Owing to the homogenous spread of SAH in the basal cisterns, it was difficult to decide the ruptured aneurysm. First, endovascular coil embolization was performed for each aneurysm. Endovascular double stent-assisted coil embolization (Codman Enterprise, Raynham, MA, USA and ev3 Inc., Solitaire, Irvine, CA, USA) was carried out for the aneurysms of the right ICA dorsal wall and ventral wall (Fig. 2A). Then, stent assisted coil embolization (ev3 Inc., Solitaire, Irvine, CA, USA) was performed for the left superior hypophyseal artery aneurysm (Fig. 2B). These aneurysms were nearly completely obliterated. Seven days after the first embolization, conventional cerebral angiography demonstrated mild recanalization of the right ICA dorsal wall aneurysm over the previously embolized site. Follow-up angiography on the 19th day showed further enlargement of the right ICA dorsal wall aneurysm (Fig. 3A). In the second session, further coiling was impossible due to the lack of aneurysmal wall resistance and additional stent placement was also failed due to unsuccessful navigation of a stent catheter owing to the hindrance of previously placed stents. Furthermore, we failed in removing the microwire caught between stent(s) or wall of the ICA. After careful clockwise and counterclockwise rotation of the wire, the distal portion of the microwire was cut within the stents. Angiography demonstrated a delayed filling of the right ICA dorsal wall aneurysm and some thrombus formation which in distal to the origin site of the right anterior choroidal artery (Fig. 3B). After the second embolization, she had drowsiness and left hemiparesis. Her diffusion MRI revealed multiple tiny acute cerebral infarctions in the territory of the right middle cerebral artery. Follow-up cerebral angiogram after seven days of the second session demonstrated further recanalization of the aneurysm (Fig. 3C). We decided surgical approach, including extracranial-intracranial (EC-IC) bypass and trapping of the ICA or direct clipping with the Sundt clip graft. Initially, we exposed the right cervical carotid bifurcation area for the proximal control and possible high-flow bypass procedures. After a right fronto-temporal craniotomy, wide dissection of the Sylvian fissure and the intradural drilling of the anterior clinoid process were performed. The medial wall of the distal ICA showed a purplish bulging attached to the right optic nerve. Some portion of previously placed stent strut and coils were visible through the wall of the ICA and the aneurysm, respectively (Fig. 4). After identification and dissection of the surrounding major structures, the aneurysm was secured successfully with the Sundt clip graft with a 5 mm diameter and 3 mm width. The bypass procedure was unnecessary because the blood flow was unchanged before and after the clipping. The right carotid angiogram on the next day of clipping revealed good patency of the ICA and no aneurysmal dilatation. The patient improved gradually with a hemiparesis on the left side (grade III, arm and grade IV, leg). Five months later after clipping, follow-up angiography demonstrated no aneurysmal recanalization with a patency of the arterial lumen to its normal configuration (Fig. 5). Follow-up angiography of 2-years after the clipping also showed unchanged good condition.
Aneurysms arising from the dorsal wall of the ICA are rare with an incidence rate of 0.9 to 6.5% of all of the ICA aneurysms and particularly difficulty lesions to manage successfully1,10). Fragile thin-walled aneurysms have wide and poorly defined necks and make it difficult to clip primarily. Several treatment options for the treatment of blister-like aneurysms, including direct clipping, wrapping only, clipping on the wrapping materials, direct repair, ICA trapping with or without bypass, and endovascular approach, have been reported1,2,4,7,9,14,15,17,18,19). Ogawa et al.12) reported that wrapping only had not prevented rebleeding and had been associated with a high incidence of postoperative bleeding and death. A direct arterial suture followed by clip reinforcement has reportedly been a rather valid treatment modality for dorsal wall ICA aneurysms7,9). Some authors often prefer direct surgical clipping. If direct clipping should be attempted, the clip must be applied with the clip blades positioned parallel to the parent artery, and also should include the arterial wall beyond the lesion1,15). Parallel clip application has been associated with a high rate of intraoperative rupture, parent artery stenosis, and avulsion of the lesion from the ICA. To handle possible unsuccessful clipping, Gar-rett and Spetzler5) placed a strip of wrapping material around the artery before direct clipping is attempted. There were also other reports of using a special encircling clip, which resulted in better outcome14,18,19). The other treatment options include endovascular treatments, such as stent-assisted coil embolization, stent-in-stent technique, and endovascular ICA occlusion with or without bypass surgery. Stent-assisted coil embolization has been reported as a treatment preference for the management of dorsal wall ICA aneurysms4,17). However, Park et al.13) asserted in their recent report of seven patients who presented with SAH due to ruptured ICA BBA and treated with endovascular methods that endovascular coil embolization could not be the definitive treatment modality for ICA BBAs. The use of stent-in-stent technique had been reported6,9). Gaughen et al.6) suggested that a staged endovascular treatment entailing the use of a stent-in-stent technique, augmented with subsequent coil embolization, would be a viable endovascular option for the treatment of ruptured supraclinoid blister aneurysms, which were initially too small and shallow for coils to be introduced on the first day of treatment. Lee et al.11) reported that endovascular trapping of the ICA, including the segment of lesion, should be considered as the first option for the definitive treatment, if the balloon occlusion test could be successful. Recently, it was reported that the procedure encompassing bypass surgery and ICA trapping (surgical or endovascular) would be an another definitive treatment option for ICA BBAs2,8). A case similar to ours would be the Cho et al.3) report, which reported a successful case of the use of an encircling clip graft for the treatment of a BBA after endovascular treatment (stent-in-stent technique) had failed. In our case, several attempts of endovascular procedures, such as stent assisted coil embolization, repeated coil embolization for recanalized aneurysm failed to prevent aneurysmal enlargement or reduce the risk of rebleeding of the fragile aneurysm. As the next best solution, we decided surgical approach including EC-IC bypass and trapping of the ICA or direct clipping with the Sundt clip graft. In the final stage of the surgery, the Sundt clip graft was applied to the ICA, for which two endovascular stents and coils had already been placed. In this case, clipping-induced stenosis could be minimized by the previously inserted self-expandable stents, which resulted in good preservation of the luminal flow by having the stent as a vascular frame. To our know-ledge, this is the first report of successful clipping case with the Sundt clip graft in a previously stents assisted coiled but recanalized ICA BBA. When considering the selection of the appropriate clip, it is reasonable to undersize the length and to oversize the diameter of the clip for the prevention of the Sundt clip graft ssociated complications such as perforator injury or stenosis of the parent vessels14).
As shown in this case, multiple paraclinoid aneurysms including the ICA dorsal wall aneurysm resented with spontaneous SAH may be treated by first applying stent-assisted coiling. Follow-up conventional cerebral angiograms convincingly demonstrate recanalization of the ICA dorsal wall aneurysm in the previously embolized site. Accordingly, a direct clipping approach with a Sundt clip graft may prove to be a rather useful treatment modality for fragile aneurysm(s), for which other options, such as repeated coil embolization, as well as endovascular stent placement (stent-in-stent technique) are not feasible.
References
1. Abe M, Tabuchi K, Yokoyama H, Uchino A. Blood blisterlike aneurysms of the internal carotid artery. J Neurosurg. 1998; 89:419–424. PMID: 9724116.

2. Başkaya MK, Ahmed AS, Ateş O, Niemann D. Surgical treatment of blood blister-like aneurysms of the supraclinoid internal carotid artery with extracranial-intracranial bypass and trapping. Neurosurg Focus. 2008; 24:E13. PMID: 18275289.

3. Cho TG, Hwang SN, Nam TK, Park SW. Salvage surgical treatment for failed endovascular procedure of a blood blister-like aneurysm. J Cerebrovasc Endovasc Neurosurg. 2012; 14:99–103. PMID: 23210036.

4. Fiorella D, Albuquerque FC, Deshmukh VR, Woo HH, Rasmussen PA, Masaryk TJ, et al. Endovascular reconstruction with the Neuroform stent as monotherapy for the treatment of uncoilable intradural pseudoaneurysms. Neurosurgery. 2006; 59:291–300. discussion 291-300. PMID: 16823325.

5. Garrett M, Spetzler RF. Surgical treatment of blister-like aneurysms. World Neurosurg. 2012; 77:76–77. PMID: 22405389.

6. Gaughen JR Jr, Hasan D, Dumont AS, Jensen ME, McKenzie J, Evans AJ. The efficacy of endovascular stenting in the treatment of supraclinoid internal carotid artery blister aneurysms using a stent-in-stent technique. AJNR Am J Neuroradiol. 2010; 31:1132–1138. PMID: 20150303.

7. Joo SP, Kim TS, Moon KS, Kwak HJ, Lee JK, Kim JH, et al. Arterial suturing followed by clip reinforcement with circumferential wrapping for blister-like aneurysms of the internal carotid artery. Surg Neurol. 2006; 66:424–428. discussion 428-429. PMID: 17015131.

8. Kawashima A, Okada Y, Kawamata T, Onda H, Kubo O, Hori T. Successful treatment of a blood blister-like aneurysm of the internal carotid artery by trapping with a high-flow bypass. J Clin Neurosci. 2008; 15:797–800. PMID: 18406147.

9. Kim BM, Chung EC, Park SI, Choi CS, Won YS. Treatment of blood blister-like aneurysm of the internal carotid artery with stent-assisted coil embolization followed by stent-within-a-stent technique. Case report. J Neurosurg. 2007; 107:1211–1213. PMID: 18077959.

10. Kim YG, Kim YD. Direct repair of a dorsal wall aneurysm on supraclinoid internal carotid artery. J Korean Neurosurg Soc. 2005; 37:160–162.
11. Lee CC, Hsieh TC, Wang YC, Lo YL, Lee ST, Yang TC. Ruptured symptomatic internal carotid artery dorsal wall aneurysm with rapid configurational change. Clinical experience and management outcome: an original article. Eur J Neurol. 2010; 17:1277–1284. PMID: 20831774.

12. Ogawa A, Suzuki M, Ogasawara K. Aneurysms at nonbranching sites in the surpaclinoid portion of the internal carotid artery : internal carotid artery trunk aneurysms. Neurosurgery. 2000; 47:578–583. discussion 583-586. PMID: 10981744.

13. Park JH, Park IS, Han DH, Kim SH, Oh CW, Kim JE, et al. Endovascular treatment of blood blister-like aneurysms of the internal carotid artery. J Neurosurg. 2007; 106:812–819. PMID: 17542524.

14. Park PJ, Meyer FB. The Sundt clip graft. Neurosurgery. 2010; 66(6 Suppl Operative):300–305. discussion 305. PMID: 20489520.

15. Shigeta H, Kyoshima K, Nakagawa F, Kobayashi S. Dorsal internal carotid artery aneurysms with special reference to angiographic presentation and surgical management. Acta Neurochir(Wien). 1992; 119:42–48. PMID: 1481751.

16. Sim SY, Shin YS, Cho KG, Kim SY, Kim SH, Ahn YH, et al. Blood blister-like aneurysms at nonbranching sites of the internal carotid artery. J Neurosurg. 2006; 105:400–405. PMID: 16961134.

17. Tanoue S, Kiyosue H, Matsumoto S, Yamashita M, Nagatomi H, Mori H. Ruptured "blisterlike" aneurysm with a pseudoaneurysm formation requiring delayed intervention with endovascular coil embolization. Case report. J Neurosurg. 2004; 101:159–162. PMID: 15255268.

18. Yanagisawa T, Mizoi K, Sugawara T, Suzuki A, Ohta T, Higashiyama N, et al. Direct repair of a blisterlike aneurysm on the internal carotid artery with vascular closure staple clips. Technical note. J Neurosurg. 2004; 100:146–149. PMID: 14743928.

19. Yanaka K, Meguro K, Nose T. Repair of a tear at the base of a blister-like aneurysm with suturing and an encircling clip : technical note. Neurosurgery. 2002; 50:218–221. PMID: 11844255.

Fig. 1
A : Brain CT scan reveals thick and diffuse SAH in the basal cisterns. B : Digital subtraction angiogram demonstrating a blood blister-like aneurysmal dilatation (black arrow) on the dorsal wall of the right distal ICA and a saccular aneurysm (white arrow) on the paraclinoid portion of the right ICA (white arrow). C : Left carotid angiogram reveals a saccular aneurysm (white arrow) on the paraclinoid portion of the left ICA. SAH : subarachnoid hemorrhage, ICA : internal carotid artery.
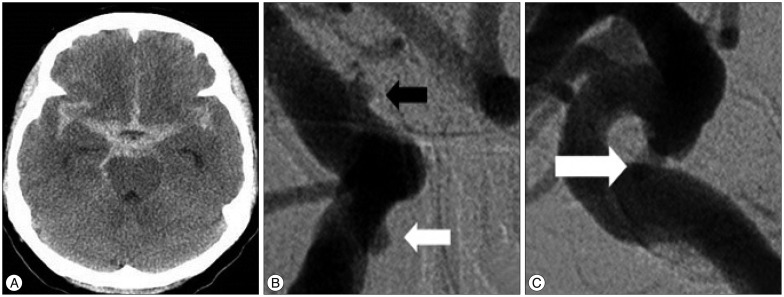
Fig. 2
Digital subtraction angiogram after the first coil embolization. An-teroposterior oblique view (A) and lateral view (B) show aneurysms on both ICAs are almost completely obliterated. ICA : internal carotid artery.

Fig. 3
A : Follow-up angiography on the 19th day shows further enlargement of the right ICA dorsal wall aneurysm (black arrow). B : Angiography after second embolization demonstrates a delayed filling of the right ICA dorsal wall aneurysm (white arrow) and some thrombus formation (black arrow) distal to the origin site of the right anterior choroidal artery. C : Follow-up cerebral angiogram on the seventh day after second embolization demonstrates recanalization (black arrow) of the right ICA dorsal wall aneurysm. ICA : internal carotid artery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download