Abstract
Objective
We assessed the life-time prevalence (LTP) of chronic low back pain (LBP) in young Korean males. We also evaluated the relationship between lumbar spinal lesions and their health related quality-of-life (HRQOL).
Methods
A cross-sectional, self-reported survey was conducted in Korean males (aged 19-year-old) who underwent physical examinations for the conscript. We examined 3331 examinees in November 2014. We included 2411 subjects, who accepted to participate this study without any comorbidities. We interviewed using simple binary questions for their LBP experience and chronicity. HRQOL was assessed by Short-Form Health-Survey-36 (SF-36) in chronic LBP and healthy control groups. Radiological assessment was performed in chronic LBP group to determine whether there were any pathological causes of their symptoms.
Results
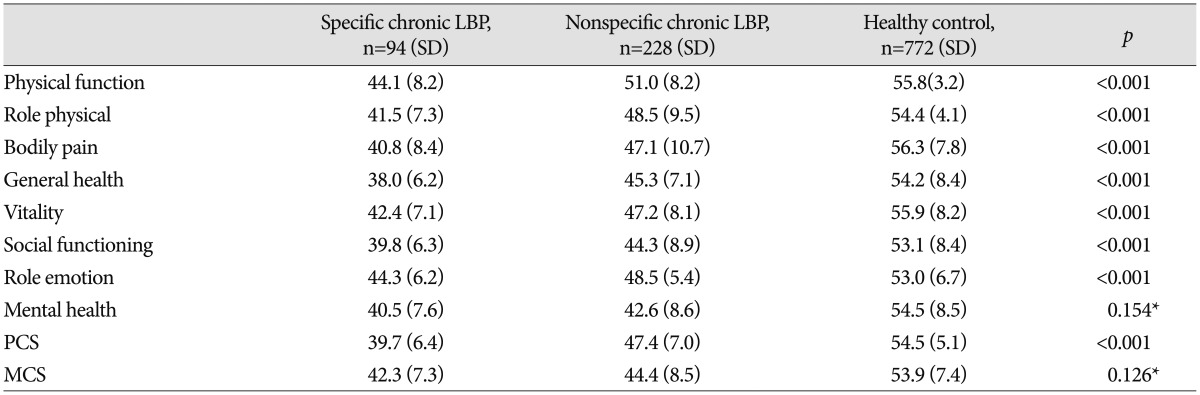
The LTP of chronic LBP was 13.4%. Most (71.7%) of them didn't have any lumbar spinal lesions (i.e., non-specific chronic LBP). The SF-36 subscale and summary scores were significantly lower in subjects with chronic LBP. Between specific and non-specific chronic LBP group, all physical and mental subscale scores were significantly lower in specific chronic LBP group, except mental health (MH) subscale score. In MH subscale and mental component summary score, statistical significant differences didn't appear between two groups (p=0.154, 0.126).
Conclusion
In Korean males 19 years of age, the LTP of chronic LBP was 13.4%, and more than two-thirds were non-specific chronic LBP. Chronic LBP had a significant impact on HRQOL. The presence of lumbar spinal pathoanatomical lesions affected mainly on the physical aspect of HRQOL. It influenced little on the mental health.
Low back pain (LBP) is defined as pain and discomfort localized between the 12th rib and the inferior gluteal folds, with or without referred pain. About 90% of LBP has benign course (i.e., most patients with acute LBP improve within weeks)7,8,30). However, some patients will not recover and will develop chronic LBP.
Chronic LBP, persisting for at least 12 weeks1,31), is one of the greatest adult public health problems. It causes quite considerable individual and social burden in the industrialized world17,23). The life-time prevalence of LBP in adults is reported to be as high as 84%3). In late adolescence, the prevalence of LBP varies from 30% to 70%, and some authors report that adolescent LBP is a strong predictor for adult chronic LBP2,12,15,20,26,36). Therefore, it is important that precise diagnosis and proper management for chronic LBP in late adolescents and young adults.
There are growing evidences that chronic LBP is regarded as biopsychosocial perspective10,25). Recent studies suggested the approach to management of patients with chronic LBP do not restrict to tissue damage or structural abnormality. It proposed to extend the treatment paradigm for psychological factors and the demand for the health care1,3,19). Therefore, it would be useful to understand health-related quality of life (HRQOL) in patients with chronic LBP. The identification of the higher impact factors in chronic LBP among the variables of HRQOL is helpful to make proper treatment strategies.
The aims of present study were 1) to estimate the life-time prevalence of chronic LBP in young Korean males and the proportion of nonspecific chronic LBP; 2) to determine the impact of chronic LBP on HRQOL; and 3) to determine the difference of HRQOL between specific chronic LBP and non-specific chronic LBP.
Korean males are obligated to have physical examinations for the conscript at the age of 19 years. Seoul regional military manpower administration conducts physical examination for the conscript about seventeen thousand males in every year. Ten specialists (internal medicine, orthopedics, neurosurgery, psychiatry, ophthalmology, dermatology, otorhinolaryngology, dentistry, and radiology) carry out physical examination. Examinees are conscripted when they have no major ailments or symptoms according to the Korean military service law. In cases with severe diseases or symptoms, the examinees are decided to serve as a public service worker, or exemption from the conscription.
The flow chart summarized the overall study design (Fig. 1). We examined 3331 Korean males of 19 years old for the conscript from November 4, 2013 to November 29, 2013. We explained about this study, and informed that the results of their questionnaire did not influence on the conscript. We excluded 152 examinees who refused to participate this study. We also excluded 768 participants who have surgical, medical, or psychological diseases diagnosed by the corresponding specialists in each department in order to foreclose the influence for HRQOL. Ethical approval was granted from Soonchunhyang University Human Research Ethics Committee (SCHCA 2013-11-010). We included 2411 consecutive subjects in this study. Body mass index (BMI) and educational status gathered at the first time. We performed self-reported questionnaire for LBP experience and chronicity. One member of our study team explained the questionnaire to each participant during physical examination. The participants were asked simple binary questions : 1) Have you ever been experienced low back pain?; 2) If it was, has your low back pain been persisted more than three months? The subjects who answered "NO" on the first question were categorized into the healthy control group. The subjects who answered "YES" on both questions were grouped into the chronic LBP group. The subjects who answered "YES" on the first question and "NO" on the second question were grouped into the non-chronic LBP group.
To assess the impact of chronic LBP on HRQOL, we performed the Korean version of Short-Form Health-survey-36 (SF-36)11) in the healthy controls and the chronic LBP group. SF-36 is a widely used generic HRQOL instrument to assess the eight health phenomena : 4 subscales to reflect physical health, physical function; role physical; bodily pain; general health, and 4 subscales to reflect mental health, vitality (VT); social functioning (SF); role emotion (RE); mental health (MH). These subscales summarized to score physical component summary (PCS) and mental component summary (MCS). The scores of subscales and summaries were transformed norm-based scoring to have the same average (50 points) and the same standard deviation (10 points). If a participant was missing 1 item, it was imputed from the average of the other 8 items, but no score was calculated for those participants missing more than 1 item.
Radiological evaluations were performed in the chronic LBP group. All subjects of the chronic LBP group were examined by plain radiography of the lumbar spine after physical examinations by a neurosurgeon and an orthopedic surgeon. CT scans or MRIs of the lumbar spine were also performed, if needed. All radiographic images were read by two independent radiologists. When there were any definite spinal pathoanatomical lesions in the radiological examinations, we classified the subjects as the specific chronic LBP group. When there were no recognizable or specific spinal pathologic lesions, we classified them as the non-specific chronic LBP group. Since spondylolysis, spondylolisthesis, or spina bifida occulta in plain radiography or CT scans did not explain the exact cause of LBP, we classified them as the non-specific lesions.
Statistical analysis was performed using SPSS statistics version 19.0 software package (SPSS Inc., Chicago, IL, USA). To determine the life time prevalence of chronic LBP, frequency analysis and bootstrapping were performed in all participants of self-reported questionnaire. Chi-squared test in nominal variables and Kruskal-Wallis test in scale variables were performed to test relationships among nonspecific, specific chronic LBP group, and healthy control group. ANOVA was used for variance analysis of the results. The Bonferroni correction was used for counteract the problem of multiple comparisons. To determine the independent impact of SF-36 summary score (PCS and MCS, respectively) in subjects with chronic LBP, univariate multiple regression model was used with BMI, educational status, and radiologic abnormalities as independent variables. A difference was considered statistically significant at p value of <0.05.
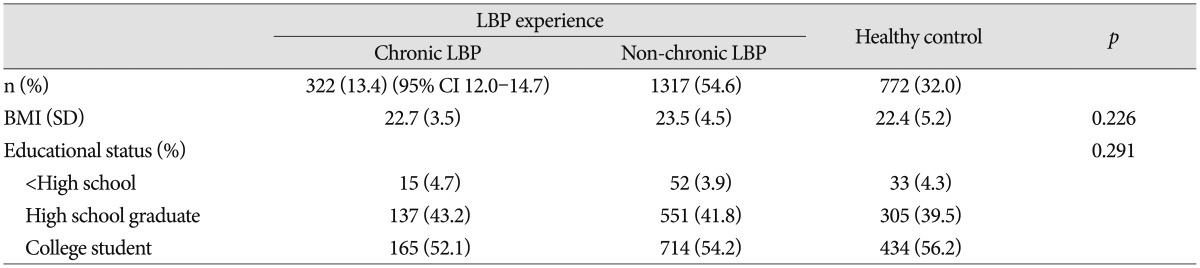
Overall 1317 (54.6%) in 2411 participants answered they have experienced with LBP during their life-time. A total of 322 (proportion, 13.4%; 95% CI 12.0-14.7%) out of 2411 participants reported chronic LBP. Seven hundreds and seventy two participants were answered that did not experience LBP, and they clas-sified as healthy control. BMI and educational status were not significantly different among three groups (p=0.226 and 0.291, respectively) (Table 1).
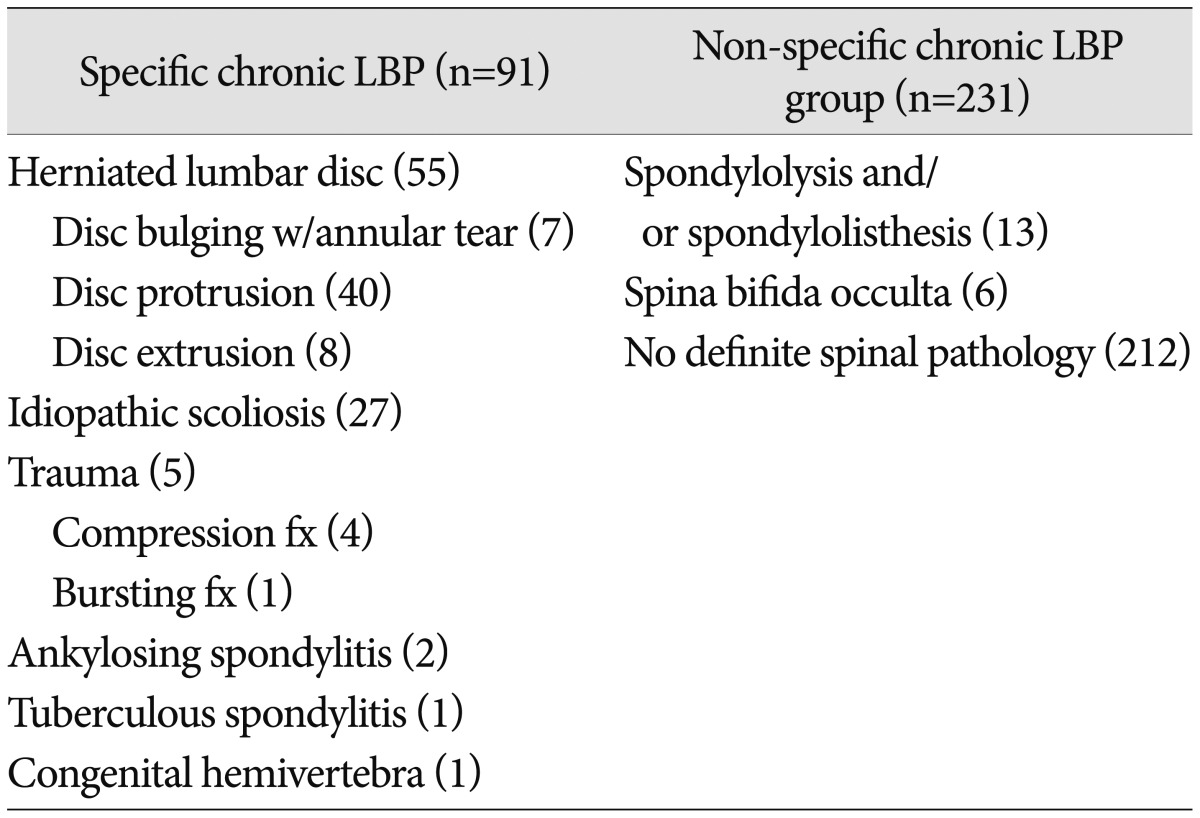
In 322 subjects with chronic LBP, radiological evaluations showed specific spinal pathoanatomical lesions in 91 (28.3%) subjects. Remaining 231 (71.7%) were classified as the non-specific chronic LBP group. Herniated lumbar disc (HLD) was the most common attributable pathoanatomical lesion of the chronic LBP (Table 2).
Table 3 showed SF-36 subscales and summary scores in the specific chronic LBP, the non-specific chronic LBP, and the healthy controls. The SF-36 subscale score and summary score in subjects with chronic LBP were significantly lower than the healthy control. Between the specific and non-specific chronic LBP groups, all but one subscale, MH subscale, were significantly lower in the specific chronic LBP group. In MH subscale score, statistical significant differences did not appear between two groups according to Bonferroni correction (p=0.154). And the mean score gap was just 2.1 points between two groups. Because of MCS score summarized with VT, SF, RE, and MH subscales, there was no statistically significant differences in MCS score, either (p=0.126).
We performed multiple regression analysis in subjects with chronic LBP to determine independent impact of PCS and MCS score adjusting for BMI, educational status and radiologic abnormality. The adjusted difference in PCS score between subjects with radiologic abnormality and those without was 6.8 points (R square=0.034, 95% CI=4.6 to 8.9, p<0.001). However, the difference was not reported in MCS score between subjects with chronic LBP with and without radiologic abnormality (p=0.073).
In this study, the proportion of LBP experience and the life-time prevalence of chronic LBP in aged 19 Korean males were 53.6% and 13.4%, respectively. Many studies attest to the high frequency and wide ranges of back complaints in any given society. One systematic review of literature from 1966 to 1998 identified the life-time prevalence of LBP ranged from 11 to 84%33). Another study reported that the life-time prevalence of LBP in cross-sectional studies ranged from 49 to 70%32). The life-time prevalence of LBP in children and adolescents raged from 30 to 51%4). However, these studies did not give a specific prevalence of chronic LBP. There is some attempt to estimate the epidemiology of chronic LBP. In 2009, Jhun and Park16) reported that over 2 million (5.7%) Korean adults have experienced chronic LBP during the year and the 12-month period prevalence of chronic LBP in 20-29 aged population was 2.4% after analyzing the data from the fourth Korea National Health and Nutrition Examination Survey. Freburger et al.9) reported that the chronic LBP prevalence in 19-89 aged adults was 10.2% though a cross sectional study in North Carolina. Best estimates suggested that the prevalence of chronic LBP was about 23%1). Many studies revealed that chronic LBP was more frequently occurrence in female6,37) and older age group9,16,22,32,33). We expected that this study population would be a lower risk group of chronic LBP, since they are young males. Although we repeatedly announced that the survey itself will not affect on the conscript, we could not rule out the possibility that some of the people surveyed might exaggerate their symptoms in order to avoid the conscription. As other possible reasons, in recent health care system in Korea, the health care accessibility is much easier and there are plenty of information about public knowledge of LBP via medicalization, media, and internet. In spite of a low risk group, high prevalence of chronic LBP may draw in these respects.
We examined the impact of chronic LBP on HRQOL using SF-36. Especially, we reported the difference of HRQOL between the specific and non-specific chronic LBP groups. This is the first report, to our knowledge, that comparing the difference of HRQOL between the specific and non-specific chronic LBP in young male adults.
Chronic LBP is typically classified as being 'specific' or 'non-specific'. It is known that approximately 90% of patients with LBP will have no definite causes of their pain32). Non-specific chronic LBP generally defined as symptoms without clear specific pathoanatomical causes, such as HLD, infection, trauma, tumor, inflammatory disorder, osteoporosis, or structural deformity. However, there are no established diagnostic criteria for specific and non-specific chronic LBP. The authors performed radiological evaluations for 322 consecutive subjects with chronic LBP. We included HLDs, bulging discs with annular tear, idiopathic scoliosis, compression or bursting fractures, inflammatory disorders, infections, and congenital deformities as specific pathoanatomical lesions of the spine which could cause back pain symptoms. We classified spondylolysis or spondylolisthesis (13 subjects), and spina bifida occulta (6 subjects) as the non-specific chronic LBP. A considerable proportion of patients with such anatomic abnormalities are asymptomatic28). Incomplete closure of posterior arch of L5 and/or S1 vertebra is by itself of no clinical significance5). As a result, 231 (71.7%) were classified as non-specific chronic LBP. Back pain symptoms are frequently poorly correlated to pathology or radiographic finding1). Therefore, clinicians should be aware of the incidence and characteristics of specific back pain, and should be noted that a not inconsiderable number of patients with chronic LBP did not have recognizable, known specific pathology which could cause of their symptoms.
According to our results of SF-36 survey, the subjects with chronic LBP had significant reduction on their HRQOL. All subscale and summary score were significantly lower without reference to specific or non-specific group than healthy control. In comparison with non-specific chronic LBP, physical components of SF-36 were significantly lower in specific chronic LBP group. In other words, specific chronic LBP significantly reduces the physical activities than non-specific chronic LBP. It is supported in that a recent study, specific LBP group suffered more pain and showed significantly higher score of disability scales than non-specific LBP group18). MH subscale score was the only subscale which did not show statistical difference between specific and non-specific chronic LBP group. And the mean score gap was just 2.1 points. The concept of minimal clinical important difference (MCID) is referred to the smallest difference in score14). A difference smaller than MCID is considered as worthless regardless of whether it has statistically significant or not. The MCID for SF-36 is typically in the range of 3 to 5 points27). Because of MCS score summarized with VT, SF, RE, and MH subscales, MCS score was not different between specific and non-specific chronic LBP, either. The lowest MH subscale score implied feelings of nervousness and depression, and lowest MCS score can be interpreted as frequent psychological distress, social and role disability due to emotional problems. MH subscale score is the most valid measure of mental health, and is useful in screening for psychiatric disorders34). Therefore, it can be suggested that the spinal pathoanatomical lesions influence more on the physical aspects of HRQOL than the mental aspects.
Mental health is affected by chronic pain itself, not by the spinal pathology. Hart13) described about the "sickness response", which is thought to a survival enhancing strategy that restricts movement and conserves energy for host defenses against to injuries or stressors. Three cytokines-interleukin (IL)-1, IL-6, and tumor necrosis factor-α-have come to be characterized as typical pro-inflammatory cytokines (PICs). The PICs play important roles in sickness response29). The PICs initiate series of cascade of cellular events-inducing and enhancing pain behavior by central nervous system glial cell activation35), developing depressive emotion by alterations of hypothalamus-pituitary-adrenal axis21), leading sleep disturbance by changing serotonin and dopamine secretion24). These evidences indicate that chronic LBP and depres-sion may share common pathophysiology, and PICs act mediator by similar mechanism in both situations. Therefore, it can be said that enhanced pain or depressive mood can occur without tissue injury or pathologic change.
Due to the cross-sectional nature of our study, these findings need to be validated in prospective settings. And other predictors of reduced HRQOL in chronic LBP should also be evaluated.
Our study findings confirm the high prevalence of chronic LBP in age of 19 years Korean males, even though they might belong to the low risk group. And among them, more than two thirds did not have any spinal pathoanatomical lesions which might cause their symptoms. These results implied the clinical importance and seriousness of chronic LBP in young adults. The HRQOL was significantly more decreased in subjects with chronic LBP than the healthy control. The physical component score of SF-36 was significantly lower in the specific chronic LBP group than in the non-specific chronic LBP group. However, MH subscale and MCS score were not different between two groups. In other words, the mental health was reduced in subjects with chronic LBP whether they have spinal pathoanatomical lesion or not.
References
1. Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006; 15(Suppl 2):S192–S300. PMID: 16550448.

2. Balagué F, Ferrer M, Rajmil L, Pont Acuña A, Pellisé F, Cedraschi C. Assessing the association between low back pain, quality of life, and life events as reported by schoolchildren in a population-based study. Eur J Pediatr. 2012; 171:507–514. PMID: 21979564.

3. Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet. 2012; 379:482–491. PMID: 21982256.

4. Balagué F, Troussier B, Salminen JJ. Non-specific low back pain in children and adolescents: risk factors. Eur Spine J. 1999; 429–438. PMID: 10664299.
5. Boone D, Parsons D, Lachmann SM, Sherwood T. Spina bifida occulta : lesion or anomaly? Clin Radiol. 1985; 36:159–161. PMID: 3905193.
6. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006; 10:287–333. PMID: 16095934.

7. Buchbinder R, Underwood M. Prognosis in people with back pain. CMAJ. 2012; 184:1229–1230. PMID: 22586338.

8. Carey TS, Garrett J, Jackman A, McLaughlin C, Fryer J, Smucker DR. The outcomes and costs of care for acute low back pain among patients seen by primary care practitioners, chiropractors, and orthopedic surgeons. The North Carolina Back Pain Project. N Engl J Med. 1995; 333:913–917. PMID: 7666878.

9. Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009; 169:251–258. PMID: 19204216.

10. Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain : scientific advances and future directions. Psychol Bull. 2007; 133:581–624. PMID: 17592957.

11. Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M. Development of the Korean version of Short-Form 36-Item Health Survey : health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med. 2004; 203:189–194. PMID: 15240928.

12. Harreby M, Neergaard K, Hesselsøe G, Kjer J. Are radiologic changes in the thoracic and lumbar spine of adolescents risk factors for low back pain in adults? A 25-year prospective cohort study of 640 school children. Spine (Phila Pa 1976). 1995; 20:2298–2302. PMID: 8553117.

13. Hart BL. Biological basis of the behavior of sick animals. Neurosci Biobehav Rev. 1988; 12:123–137. PMID: 3050629.

14. Hays RD, Woolley JM. The concept of clinically meaningful difference in health-related quality-of-life research. How meaningful is it? Pharmacoeconomics. 2000; 18:419–423. PMID: 11151395.

15. Hestbaek L, Leboeuf-Yde C, Kyvik KO, Manniche C. The course of low back pain from adolescence to adulthood: eight-year follow-up of 9600 twins. Spine (Phila Pa 1976). 2006; 31:468–472. PMID: 16481960.
16. Jhun HJ, Park JY. Estimated number of Korean adults with back pain and population-based associated factors of back pain : data from the fourth Korea national health and nutrition examination survey. J Korean Neurosurg Soc. 2009; 46:443–450. PMID: 20041054.

17. Katz JN. Lumbar disc disorders and low-back pain : socioeconomic factors and consequences. J Bone Joint Surg Am. 2006; 88(Suppl 2):21–24. PMID: 16595438.

18. Kim GM, Yi CH, Cynn HS. Factors influencing disability due to low back pain using the Oswestry Disability Questionnaire and the Quebec Back Pain Disability Scale. Physiother Res Int. 2014; 5. 01. [Epub]. http://dx.doi.org/10.1002/pri.1591.

19. Krismer M, van Tulder M. Low Back Pain Group of the Bone and Joint Health Strategies for Europe Project. Strategies for prevention and management of musculoskeletal conditions. Low back pain (non-specific). Best Pract Res Clin Rheumatol. 2007; 21:77–91. PMID: 17350545.
20. Leboeuf-Yde C, Kyvik KO. At what age does low back pain become a common problem? A study of 29,424 individuals aged 12-41 years. Spine (Phila Pa 1976). 1998; 23:228–234. PMID: 9474731.
21. Leonard BE. The immune system, depression and the action of antidepressants. Prog Neuropsychopharmacol Biol Psychiatry. 2001; 25:767–780. PMID: 11383977.

22. Loney PL, Stratford PW. The prevalence of low back pain in adults : a methodological review of the literature. Phys Ther. 1999; 79:384–396. PMID: 10201544.

23. Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA. American Society of Interventional Pain Physicians. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009; 12:E35–E70. PMID: 19668291.
24. Marty M, Rozenberg S, Duplan B, Thomas P, Duquesnoy B, Allaert F. Section Rachis de la Société Française de Rhumatologie. Quality of sleep in patients with chronic low back pain: a case-control study. Eur Spine J. 2008; 17:839–844. PMID: 18389288.

25. O'Sullivan PB, Beales DJ, Smith AJ, Straker LM. Low back pain in 17 year olds has substantial impact and represents an important public health disorder: a cross-sectional study. BMC Public Health. 2012; 12:100. PMID: 22304903.
26. Pellisé F, Balagué F, Rajmil L, Cedraschi C, Aguirre M, Fontecha CG, et al. Prevalence of low back pain and its effect on health-related quality of life in adolescents. Arch Pediatr Adolesc Med. 2009; 163:65–71. PMID: 19124706.

27. Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D. Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics. 1999; 15:141–155. PMID: 10351188.

28. Soler T, Calderón C. The prevalence of spondylolysis in the Spanish elite athlete. Am J Sports Med. 2000; 28:57–62. PMID: 10653544.

29. Strouse TB. The relationship between cytokines and pain/depression : a review and current status. Curr Pain Headache Rep. 2007; 11:98–103. PMID: 17367587.

30. van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006; 15(Suppl 2):S169–S191. PMID: 16550447.

31. van Tulder M, Koes B. Low back pain (chronic). Clin Evid. 2006; 1634–1653. PMID: 16973063.
32. van Tulder M, Koes B, Bombardier C. Low back pain. Best Pract Res Clin Rheumatol. 2002; 16:761–775. PMID: 12473272.

33. Walker BF. The prevalence of low back pain : a systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000; 13:205–217. PMID: 10872758.

34. Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976). 2000; 25:3130–3139. PMID: 11124729.

35. Watkins LR, Maier SF. Immune regulation of central nervous system func-tions: from sickness responses to pathological pain. J Intern Med. 2005; 257:139–155. PMID: 15656873.

36. Watson KD, Papageorgiou AC, Jones GT, Taylor S, Symmons DP, Silman AJ, et al. Low back pain in schoolchildren : occurrence and characteristics. Pain. 2002; 97:87–92. PMID: 12031782.
37. Yao W, Mai X, Luo C, Ai F, Chen Q. A cross-sectional survey of nonspecific low back pain among 2083 schoolchildren in China. Spine (Phila Pa 1976). 2011; 36:1885–1890. PMID: 21270687.

Fig. 1
Summarized overall study design and inclusion/exclusion criteria. CLBP : chronic low back pain, LBP : low back pain, SF-36 survey : Short-Form Health-survey-36.

Table 1
Life-time prevalence of CLBP and baseline characteristics of 2411 aged 19 Korean male subjects




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download