Abstract
Sarcoidosis is a systemic disease of unknown etiology that may affect any organ in the body. The nervous system is involved in 5-16% of cases of sarcoidosis. Here, we report a case of intramedullary sarcoidosis presenting with delayed spinal cord swelling after laminoplasty for the treatment of compressive cervical myelopathy. A 56-year-old woman was admitted to our hospital complaining of upper extremity pain and gait disturbance. The patient had undergone laminoplasty for compressive cervical myelopathy 3 months previously. Follow-up magnetic resonance imaging revealed a large solitary intramedullary lesion with associated extensive cord swelling, signal changes, and heterogeneous enhancement of spinal cord from C2 to C7. Spinal cord biopsy revealed non-necrotizing granulomas with signs of chronic inflammation. The final diagnosis of sarcoidosis was based upon laboratory data, imaging findings, histological findings, and the exclusion of other diagnoses. Awareness of such presentations and a high degree of suspicion of sarcoidosis may help arrive at the correct diagnosis.
Sarcoidosis is a multisystem granulomatous disease of unknown origin that affects multiple organs; its pathological hallmark is the presence of non-caseating epithelioid granulomas3,8,26). Lesions commonly occur in the lungs, lymphatic system, eyes, skin, liver, spleen, salivary glands, heart, nervous system, muscles, and bone11,21).
Neurosarcoidosis is a rare manifestation that occurs in 5% of patients with systemic sarcoidosis2). It can manifest as intramedullary lesions, intradural extramedullary or extradural lesions, cauda equina syndrome, or arachnoiditis23). Primary spinal cord involvement in sarcoidosis is very uncommon, estimated to occur in only 0.3-0.4% of patients with systemic sarcoidosis5).
Here, we report a case of spinal cord sarcoidosis without systemic symptoms. The patient presented with delayed spinal cord swelling after laminoplasty for the treatment of compressive cervical myelopathy. We also discuss the clinical symptoms, laboratory tests, and imaging findings that assisted in the differential diagnosis of spinal cord sarcoidosis.
A 56-year-old woman presented to our institution with a 1-month history of bilateral hand tingling and hypoesthesia. She had no history of spinal trauma. Computed tomography (CT) revealed ossification of the posterior longitudinal ligament (OPLL) from C3 to C7. Cervical magnetic resonance imaging (MRI) revealed severe cord compression and high signal intensity at C4-5. At that time, the patient was diagnosed with compressive myelopathy due to OPLL and disc herniation. An open door laminoplasty was performed from C3 to C7 using centerpiece miniplates (Medtronic Sofamor Danek, Minneapolis, MN, USA). Postoperative MRI confirmed disappearance of the spinal cord compression and sufficient canal expansion after laminoplasty. Her preoperative signs and symptoms were completely alleviated (Fig. 1).
Three months after surgery, the patient was re-admitted to our hospital because of pain in the upper extremities and gait disturbance, which she had been experiencing for 1 month. On neurological examination, her C5 elbow flexors and C6 wrist extensors were weak (grade 4). Right knee extension was also weak (grade 4). The patient felt numbness and pain in both hands and in the right forearm. Hoffman's sign was positive in both hands. The patient showed gait disequilibrium and ataxia. Results of routine laboratory tests, including assays for the estimation of C-reactive protein levels, erythrocyte sedimentation rate, and serum total immunoglobulin E levels, were within normal ranges. Polymerase chain reaction for Mycobacterium tuberculosis and Herpes simplex virus type 1 yielded negative results. Cerebrospinal fluid (CSF) analysis showed a cell count of 100/µL (mononuclear cells, 30/µL; lymphocytes, 68/µL; polynuclear cells, 2/µL). The serum level of angiotensin-converting enzyme (ACE) was mildly elevated at 48.3 U/L. The patient was negative for anti-aquaporin-4 antibodies.
Follow-up cervical spine MRI revealed a large intramedullary lesion with associated cord swelling extending from C2 to C7, signal changes, and heterogeneous enhancement in the spinal cord lesion (Fig. 2). Positron emission tomography-CT (PET-CT) showed linear fludeoxyglucose (FDG) uptake from the C3 to C6, varying FDG uptake in multiple lymph nodes, and increased FDG uptake in a nodule in the right lower lobe of the lung. Malignancy, lung cancer or lymphoma, was suspected. Therefore, thoracoscopic lymph node biopsy was performed, but no evidence of malignancy was noted. A subsequent spinal cord biopsy revealed non-necrotizing granulomas with signs of chronic inflammation (Fig. 3).
Finally, intramedullary spinal cord sarcoidosis was diagnosed, and steroid therapy was initiated. Despite high-dose steroid therapy, the patient's symptoms persisted. Furthermore, her muscle weakness aggravated and she developed urinary incontinence. Therefore, the patient was also treated with methotrexate. Follow-up MRI performed 3 months after the biopsy showed shrinkage of the enhanced lesion and improvement in the cord swelling (Fig. 4). Six months after the biopsy, a neurologic examination demonstrated modest and partial improvement in the muscle power of the elbow, wrist, and lower extremities, whereas the decreased perception of a pinprick, temperature, and touch as well as paresthesia from C5 downward remained unchanged. Once able to stand on crutches, the patient was transferred to a rehabilitation center.
Neurosarcoidosis is an uncommon disease that affects only 5-16% of patients with sarcoidosis24). The incidence of spinal sarcoidosis is estimated to be 0.43-0.8%3), and the disease can present as intramedullary lesions (35%), intradural-extramedullary lesions (35%), a combination of these two lesion types (23%), or extradural lesions (7%)7). Men are afflicted more frequently, and the disease is more common in African-American and Scandinavian populations but rare in South Asian populations3,7). One case series report, which included a review of the literature, reported that the mean age of patients with spinal sarcoidosis was 42.8 years7).
Sarcoidosis has no specific symptoms for its diagnosis. Common symptoms include fatigue and weight loss. Symptoms originating from spinal cord injuries, such as muscle weakness, hypoesthesia, pain, myelopathy, and palsy, can be attributed to spinal cord damage itself.
Laboratory tests alone are not conclusive but can help distinguish sarcoidosis from other diseases. In our case, the serum ACE level was slightly higher than normal, but this level is elevated in only 23.5% of patients with sarcoidosis25). Further, an elevated ACE level is not specific and is observed in other disease conditions involving the spinal cord, such as tuberculosis1,22). Neuromyelitis optica (NMO) is also an important cause of demyelinating spinal cord lesions extending over three vertebral segments. Approximately 90% of patients with NMO are positive for aquaporin-4 antibodies15). MRI is a useful technique for diagnosing sarcoidosis. The most common MRI finding is leptomeningeal enhancement, which is observed in 40-67% of patients with neurosarcoidosis12,15). Other MRI findings include patchy intraparenchymal enhancement, an increased T2 signal indicative of cord edema, and cord atrophy. Enhancing dural lesions are relatively uncommon22). However, it is very difficult to distinguish spinal cord sarcoidosis from tumors, transverse myelitis, tuberculosis, and especially multiple sclerosis10).
Transverse myelitis, a disorder caused by spinal cord inflammation, is characterized by neurological dysfunction of the motor and sensory tracts on both sides of the spinal cord. In our case, transverse myelitis was less likely because it is characterized by CSF pleocytosis (>10 cells/mm3)17). Multiple sclerosis is a common cause of intramedullary white matter lesions. The lesions observed in multiple sclerosis are usually small and peripheral; therefore, they are associated with asymmetric signs and symptoms. Multiple sclerosis was not highly suspected in our patient because the radiculopathy and peripheral neuropathy symptoms she experienced are not typical presentations of multiple sclerosis18). Interestingly, the patient previously had cervical OPLL that was treated with laminoplasty. Seichi et al.21) performed follow-up MRI at 3 weeks after laminoplasty in >100 patients to determine the frequency of spinal cord swelling with an intramedullary lesion and the possible mechanism of postoperative motor paresis of the upper extremity. We consider postoperative complications a possible reason for the edema and increased signal intensity on MRI. Furthermore, intramedullary enhancement may be indicative of spinal sarcoidosis7).
The key histological finding for diagnosing sarcoidosis is the presence of non-caseating granulomas with negative findings on mycobacterial and fungal staining3). Granulomas of the spinal cord and brain are smaller than systemic lesions and consist of fewer giant cells; therefore, non-caseating granulomas are difficult to detect11). Finally, the diagnosis of sarcoidosis was based on laboratory data, imaging findings, histology, and the exclusion of other diagnoses.
Medical treatment is the first choice for sarcoidosis. Systemic corticosteroids and immunosuppressive therapy are standard options; however, such treatment is only partially effective, especially in spinal cord sarcoidosis4,9,16,19,20,23). Corticosteroids are partially effective : a response to steroids alone is observed in only 29% of patients with neurosarcoidosis14). Further, no response to current conventional immunosuppressant treatments is observed in 20-40% of patients with neurosarcoidosis8). In our case, the patient was treated with both steroid and immunosuppressant therapy. Fortunately, she responded well to high-dose corticosteroids and immunosuppressants.
In our case, maintenance of motor function with evidence of radiological improvement was demonstrated at the 6-month follow-up. Clinical and laboratory investigation of a large group of patients with neurosarcoidosis followed up for at least 5 years showed that neurological involvement at the onset is associated with a poor outcome and less favorable disease course6). However, in cases of spinal sarcoidosis, steroid therapy may be associated with a favorable outcome13).
Diagnosing spinal cord sarcoidosis is quite difficult. The symptoms, signs, and MRI findings of intramedullary sarcoidosis do not differ from those of intramedullary tumors, transverse myelitis, and multiple sclerosis. Being aware of the possibility of sarcoidosis is important to avoid its misdiagnosis as cervical non-tumorous myelitis, a tumor, or infection. As observed in our case, delayed spinal cord swelling after cervical laminoplasty may indicate the possibility of neurosarcoidosis. Awareness of such presentations and a high degree of suspicion of sarcoidosis may assist clinicians in making an accurate diagnosis.
References
1. Allen RK. A review of angiotensin converting enzyme in health and disease. Sarcoidosis. 1991; 8:95–100. PMID: 1670005.
2. Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H Jr, Bresnitz EA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. 2001; 164(10 Pt 1):1885–1889. PMID: 11734441.

3. Bradley DA, Lower EE, Baughman RP. Diagnosis and management of spinal cord sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2006; 23:58–65. PMID: 16933471.
4. Caneparo D, Lucetti C, Nuti A, Cipriani G, Tessa C, Fazzi P, et al. A case of sarcoidosis presenting as a non-specific intramedullary lesion. Eur J Neurol. 2007; 14:346–349. PMID: 17355560.

6. Ferriby D, de Seze J, Stojkovic T, Hachulla E, Wallaert B, Destée A, et al. Long-term follow-up of neurosarcoidosis. Neurology. 2001; 57:927–929. PMID: 11552036.

7. Hayat GR, Walton TP, Smith KR Jr, Martin DS, Manepalli AN. Solitary intramedullary neurosarcoidosis : role of MRI in early detection. J Neuroimaging. 2001; 11:66–70. PMID: 11198533.
8. Hoitsma E, Faber CG, Drent M, Sharma OP. Neurosarcoidosis : a clinical dilemma. Lancet Neurol. 2004; 3:397–407. PMID: 15207796.
9. Joseph FG, Scolding NJ. Neurosarcoidosis : a study of 30 new cases. J Neurol Neurosurg Psychiatry. 2009; 80:297–304. PMID: 18977817.
10. Junger SS, Stern BJ, Levine SR, Sipos E, Marti-Masso JF. Intramedullary spinal sarcoidosis : clinical and magnetic resonance imaging characteristics. Neurology. 1993; 43:333–337. PMID: 8437698.

11. Kim SH, Lee SW, Sung SK, Son DW. Treatment of hydrocephalus associated with neurosarcoidosis by multiple shunt placement. J Korean Neurosurg Soc. 2012; 52:270–272. PMID: 23115677.

12. Kumar N, Frohman EM. Spinal neurosarcoidosis mimicking an idiopathic inflammatory demyelinating syndrome. Arch Neurol. 2004; 61:586–589. PMID: 15096410.

13. Levivier M, Brotchi J, Balériaux D, Pirotte B, Flament-Durand J. Sarcoidosis presenting as an isolated intramedullary tumor. Neurosurgery. 1991; 29:271–276. PMID: 1886670.

14. Lexa FJ, Grossman RI. MR of sarcoidosis in the head and spine : spectrum of manifestations and radiographic response to steroid therapy. AJNR Am J Neuroradiol. 1994; 15:973–982. PMID: 8059671.
15. Lower EE, Broderick JP, Brott TG, Baughman RP. Diagnosis and management of neurological sarcoidosis. Arch Intern Med. 1997; 157:1864–1868. PMID: 9290546.

16. Lury KM, Smith JK, Matheus MG, Castillo M. Neurosarcoidosis--review of imaging findings. Semin Roentgenol. 2004; 39:495–504. PMID: 15526533.

17. Maroun FB, O'Dea FJ, Mathieson G, Fox G, Murray G, Jacob JC, et al. Sarcoidosis presenting as an intramedullary spinal cord lesion. Can J Neurol Sci. 2001; 28:163–166. PMID: 11383944.

18. Miller D, Barkhof F, Montalban X, Thompson A, Filippi M. Clinically isolated syndromes suggestive of multiple sclerosis, part I : natural history, pathogenesis, diagnosis, and prognosis. Lancet Neurol. 2005; 4:281–288. PMID: 15847841.

19. Scott TF, Frohman EM, De Seze J, Gronseth GS, Weinshenker BG. Therapeutics and Technology Assessment Subcommittee of American Academy of Neurology. Evidence-based guideline : clinical evaluation and treatment of transverse myelitis : report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2011; 77:2128–2134. PMID: 22156988.

20. Scott TF, Yandora K, Valeri A, Chieffe C, Schramke C. Aggressive therapy for neurosarcoidosis : long-term follow-up of 48 treated patients. Arch Neurol. 2007; 64:691–696. PMID: 17502468.
21. Seichi A, Takeshita K, Kawaguchi H, Nakajima S, Akune T, Nakamura K. Postoperative expansion of intramedullary high-intensity areas on T2-weighted magnetic resonance imaging after cervical laminoplasty. Spine (Phila Pa 1976). 2004; 29:1478–1482. discussion 1482. PMID: 15223942.

22. Stern BJ. Neurological complications of sarcoidosis. Curr Opin Neurol. 2004; 17:311–316. PMID: 15167067.

23. Terushkin V, Stern BJ, Judson MA, Hagiwara M, Pramanik B, Sanchez M, et al. Neurosarcoidosis : presentations and management. Neurologist. 2010; 16:2–15. PMID: 20065791.
24. Varron L, Broussolle C, Candessanche JP, Marignier R, Rousset H, Ninet J, et al. Spinal cord sarcoidosis : report of seven cases. Eur J Neurol. 2009; 16:289–296. PMID: 19170748.
25. Vinas FC, Rengachary S. Diagnosis and management of neurosarcoidosis. J Clin Neurosci. 2001; 8:505–513. PMID: 11683596.

26. Zajicek JP, Scolding NJ, Foster O, Rovaris M, Evanson J, Moseley IF, et al. Central nervous system sarcoidosis--diagnosis and management. QJM. 1999; 92:103–117. PMID: 10209662.

Fig. 1
A : A preoperative T2-weighted sagittal magnetic resonance imaging (MRI) scan shows marked spinal cord compression from C5 to C8 and an enhanced lesion at the C5-7 vertebral body. B : A postoperative T2-weighted sagittal MRI scan shows disappearance of the spinal cord compression from C5 to C8.

Fig. 2
T2-weighted (A) and T1-weighted (B) follow-up magnetic resonance imaging (MRI) scans at readmission show edematous expansion of the spinal cord and enhanced nodules involving the C4 to C6 levels of the spinal cord. A gadolinium-enhanced T1-weighted MRI scan shows enhancement at multiple vertebra and heterogeneous intramedullary enhancement extending from C3 to C6 (C).

Fig. 3
Microscopic examination revealed several granulomas and central aggregation of epithelioid histiocytes with infiltration of lymphocytes at the periphery, consistent with non-caseating granuloma observed in sarcoidosis (hematoxylin and eosin staining, 400×).
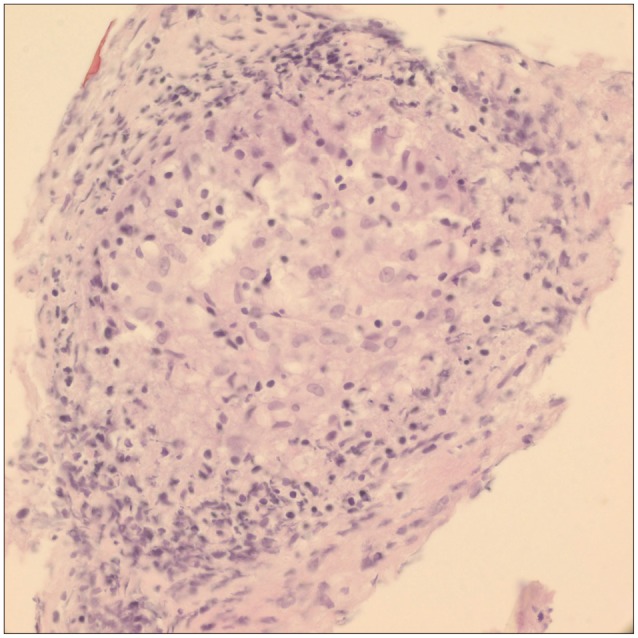
Fig. 4
T2-weighted (A) and T1-weighted (B) follow-up magnetic resonance imaging scans acquired after steroid therapy show that the nodule at the spinal cord is no longer enhanced and expansion of the spinal cord. A gadolinium-enhanced T1-weighted image shows that the enhanced nodule at the site of the spinal lesion is reduced in size (C).





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download