Abstract
Neurosurgeons have been trying to reduce surgical invasiveness by applying minimally invasive keyhole approaches. Therefore, this paper clarifies the detailed surgical technique, its limitations, proper indications, and contraindications for a superciliary keyhole approach as a minimally invasive modification of a pterional approach. Successful superciliary keyhole surgery for unruptured aneurysms requires an understanding of the limitations and the use of special surgical techniques. Essentially, this means the effective selection of surgical indications, usage of the appropriate surgical instruments with a tubular shaft, and refined surgical techniques, including straightforward access to the aneurysm, clean surgical dissection, and the application of clips with an appropriate configuration. A superciliary keyhole approach allows unruptured anterior circulation aneurysms to be clipped safely, rapidly, and less invasively on the basis of appropriate surgical indications.
For unruptured anterior circulation aneurysms, a superciliary keyhole approach using a supraorbital mini-craniotomy, rather than a pterional approach, is invariably limited due to the small cranial opening. Notwithstanding, most anterior circulation aneurysms can still be clipped safely, rapidly, and less invasively using a superciliary approach based on appropriate indications and refined surgical techniques4,5,6,11,12,13,15,16).
Such proper indications and contraindications, along with the detailed surgical technique and its limitations, are presented herein. This report is based on the author's experience in more than 400 cases of a superciliary keyhole approach for unruptured aneurysms.
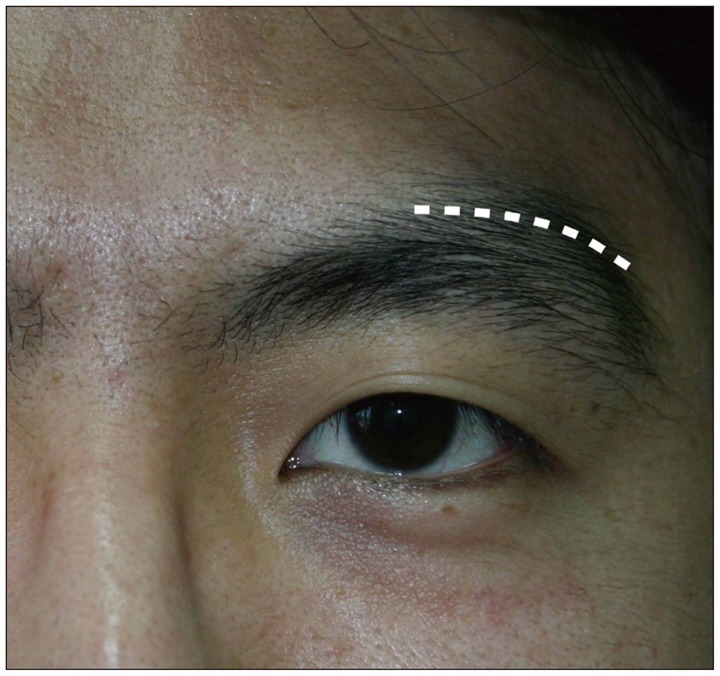
The superciliary skin incision is made starting from the midpupillary line, and located within 1 cm of the supraorbital margin, measuring 3.5 cm in length (Fig. 1). The underlying muscles are the frontalis, corrugator supercilii, and temporalis (Fig. 2). The relevant nerves are the supraorbital nerve and the frontal branch of the facial nerve.
According to a previous nerve conduction study by the current author10), the location of the frontal branch of the facial nerve is normally between 1 and 3 cm above the supraorbital margin as follows : 1) between 2 and 3 cm in 52% of patients, 2) at 1.5 cm in 10% of patients, 3) at 1 cm in 12% of patients, and 4) exhibits a dual innervation with a high (2-3 cm) and low (1-1.5 cm) distribution in 27% of patients.
After the superciliary skin incision, the underlying muscles are cut and widely undermined to facilitate a relatively large craniotomy with only a small skin incision. After drilling a frontobasal lateral burrhole, a supraorbital bone flap with a diameter of <2 cm is created using a high-speed drill with a footplate attachment. Unidirectional skin retraction preceding the drill movement using a retractor held by an assistant can avoid skin damage and allow sufficient space for a craniotomy. Six retraction sutures are then placed at the edge of the skin incision (Fig. 3). The inner edge of the craniotomy above the orbital rim is drilled and beveled, and the frontal floor prominences are flattened. A sphenoid ridge is slightly drilled adjacent to the frontobasal lateral burrhole to expose the sylvian fissure area.
After the dural incision, a narrow brain spatula is slid over the base of the frontal lobe toward the carotid and optic nerve cisterns with the use of an operating microscope. The cisterns are then opened to drain the cerebrospinal fluid, achieve brain relaxation, and obtain an intracranial working space. To expose the supraclinoid internal carotid artery (ICA) aneurysms, dissection of the proximal sylvian fissure allows more frontal lobe retraction and visualization up to the carotid bifurcation.
In the case of middle carotid artery (MCA) aneurysms at the MCA genu, focal (<2 cm) opening of the sylvian fissure at the pars triangularis is sufficient to expose the aneurysm and its parent artery. The sylvian dissection is carried out along the frontal side of the sylvian veins, yet can be limited by the location of the fronto-sylvian veins. Sometimes, division of a few small fronto-sylvian veins is inevitable. For MCA aneurysms proximal to the MCA genu, the sylvian dissection is extended proximally from the pars triangularis.
Furthermore, a superciliary approach can be advocated in the case of inferior- and anterior-directing anterior communicating artery (ACoA) aneurysms, whereas a pterional-transsylvian approach will be favored for superior-directing or high-positioned anterior communicating artery ACoA aneurysms, especially with a large diameter, in order to reduce the brain retraction.
In keyhole surgery using a small cranial opening, certain technical pointers are crucial. The aneurysm should be accessed by the most direct and straightforward route without unnecessary intraoperative navigation. Careful and clean surgical dissection is required to minimize cortical woozing and venous bleeding, avoid a dim operative field, and facilitate surgical processes. The unidirectional application of a clip through the small cranial opening can be a major limitation. Yet, this can be overcome by using aneurysm clips with various configurations, along with gentle mobilization of the parent artery and aneurysm using a suction tip. If an arterial repair is required beyond simple aneurysm clipping, special surgical techniques used in the small and deep operative field are applied7,9).
The dural incision is sutured water-tight, and dural tenting sutures, if needed, are placed along the bone edge using an anchor screw technique8). The bone flap is then fixed in place using low profile, titanium plates and screws. Thereafter, the burrhole and bone gaps around the bone flap are filled with biocompatible material3).
When compared with a pterional approach, the advantages of a superciliary approach are as follows : 1) small operative wound, 2) short operative duration, 3) no intraoperative blood transfusion, 4) rare occurrence of a postoperative epidural hematoma, 5) negligible damage to the temporalis muscle, 6) less wound-related pain, and 7) early return to work and normal life.
However, the major limitations are narrow viewing angles with reduced intraoperative light and reduced maneuverability of the microinstruments, including unidirectional application and coaxial control of the instruments. Thus, an aneurysm clip applier, microscissors, and bipolar coagulation forceps with a tubular shaft are useful to overcome these limitations.
The risk of prolonged or permanent palsy of the frontalis muscle due to injury of the frontal branch of the facial nerve is also related to a superciliary approach14). Yet, this postoperative risk is minimized when the skin incision is located <1 cm of the supraorbital margin and only measures 3.5 cm in length11,12,15). Plus, the operative wound heals well with a good cosmetic appearance, especially in younger patients, although some elderly patients can show a linear dimple at the operative wound and a slightly sagging brow due to loose skin.
A superciliary approach can be applied for unruptured aneurysms with a maximum diameter <15 mm arising at or below the level of the horizontal segments of the anterior cerebral artery and MCA.12) Thus, aneurysms at the supraclinoid ICA, A1, ACoA, and M1 segment including MCA bifurcation are normally favorable for a superciliary approach. However, the aneurysm neck diameter is also a very important consideration to predict the clippability in the case of a superciliary approach.
Table 1 summarizes the effective indications and relative/absolute contraindications of a superciliary approach according to the aneurysm location. The catheter angiograms of the aneurysms favorable and unfavorable for a superciliary approach are depicted in Fig. 4, 5. In the case of ICA aneurysms, a typical posterior communicating artery (PCoA) aneurysm and anterior choroidal artery (AChA) aneurysm, which arise at the lateral or posterolateral wall of an ICA, are the easiest to access and clip using a superciliary approach. In particular, for an unruptured PCoA aneurysm inducing oculomotor nerve palsy, a superciliary approach maximizes the symptomatic resolution and minimizes the surgical invasiveness11). However, in the case of a posterior wall aneurysm of the ICA necessitating an angled fenestrated clip placement, a larger craniotomy is required to allow the appropriate movement and tilting of the aneurysm clip applier. In addition, low-lying supraclinoid or paraclinoid ICA aneurysms that require drilling of the anterior clinoid process also need a larger cranial opening than a supraorbital mini-craniotomy with a small diameter of <2 cm. In such a case, an orbital osteotomy combined with a supraorbital mini-craniotomy can facilitate the drilling work.
For ACoA aneurysms, a superciliary approach only allows subfrontal access, plus the ipsilateral olfactory nerve is more compressed by the brain retractor than in the case of a pterional approach. Thus, while inferior- and anterior-directing ACoA aneurysms can easily be clipped using a superciliary approach, large superior-directing and high-positioned ACoA aneurysms require a pterional-transsylvian approach.
Most MCA aneurysms arising at the M1 segment and MCA bifurcation can be clipped using a superciliary approach. However, if the lesions are located beyond the MCA genu, a larger cranial opening is needed to expose them. A large wide-necked MCA aneurysm requiring aneurysm clip placement in multiple directions will also need a larger craniotomy, along with the case of two adjacent aneurysms requiring clip application in different directions.
Other relative contraindications for a superciliary approach are follows : 1) tendency to form keloids and hypertrophic scars, 2) asymmetric sagging brows, and 3) anticipated emotional stress due to even a small operative wound on the face.
The risk of the postoperative occurrence of a subdural hygroma is high in elderly patients, as in the cases of conventional craniotomies. Thus, all subdural hygromas should be monitored with follow-up computed tomography scans until complete resolution due to the possible conversion to a chronic subdural hematoma.
A superciliary approach can also be applied to some ruptured aneurysms without severe brain swelling. An intravenous mannitol infusion and drainage of cerebrospinal fluid using an intraoperative ventriculostomy or lumbar drainage can achieve brain relaxation and facilitate aneurysm surgery for the patients with mild to moderate brain swelling. Patients with a good clinical grade and small subarachnoid hemorrhage can be treated using this approach without difficulty1,2). However, there is still the risk of unexpected brain swelling and an intraoperative rupture of an aneurysm.
References
1. Brydon HL, Akil H, Ushewokunze S, Dhir JS, Taha A, Ahmed A. Supraorbital microcraniotomy for acute aneurysmal subarachnoid haemorrhage : results of first 50 cases. Br J Neurosurg. 2008; 22:40–45. PMID: 17952722.

2. Chen L, Tian X, Zhang J, Huang Y, Chen E, Lan Q. Is eyebrow approach suitable for ruptured anterior circulation aneurysms on early stage : a prospective study at a single institute. Acta Neurochir. 2009; 151(Wien):781–784. discussion 784. PMID: 19424659.

3. Goh DH, Kim GJ, Park J. Medpor craniotomy gap wedge designed to fill small bone defects along cranial bone flap. J Korean Neurosurg Soc. 2009; 46:195–198. PMID: 19844617.

4. Lan Q, Gong Z, Kang D, Zhang H, Qian Z, Chen J, et al. Microsurgical experience with keyhole operations on intracranial aneurysms. Surg Neurol. 66(Suppl 1):2006; S2–S9. PMID: 16904991.

5. Mitchell P, Vindlacheruvu RR, Mahmood K, Ashpole RD, Grivas A, Mendelow AD. Supraorbital eyebrow minicraniotomy for anterior circulation aneurysms. Surg Neurol. 2005; 63:47–51. discussion 51. PMID: 15639524.

6. Paladino J, Mrak G, Miklić P, Jednacak H, Mihaljević D. The keyhole concept in aneurysm surgery--a comparative study : keyhole versus standard craniotomy. Minim Invasive Neurosurg. 2005; 48:251–258. PMID: 16320184.

7. Park J. Maintenance of cerebral blood flow during microsuture repair of the superior wall of the intracranial internal carotid artery. World Neurosurg. 2013; 80:436.e1–436.e5. PMID: 23563099.

8. Park J. Self-drilling anchor screws for dural tenting sutures : technical note. Surg Neurol. 2009; 72:175–176. PMID: 18617249.
9. Park J, Hwang YH, Kim Y. Extended superciliary approach for middle cerebral artery embolectomy after unsuccessful endovascular recanalization therapy : technical note. Neurosurgery. 2009; 65:E1191–E1194. discussion E1194. PMID: 19934937.
10. Park J, Jung TD, Kang DH, Lee SH. Preoperative percutaneous mapping of the frontal branch of the facial nerve to assess the risk of frontalis muscle palsy after a supraorbital keyhole approach. J Neurosurg. 2013; 118:1114–1119. PMID: 23432514.

11. Park J, Kang DH, Chun BY. Superciliary keyhole surgery for unruptured posterior communicating artery aneurysms with oculomotor nerve palsy : maximizing symptomatic resolution and minimizing surgical invasiveness. J Neurosurg. 2011; 115:700–706. PMID: 21699478.

12. Park J, Woo H, Kang DH, Sung JK, Kim Y. Superciliary keyhole approach for small unruptured aneurysms in anterior cerebral circulation. Neurosurgery. 2011; 68(2 Suppl Operative):300–309. discussion 309. PMID: 21346651.

13. Ramos-Zúñiga R, Velázquez H, Barajas MA, López R, Sánchez E, Trejo S. Trans-supraorbital approach to supratentorial aneurysms. Neurosurgery. 2002; 51:125–130. discussion 130-131. PMID: 12182409.

14. Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005; 57(4 Suppl):242–255. discussion 242-255. PMID: 16234671.

15. Shin D, Park J. Unruptured supraclinoid internal carotid artery aneurysm surgery : superciliary keyhole approach versus pterional appro-ach. J Korean Neurosurg Soc. 2012; 52:306–311. PMID: 23133717.

16. van Lindert E, Perneczky A, Fries G, Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms : concept and technique. Surg Neurol. 1998; 49:481–489. discussion 489-490. PMID: 9586924.
Fig. 3
Six retraction sutures placed at the edges of the skin incision after supraorbital mini-craniotomy.

Fig. 4
Catheter angiograms of aneurysms favorable for a superciliary approach. A : PCoA aneurysm (arrow) inducing oculomotor nerve palsy. B : Inferior-directing ACoA aneurysm (arrow). C : MCA aneurysm (arrow) with a maximum diameter of 14 mm. Note the relatively narrow neck. PCoA : posterior communicating artery, ACoA : anterior communicating artery, MCA : middle carotid artery.

Fig. 5
Catheter angiograms of aneurysms unfavorable for a superciliary approach. A : Aneurysm (arrow) at the posterior wall of the ICA requiring application of a right-angled fenestrated clip. B : High-positioned ACoA aneurysm (arrow). ICA : internal carotid artery, ACoA : anterior communicating artery.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download