Abstract
Percutaneous endoscopic gastrostomy tube placement is often performed in patients with a ventriculoperitoneal shunt and it has been accepted as a safe procedure. The authors report a case of a 50-year-old male who developed acute exacerbation of the hydrocephalus immediately after the percutaneous endoscopic gastrostomy tube placement without any signs of shunt infection, which has not been reported until now. After revision of the intraperitoneal shunt catheter, the sizes of the intracranial ventricles were normalized.
Percutaneous endoscopic gastrostomy tube placement is a commonly used procedure to improve the nutritional state and rehabilitation capability of patients with central nervous system disorders2,4,5,7,8,10,18,19). It has a very low complication rate which, in most cases, is related to shunt infection occurring a few days or weeks after the procedure, and the procedure has been accepted as being safe6,11,15,16). There have been few reports of mechanical failure of the ventviculoperitoneal (VP) shunt after percutaneous endoscopic gastrostomy (PEG) tube insertion without shunt infection. The authors report a unique patient who had developed shunt malfunction immediately after PEG tube placement without any signs of shunt infection.
A 50-year-old male underwent a decompressive craniectomy and evacuation of intracranial hematoma because of his subdural hematoma and severe cerebral edema, caused by a motor vehicle accident. After a month, he developed hydrocephalus and required a VP shunt. His right Kocher's point was used for ventricular entry, and the peritoneal catheter was placed through a paramedian subcostal incision. He was transferred to the rehabilitation department and had been in a semicomatous state for 8 months.
A percutaneous endoscopic gastrostomy tube was placed six months after the VP shunt by a senior gastroenterologist who had more than 10 years of endoscopic experiences. The tube was introduced into the stomach through the epigastrium with a standard endoscopic pull-through technique. As usual, the patient received prophylactic antibiotics, and the procedure was performed with special attention and using a gentle technique so as not to interrupt the intraperitoneal shunt catheter.
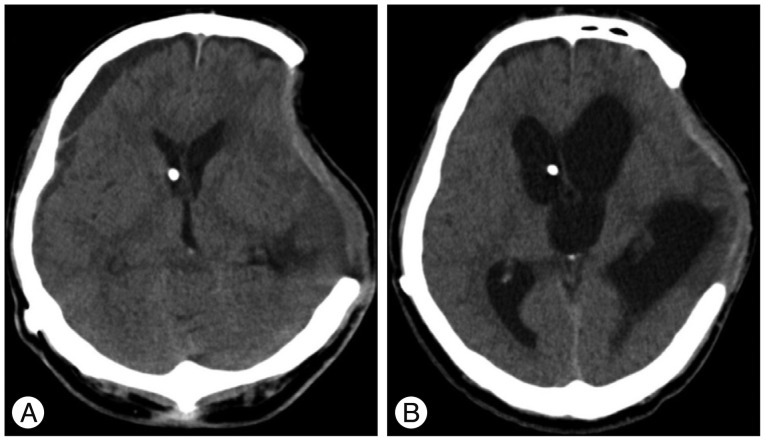
After a few hours, the scalp covering the surgical defect of his skull, which had been made by decompressive craniectomy, began to swell up. On the next day, it became worse and we took a brain CT scan which showed severely enlarged intracranial ventricles (Fig. 1).
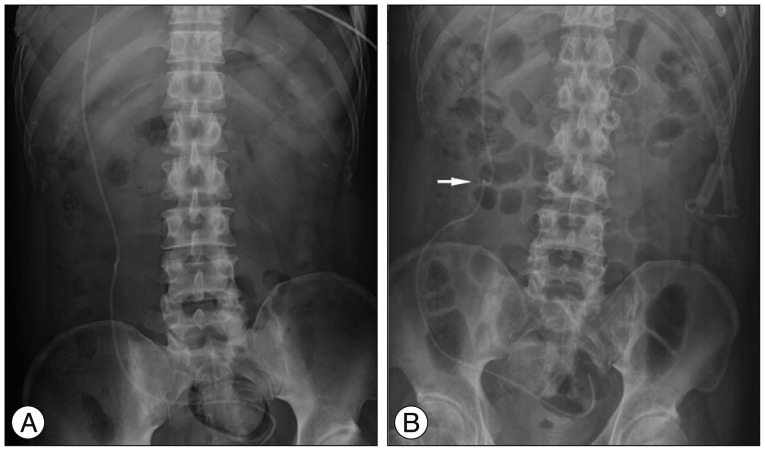
He had no fever or leukocytosis. Furthermore, no red blood cells or white blood cells were found in his cerebrospinal fluid. Skull X-rays were taken to confirm that the valve setting of the VP shunt had not been changed. The postprocedural abdominal film showed no gastrointestinal complications such as pneumoperitoneum or ileus, but kinking in the intraperitoneal shunt catheter was observed compared to the catheter being smooth before the procedure (Fig. 2). The patient underwent a distal shunt catheter revision. We made a small incision in the subcostal area and pulled out the intraperitoneal catheter. The externalized catheter was carefully observed and no obstruction or disconnection was found. After we confirmed the adequate CSF drainage of the catheter, we put it into his peritoneal cavity again. Postoperatively, the swollen scalp depressed down and the sizes of the intracranial ventricles normalized in the follow-up CT scan. After a few days of close observation, the patient was transferred to the rehabilitation department.
Percutaneous endoscopic gastrostomy tube insertion is performed in patients who have difficulty with swallowing or problems with mentality. Sometimes these patients already have had a VP shunt inserted. Because shunt malfunction can cause severe complications to the patient, it is important to know if the PEG tube placement is safe for patients with a VP shunt. There have been eight published papers supporting the safety of PEG tube placement in patients with a VP shunt1,6,11,12,14,15,16,17). It has thus been accepted as a safe procedure because it does not increase the infection rate of VP shunt. In the 126 cases reported in the eight articles, all the complicated cases were related to shunt infection and there were no cases with a simple mechanical failure of the VP shunt without shunt infection. Our case is quite different from those cases in terms of the occurrence time and the presence of infection.
To our knowledge, this is the first reported case of acute VP shunt malfunction after PEG tube placement without any signs of shunt infection. However, in the case of percutaneous fluoroscopic gastrostomy, which is technically similar to PEG tube placement, one case was reported in 2006. Jea et al.9) reported a 68-year-old woman who developed massive pneumocephalus caused by the inflation of gas into the peritoneum during fluoroscopic gastrostomy tube placement. The patient was treated nonoperatively. In 2002, Chan et al.3) reported a 70-year-old male whose peritoneal catheter extruded through a removed gastrostomy scar which happened two years after PEG tube removal. In addition, in 2013, Niewiadomski et al.13) reported a case of a 54-year-old female whose intraperitoneal catheter of VP shunt penetrated into her stomach 3 months following the PEG insertion. Those two cases were not related to shunt infection, but they were different from our case in terms of the occurrence time.
The authors think that the intraperitoneal shunt catheter was mobilized or forced to make a kink by the movement of the stomach, the small bowel or the omentum during the procedure and that it eventually caused obstruction of the shunt catheter and acute aggravation of the hydrocephalus. Though the patient was in a semicomatous state which made it difficult to detect the early neurological symptoms of hydrocephalus, he had a surgical skull defect, so we could find out the problem immediately and took steps to make the patient better.
Therefore, although PEG tube placement has been accepted as a safe procedure in patients with a VP shunt, clinicians should be aware of the possibility that acute shunt malfunction can occur, even if there is no infection. Furthermore, gastroenterologists who perform the procedure should be careful about the shunt catheter and need to use gentler techniques when the patient has a VP shunt. After the procedure, it is important to monitor not only the patient's laboratory data but also the neurological status and postprocedural abdominal X-rays as well.
References
1. Baird R, Salasidis R. Percutaneous gastrostomy in patients with a ventriculoperitoneal shunt : case series and review. Gastrointest Endosc. 2004; 59:570–574. PMID: 15044902.

2. Bannerman E, Pendlebury J, Phillips F, Ghosh S. A cross-sectional and longitudinal study of health-related quality of life after percutaneous gastrostomy. Eur J Gastroenterol Hepatol. 2000; 12:1101–1109. PMID: 11057455.

3. Chan Y, Datta NN, Chan KY, Rehman SU, Poon CY, Kwok JC. Extrusion of the peritoneal catheter of a VP shunt system through a gastrostomy wound. Surg Neurol. 2003; 60:68–69. discussion 70. PMID: 12865019.

4. Ciocon JO, Silverstone FA, Graver LM, Foley CJ. Tube feedings in elderly patients. Indications, benefits, and complications. Arch Intern Med. 1988; 148:429–433. PMID: 3124777.

5. D'Amelio LF, Hammond JS, Spain DA, Sutyak JP. Tracheostomy and percutaneous endoscopic gastrostomy in the management of the head-injured trauma patient. Am Surg. 1994; 60:180–185. PMID: 8116977.
6. Graham SM, Flowers JL, Scott TR, Lin F, Rigamonti D. Safety of percutaneous endoscopic gastrostomy in patients with a ventriculoperitoneal shunt. Neurosurgery. 1993; 32:932–934. PMID: 8327094.

7. Harbrecht BG, Moraca RJ, Saul M, Courcoulas AP. Percutaneous endoscopic gastrostomy reduces total hospital costs in head-injured patients. Am J Surg. 1998; 176:311–314. PMID: 9817245.

8. James A, Kapur K, Hawthorne AB. Long-term outcome of percutaneous endoscopic gastrostomy feeding in patients with dysphagic stroke. Age Ageing. 1998; 27:671–676. PMID: 10408659.

9. Jea A, Baskaya MK, Farhat H, Benglis D, Zauner A. Pneumocephalus in a patient with a ventriculoperitoneal shunt after percutaneous gastrojejunostomy catheter placement : case report. Surg Neurol. 2006; 65:87–89. discussion 89. PMID: 16378870.

10. Kaw M, Sekas G. Long-term follow-up of consequences of percutaneous endoscopic gastrostomy (PEG) tubes in nursing home patients. Dig Dis Sci. 1994; 39:738–743. PMID: 8149838.

11. Kim JS, Park YW, Kim HK, Cho YS, Kim SS, Youn NR, et al. Is percutaneous endoscopic gastrostomy tube placement safe in patients with ventriculoperitoneal shunts? World J Gastroenterol. 2009; 15:3148–3152. PMID: 19575495.

12. Nabika S, Oki S, Sumida M, Isobe N, Kanou Y, Watanabe Y. Analysis of risk factors for infection in coplacement of percutaneous endoscopic gastrostomy and ventriculoperitoneal shunt. Neurol Med Chir (Tokyo). 2006; 46:226–229. discussion 229-230. PMID: 16723814.

13. Niewiadomski O, Ashrafi A, Stella DL, Hebbard G. Education and Imaging. Gastrointestinal : gastric perforation from long-term ventriculo-peritoneal shunt after insertion of percutaneous endoscopic gastrostomy. J Gastroenterol Hepatol. 2013; 28:204. PMID: 23278156.

14. Roeder BE, Said A, Reichelderfer M, Gopal DV. Placement of gastrostomy tubes in patients with ventriculoperitoneal shunts does not result in increased incidence of shunt infection or decreased survival. Dig Dis Sci. 2007; 52:518–522. PMID: 17195119.

15. Sane SS, Towbin A, Bergey EA, Kaye RD, Fitz CR, Albright L, et al. Percutaneous gastrostomy tube placement in patients with ventriculoperitoneal shunts. Pediatr Radiol. 1998; 28:521–523. PMID: 9662573.

16. Schulman AS, Sawyer RG. The safety of percutaneous endoscopic gastrostomy tube placement in patients with existing ventriculoperitoneal shunts. JPEN J Parenter Enteral Nutr. 2005; 29:442–444. PMID: 16224038.

17. Taylor AL, Carroll TA, Jakubowski J, O'Reilly G. Percutaneous endoscopic gastrostomy in patients with ventriculoperitoneal shunts. Br J Surg. 2001; 88:724–727. PMID: 11350449.

18. Wanklyn P, Cox N, Belfield P. Outcome in patients who require a gastrostomy after stroke. Age Ageing. 1995; 24:510–514. PMID: 8588542.

19. Weaver JP, Odell P, Nelson C. Evaluation of the benefits of gastric tube feeding in an elderly population. Arch Fam Med. 1993; 2:953–956. PMID: 8111526.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download