INTRODUCTION
Corpectomy is a surgical procedure that removing whole or a part of the vertebral body. The common pathologies in which corpectomy is required are tumors, trauma, infection, and deformities
7,
10,
16,
17,
18). Vertebral body replacement following corpectomy is done using several kinds of different materials. Traditionally, autologous bone grafts such as tricortical iliac, fibula and costal bones had been used extensively
12). Allografts or synthetic implants are increasingly used to substitute autologous bone grafts in many cases
14,
17,
18). Non-fusion material like bone cement can be used in surgery of spine metastasis
9,
13).
Bagby
1) introduced stainless steel basket implants for interbody fusion, and this was followed by development of other prosthetic fusion implants, such as titanium mesh cage (TMC)
12). TMCs offer an advantageous reconstruction technique after corpectomy in the spine. Their hollow cylindrical structure is of a shape that can adequately recreate the size of adjacent vertebral bodies and can be filled with cancellous bone grafts, which promotes bone fusion
12,
17,
19). They offer resistance to axial compression, lateral flexion, and axial rotation, which provides good structural support
8,
19). More recently, expandable cages have been used for spinal reconstruction following corpectomy
19). However, the most common concerns associated with cage placement are excessive subsidence of cages, spinal kyphotic angular deformity, and recurrence of pain and/or neurological symptoms potentially requiring re-operation
5,
7). Moderate degree of spinal angular change and subsidence of mesh cage can happen during follow-up period
17). As kyphosis progresses, more stress is placed on pedicle screws, leading to breaking and dislodging of the screw
6,
17).
Follow-up radiological studies of vertebral body reconstruction using mesh cages after corpectomy were reported by several authors
5,
11,
12,
15,
16,
17), in all of which some degrees of subsidence or kyphotic angulation were reported irrespective of the kinds of fusion materials, even though bony fusions were successfully achieved. However, whether radiological change was related to the clinical symptoms was not clear in their articles. Moreover, in cases that non-fusion materials were used as graft after corpectomy, few reports are available to describe radiological change or its relationship to clinical symptoms.
In this study, we investigated angular changes of reconstructed spine in which TMCs filled with several kinds of graft material were used after corpectomy in thoracic and lumbar levels, settlement of TMCs, and their association with clinical symptoms. Whether factors like graft material, surgical approach, and fusion or not can affect the radiological stability was analyzed as well.
Go to :

MATERIALS AND METHODS
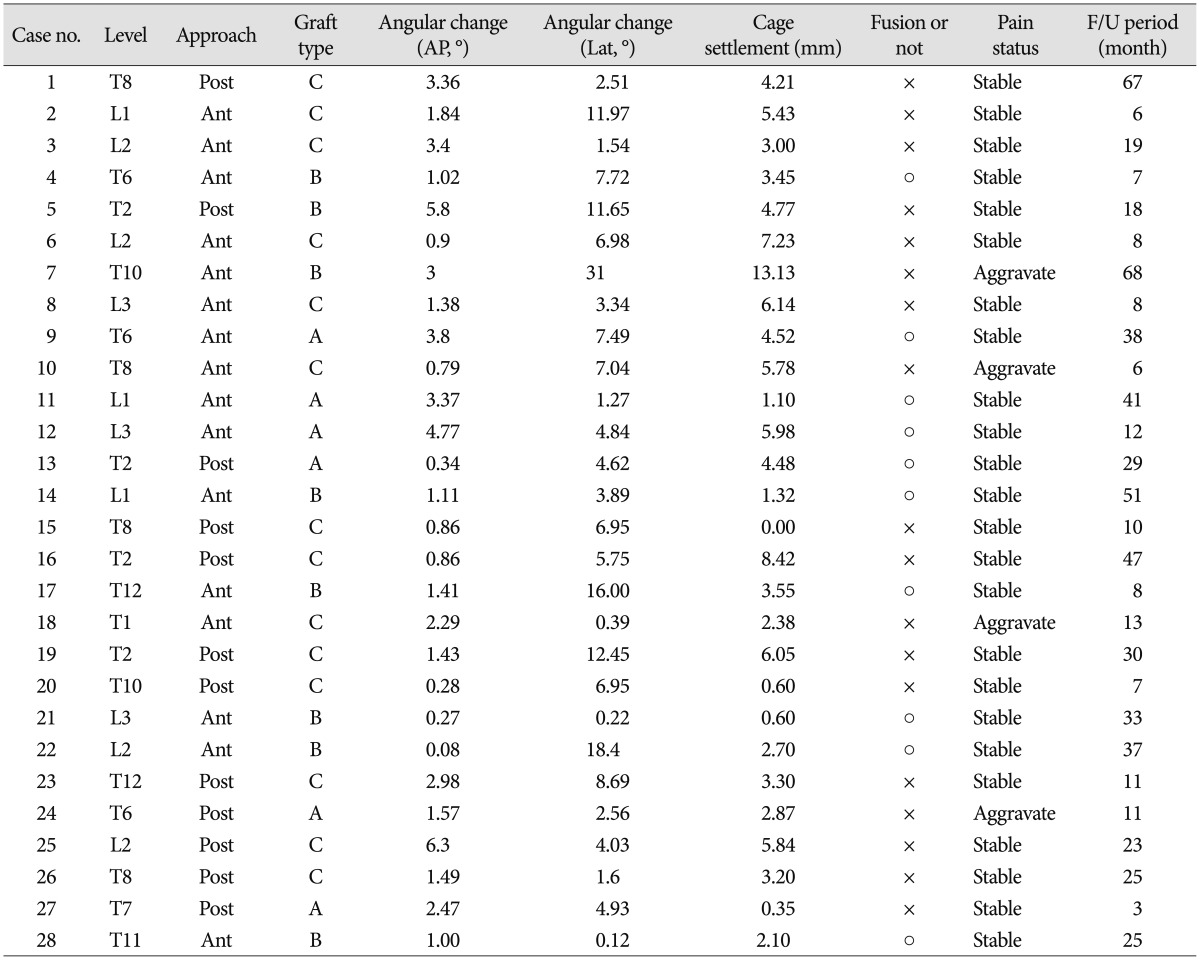
The subjects of this study were 28 patients who underwent corpectomy due to tumor, infection, and trauma from January 2005 to December 2011 (
Table 1). Their medical records and radiological data were retrospectively analyzed. Mean age was 56.2 years (18-77 years). Mean follow-up period was 23.6 months (6-68 months). In diagnosis, 23 patients of tumors, 2 patients of trauma, and 3 patients of infection were included. With regards to surgical approach, anterior approach was performed in 16 cases and posterior approach in 12 cases. In surgical strategy, anterior approach was chosen in cases that pathologic lesions were located in vertebral body only. It was adopted in 3 cases of infection, 2 cases of trauma, and 11 cases of tumor. Posterior approach was performed in cases that destructive lesions involved the pedicle and the posterior parts in addition to the vertebral body itself, all of which were tumor cases. In cases of infection and trauma, autologous bone graft was inserted into the TMC. However, three kinds of graft (autologous bone, allobone, and cement) were packed into the cage in each tumor case respectively. For anterior approach, supplementary fixation using anterior screws and rod/plate system was done to one level above and one level below the corpectomy site. Pedicle screw fixation was done to two levels above and two levels below the corpectomy site for posterior approach.
Table 1
Summary of 28 patients who underwent spinal reconstruction after corpectomy
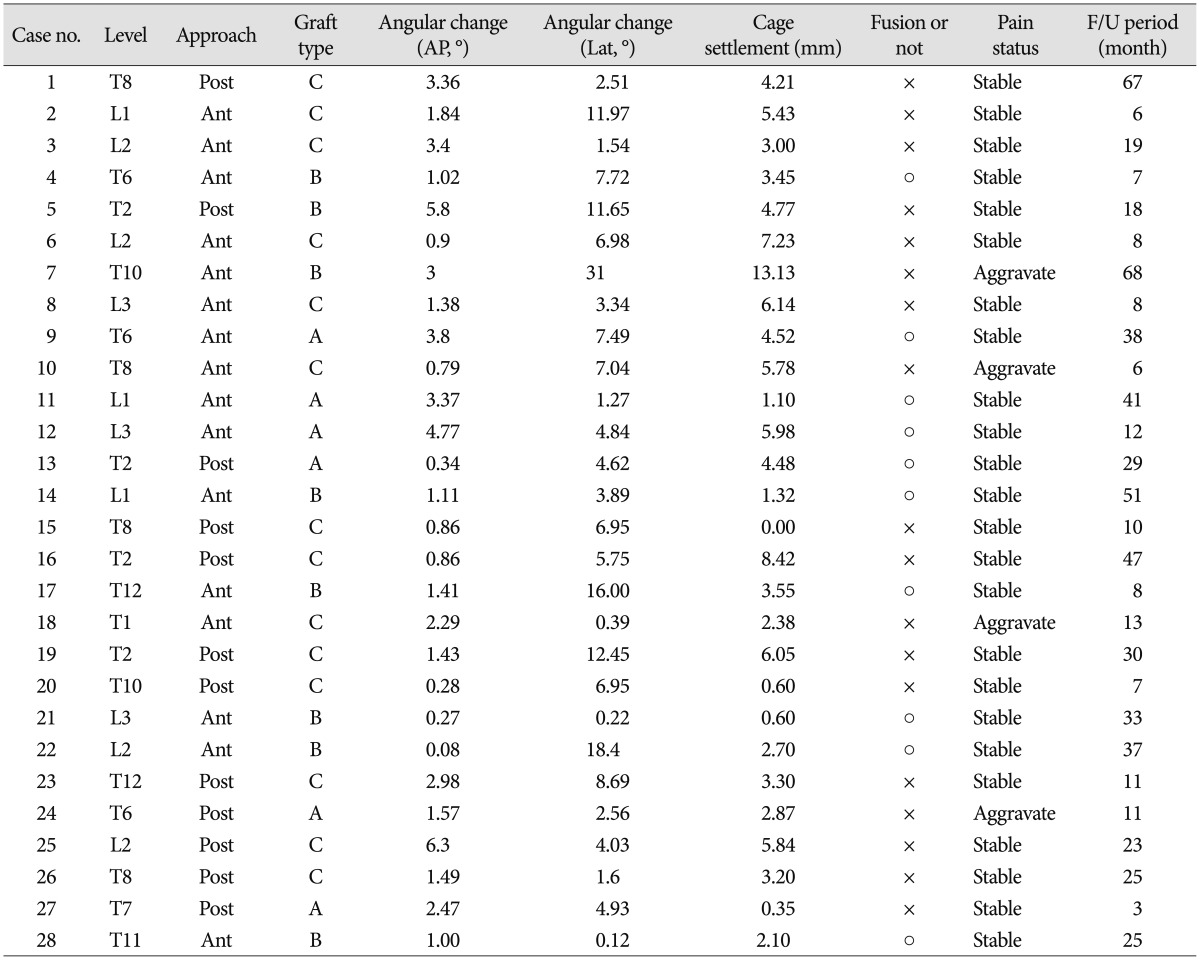

Eighteen lesions were located in thoracic spine and 10 in lumbar spine, respectively. Titanium Mesh Cage (TMC) was used in all patients and three different kinds of material were contained in it; autologous bone in 8, allograft bone in 6, and bone cement in 14. Each TMC trimmed to insert between the adjacent vertebral endplates in order to restore the sagittal alignment was stabilized by anterior or posterior instrumentation.
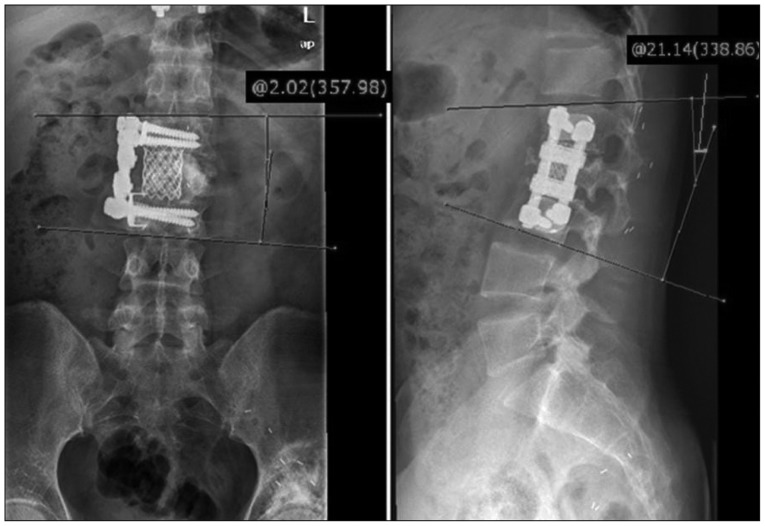
Various modality of images such as X-ray, computed tomography (CT), or magnetic resonance image (MRI) were taken at regular follow-up. Images taken at postoperative one month and last follow-up were also compared. Following factors were investigated for radiological evaluation : 1) Spinal angular changes in coronal and sagittal plane, 2) Fusion state of mesh cage with adjacent bone at last follow-up images, 3) TMC settlement; the change of vertebral body height in fused segment at last follow-up images compared to postoperative one month images. Spinal angular change was measured by Cobb's angle between the superior endplate of upper vertebrae (the one cranial to the corpectomy site) and the inferior endplate of the lower vertebrae (caudal to corpectomy site) (
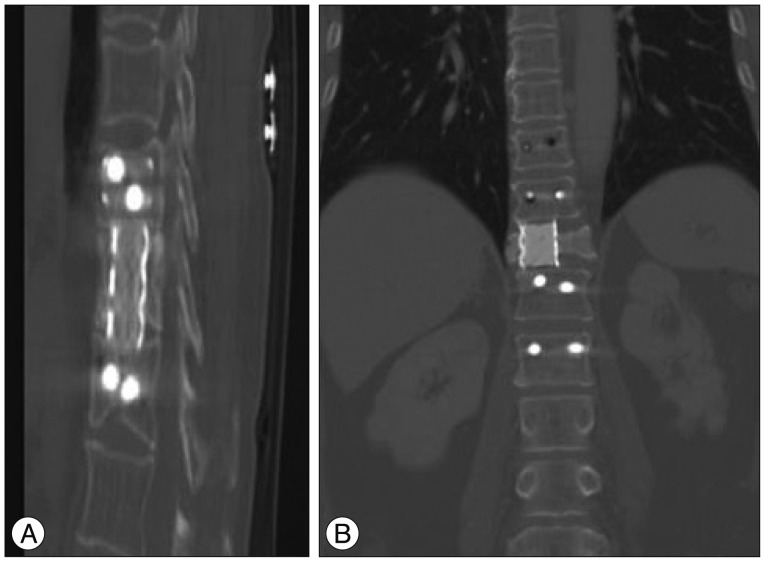
Fig. 1). Fusion status was assessed using plain radiograph or CTs, according to the grading system published by Bridwell et al.
3). In this system, grade 1 indicates definite fusion (fused with remodeling and trabeculae present); grade 2 indicates probable fusion (graft intact, not fully remodeled, no area of lucency); grade 3 indicates unlikely fusion (graft intact but lucency where it contacted the host bone surface); grade 4 indicates non-union (graft resorbed). We classified grade 1 and 2 as fusion group (
Fig. 2A), grade 3 and 4 as non-fusion group (
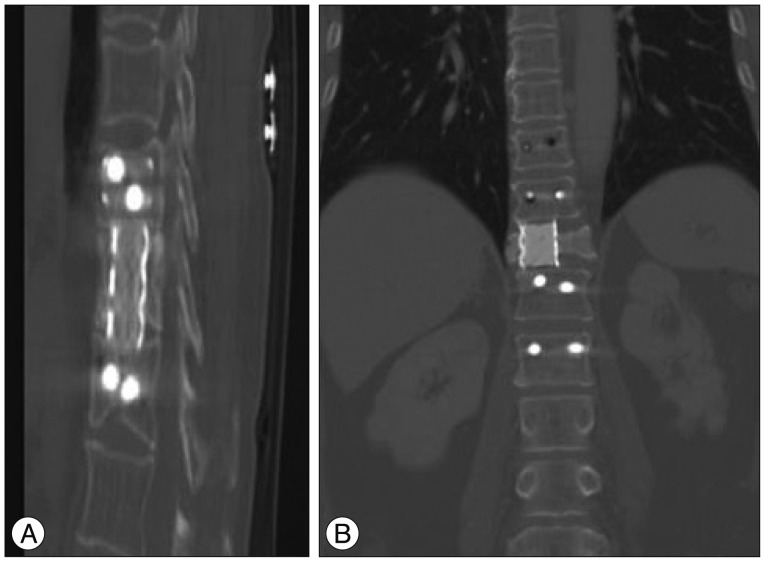
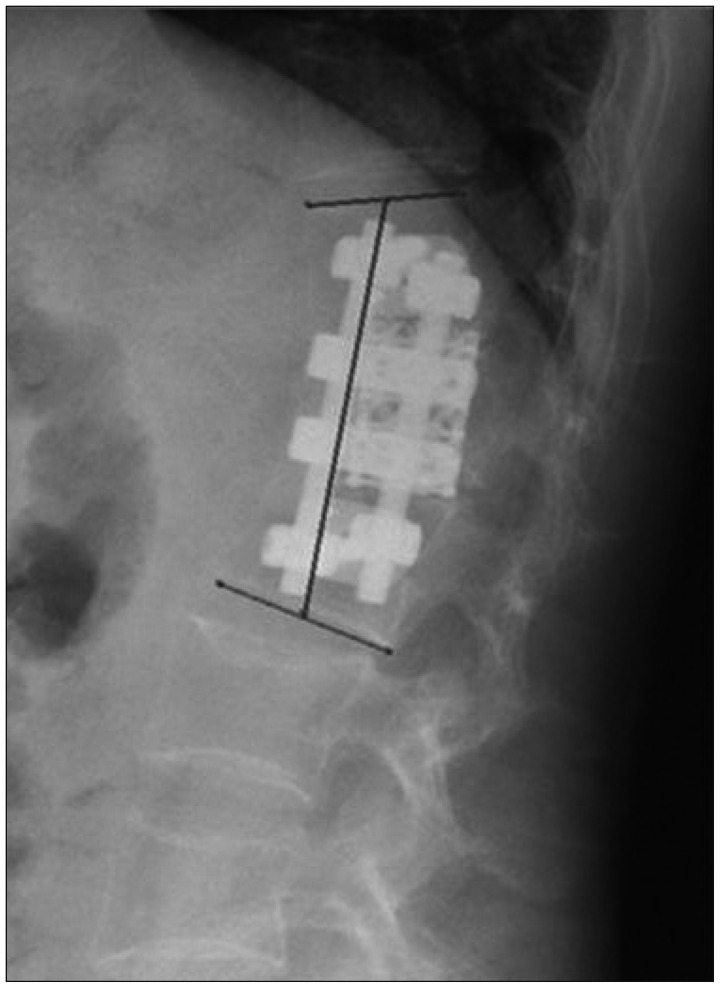
Fig. 2B). A few millimeters sinking, inclination or slippage of mesh cage was often found at the follow-up radiographs. The value of vertebral body height was checked by measuring the distance between the midpoint of superior endplate of the upper vertebrae (the one cranial to the corpectomy site) and the midpoint of inferior endplate of the lower vertebrae (caudal to corpectomy site) (
Fig. 3). Cage settlement was assessed by subtracting the values of vertebral body height measured at last follow-up from those measured at postoperative one month.
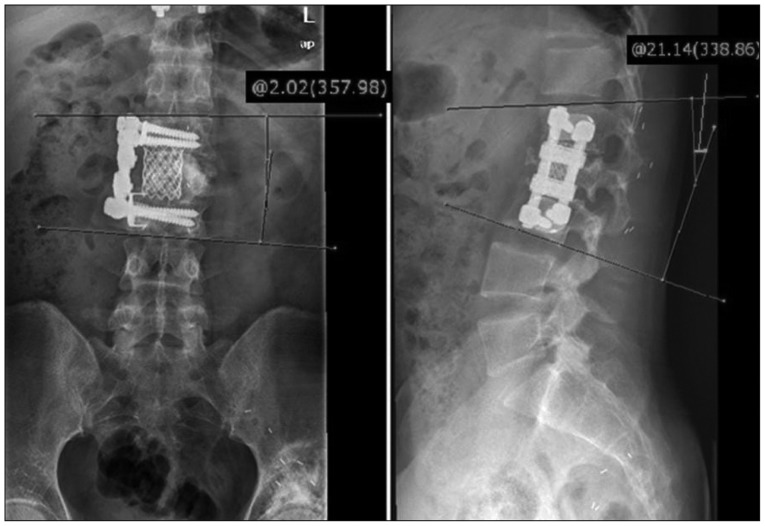 | Fig. 1Cobb's angle is measured between the superior end plate of upper vertebrae (cranial to the corpectomy site) and the inferior end plate of the lower vertebrae (caudal to corpectomy site) in coronal and sagittal plane. 
|
 | Fig. 2A : Example of definite fusion; grade 1 by Bridwell grading system. Bone remodeling and trabeculae are seen between cage and adjacent vertebral bodies. B : Example of non-fusion; grade 3 by Bridwell grading system. Radiolucency is observed between cage and lower endplate of upper vertebral body. 
|
 | Fig. 3Method of measuring vertebral height in fused segment. Vertebral body height is checked by measuring the distance between the midpoint of superior endplate of the upper vertebrae (the one cranial to the corpectomy site) and the midpoint of inferior endplate of the lower vertebrae (caudal to corpectomy site). 
|
We investigated the relationship of radiologic changes (angular change, settlement of cage) with pain status change. For assessment of patients' pain status, we evaluated pain score through chart reviews from clinical documents and sorted maintenance/improving group and aggravation group. When pain score at last follow-up was worse than that at postoperative one month, pain was considered as aggravation. Otherwise, the pain was classified as maintained/improving. The reason why the baseline was set at postoperative one month was that patients' condition was stable and free from wound pain at that time point. Whether radiological stability was influenced by several factors, such as the kind of graft material, surgical approach, and fusion was analyzed as well.
Statistical Package for the Social Sciences (SPSS) version 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The chi-square and Fisher's exact tests were used to compare means (e.g., angular change depending on surgical approach). Two-by-two crosstabs was adopted for categorical data analysis (e.g., the relationship between tumor progression and pain status). For correlation analysis of continuous variables, Pearson correlation coefficient was applied (e.g., the relationship between cage settlement and angular change). p-values of 0.05 (2-tailed) were considered significant.
Go to :

RESULTS
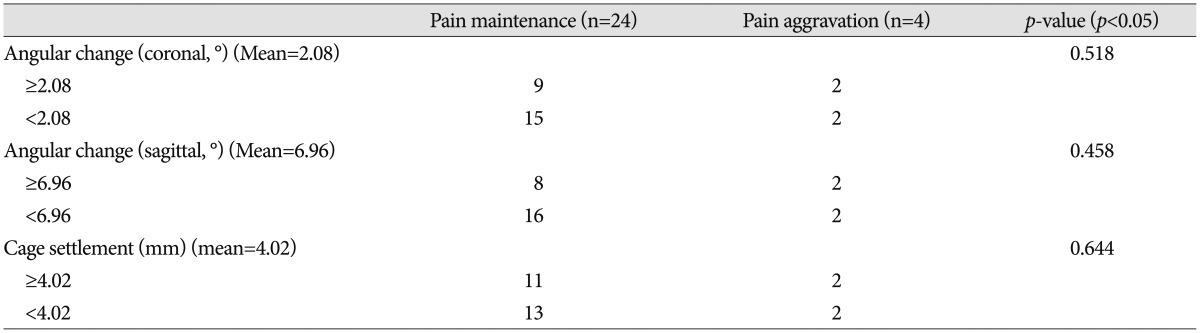
During follow-up period, mean spinal angular change of 2.08±1.65° and 6.96±2.08° was observed compared to postoperative one month in coronal and sagittal view, respectively (
Table 2). There were no cases of screw pull-out or screw breakage during the follow-up. In 4 cases, screw loosening was observed, which was supposed to influence the segmental angular change.
Table 2
The relationship between radiological stability and pain status
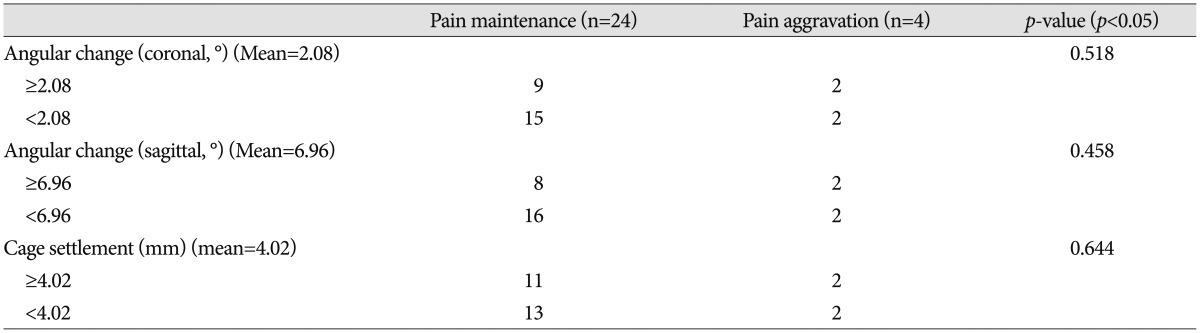

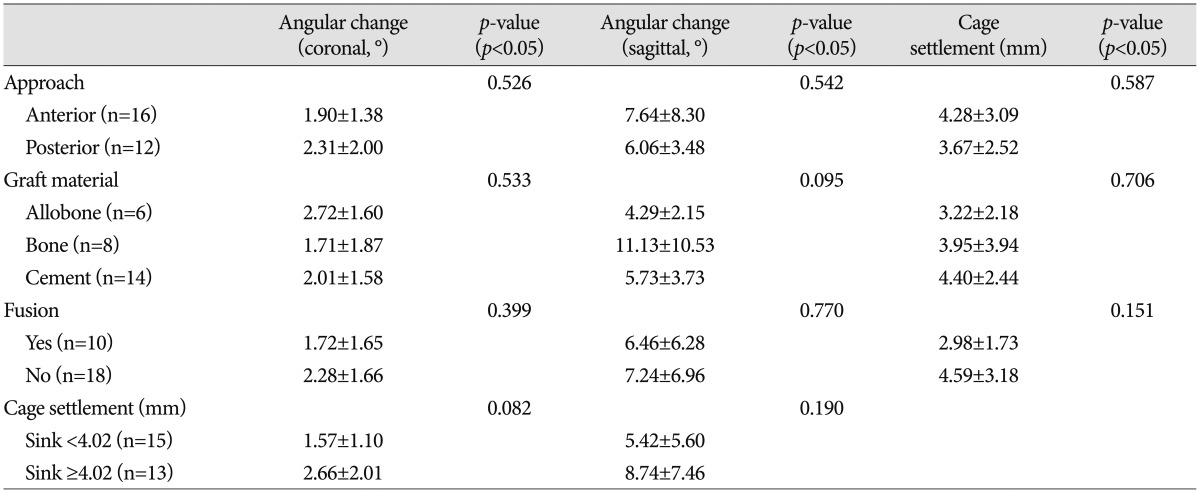
The spinal angular change was not influenced by such factors as surgical approach, bony fusion state, type of graft material (
Table 3). With regard to bone fusion, coronal angular change was 1.72±1.65° in fusion group (n=10) and 2.28±1.66° in non-fusion group (n=18) (
p=0.399) and sagittal angular change was 6.46±6.28° in fusion group and 7.30±7.67° in non-fusion group (
p=0.770).
Table 3
The factors influencing radiological stability
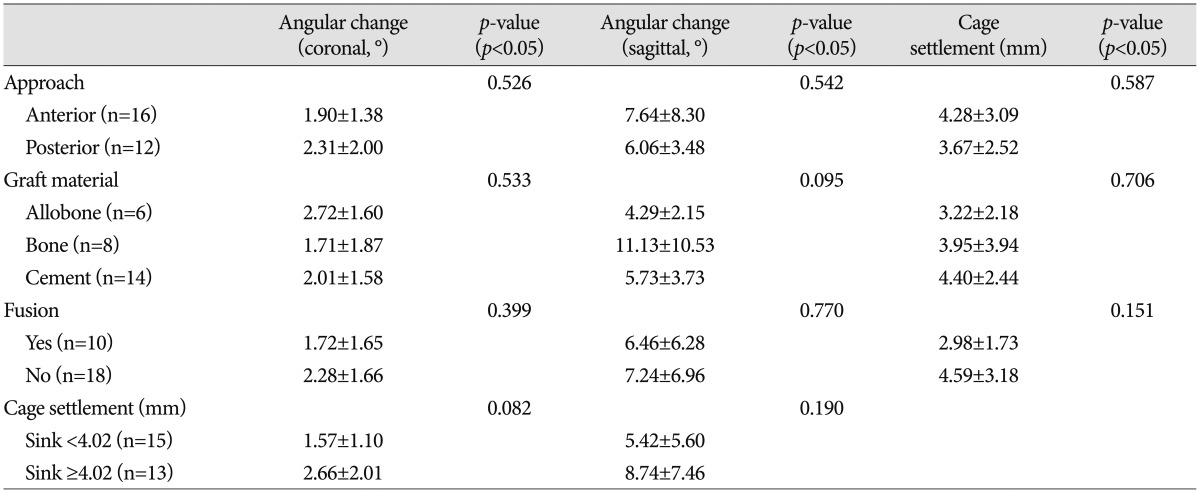

During the follow-up, TMC settlement was observed in 27 cases. A mean of cage settlement was 4.02±2.83 mm. In non-fusion group (n=18) cage settlement was 4.59±3.18 mm and in bony fusion group (n=10) it was 2.98±1.73 mm, which was not statistically significant (
p=0.151) (
Table 3). When spinal angular changes in coronal plane were compared between cage settlement <4.02 mm group and cage settlement ≥4.02 mm group, they were 1.57±1.10° and 2.66±2.01° (
p=0.082). In the evaluation of sagittal angular change, they were 5.42±5.60° and 8.74±7.46° (
p=0.190). Although spinal angular changes tend to increase according to the degree of cage settlement in both coronal and sagittal plane, they were not statistically significant (
Table 3). Data on bone mineral density (BMD) were available in 13 patients. A mean value of T score was -2.59. When the mean values of cage settlement were compared between group with T score ≥-2.5 (n=7) and group with T score <-2.5 (n=6), they were 2.94±1.47 mm and 3.05±2.04 mm, which was statistically not different (
p=0.910).
Pain aggravation was observed in 4 patients (3 cases of tumor, 1 case of infection). When pain status was analyzed depending on the spinal angular change, the correlation was not significant (
Table 2). In patients with sagittal angle change <6.96° (n=18), pain aggravation was noted in 2 patients and pain maintenance in 16. In patients with sagittal angle change ≥6.96° (n=10), pain was aggravated in 2 patients and stable in 8 (
p=0.458) (
Table 2). With regard to coronal plane angle evaluation, 2 patients suffered from aggravated pain out of 11 patients with angle change ≥2.08°. In 17 patients with angle change <2.08°, 2 patients showed pain aggravation (
p=0.518). The settlement of TMC was not correlated with patients' pain status, either. In patients whose TMC sinking was more than 4.02 mm (n=13), pain was aggravated in 2 patients and stable in 11. In patients whose TMC sinking depth was less than 4.02 mm (n=15), 2 patients suffered from aggravated pain and 13 were in stable state. This findings show no significant difference in pain score between both groups (
p=0.644) (
Table 2).
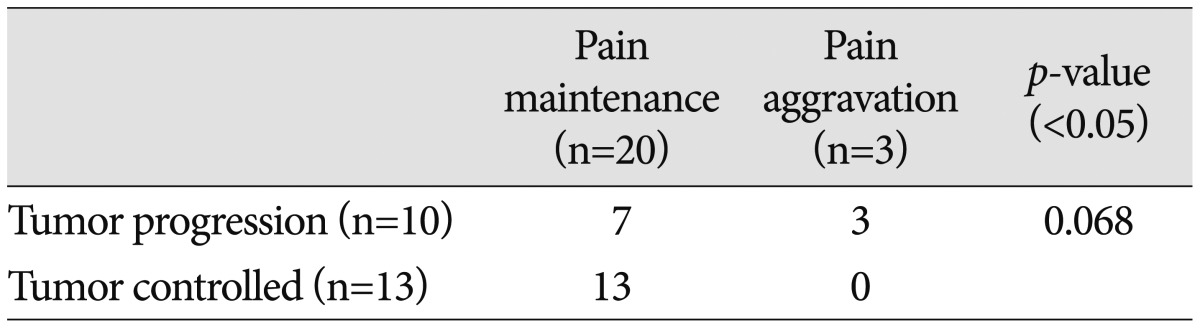
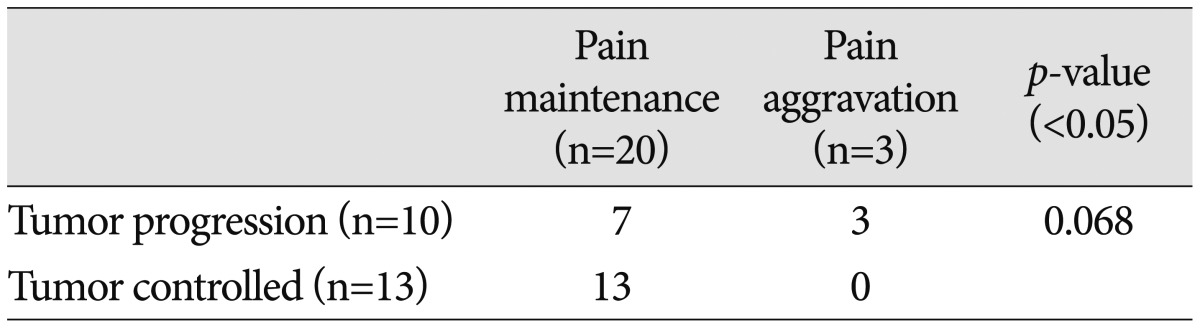
Out of 23 tumor cases, 3 patients of pain aggravation were noted. Regarding tumor state, 13 patients were in tumor-controlled state and 10 patients showed tumor progression due to local recurrence. The patients who suffered from pain aggravation with tumors were in the state of tumor progression. However, statistical significance was not found between tumor progression and pain aggravation (
p=0.068) (
Table 4).
Table 4
The relationship between tumor progression and pain status

Go to :

DISCUSSION
The primary role of TMC is to provide structural support to the anterior spinal column
19). An ideal anterior spinal column reconstruction should provide a mechanically stable construct between vertebral endplates that can maintain spinal alignment while facilitating bony fusion.
With regards to mechanical stability, TMCs have been known to give stable construct in follow-up radiological studies. Zahra et al.
19) reported the occurrence of 2° of mean kyphosis at postoperative 2 years in the thoracolumbar spine fracture patients in whom anterior reconstruction with cylindrical mesh cage was performed after vertebral body resection. Karaeminogullari et al.
12) reported that a mean correction loss of 4° on minimum 3-year follow-up was noted in 34 patients who underwent anterior reconstruction after corpectomy due to fracture, infection and deformity. In their study, TMCs filled with autologous bone graft were superior to strut autografts and strut allografts in terms of mechanical stability when used for interbody fusion
12). Robertson et al.
17) reported 3° progression at 1-year follow-up after anterior reconstruction with plate in 31 thoracolumbar corpectomy cases. Eck et al.
7) reported 1° progression of kyphosis on follow-up of 33 months in patients who had anterior reconstruction with TMC in deformity correction surgery. In our study, mean progression of 2° in coronal plane and 7° in sagittal plane were detected respectively (
Table 2).
Regarding study population, only a few articles dealt with each single disease entity such as trauma or deformity
7,
19). However, in most articles, the disease of the study population was mixed and surgical approaches of anterior only, posterior only, or combination were dependent upon the diseases and were complexly used
2,
6,
8,
12,
17). Our series also included cases with different disease and with complex surgical approaches. Because the purpose of our study was to investigate the relationship between radiological change and clinical symptoms in reconstructed spine, the heterogeneity of the disease and surgical approach was unlikely to be significant.
The subsidence of TMC was a common phenomenon after anterior cervical corpectomy and fusion. Chen et al.
5) described that subsidence of mesh cage was diagnosed in 79.7% of 300 patients in whom one level or two-level copectomy was performed. In their reports, severe subsidence more than 3 mm was related to clinical symptom development. In another report, structural bone graft without plating in cervical corpectomy cases showed average settling of 6.7 mm, which did not correlate with pain outcomes
11). In thoracic and lumbar spine, settlement of cage was seen to be less than 3 mm in patients in whom successful bone fusion was achieved
2,
12,
19). Though 4.02 mm of TMC settlement occurred during the follow-up, our data revealed that the severity of cage settlement was not related to clinical symptoms.
In regarding fusion, high rate of fusion over than 95% was reported using TMC with autologous bone grafts
19). This figure was better than the results with structural allograft. Bridwell et al.,
3) and Buttermann et al,
4) reported a fusion rate of 92%, and 91.4% respectively in reconstruction with structural allograft. In Bhat et al.,
2) study, 13 patients who underwent anterior reconstruction with TMC-autologous bone graft after thoracic and lumbar corpectomy showed 100% bony fusion
7). Rapid and strong fusion requires good surface contact and stability in the fusion region
12). TMCs offer the option of autogenous bone's osteoconductivity and osteoinductivity without structural bulk graft
17). TMCs' transformability provides ideal shape to be positioned between adjacent vertebral bodies
12).
When pain status was evaluated in relating to tumor progression in 23 tumor patients, pain aggravation was observed in 3 out of 10 patients with tumor progression. However, no patients showed pain aggravation in tumor controlled group (
p=0.068) (
Table 4). Although it was statistically not significant, it showed trend that pain status tended to aggravate depending on tumor progression. If the number of cases is increased, statistical significance might be found between pain status and tumor progression.
In surgery for spinal metastasis, non-fusion materials such as bone cement, metal and synthetic materials are used instead of bone grafts. In contrast to surgery for trauma and degenerative disease, surgical goal in metastatic disease is not fusion, but tumor resection, stabilization, and pain control. This is the reason why spinal reconstruction with non-fusion materials is increasingly used in place of bone grafts
16). Bone cements such as polymethylmethacrylate (PMMA) are used either in combination with TMCs or alone
9,
13). Liu et al.
13) reported that six patients of cervical spine metastasis were treated with PMMA-filled cage via anterior approach. During follow-up period of 1-19 months (mean, 6.8 months) graft subsidence, dislodgement, or construct failure were not noted. Rajpal et al.
16) compared different interbody reconstruction implants after corpectomy in 37 patients of metastatic spine tumors. Twenty-seven, 5, and 5 patients underwent reconstruction with metal implants, bone grafts, and PMMA, respectively. They evaluated the three kinds of implants in view of the need for any revision surgeries or complications after surgery, not by radiological stability. The rate of revision surgery was highest in the bone graft group (40%) compared with none in the PMMA and only 3.7% in the metal groups. A variety of metal and synthetic materials now exist, including metal alloys, carbon fibers, polyetheretherketone (PEEK) and ceramics
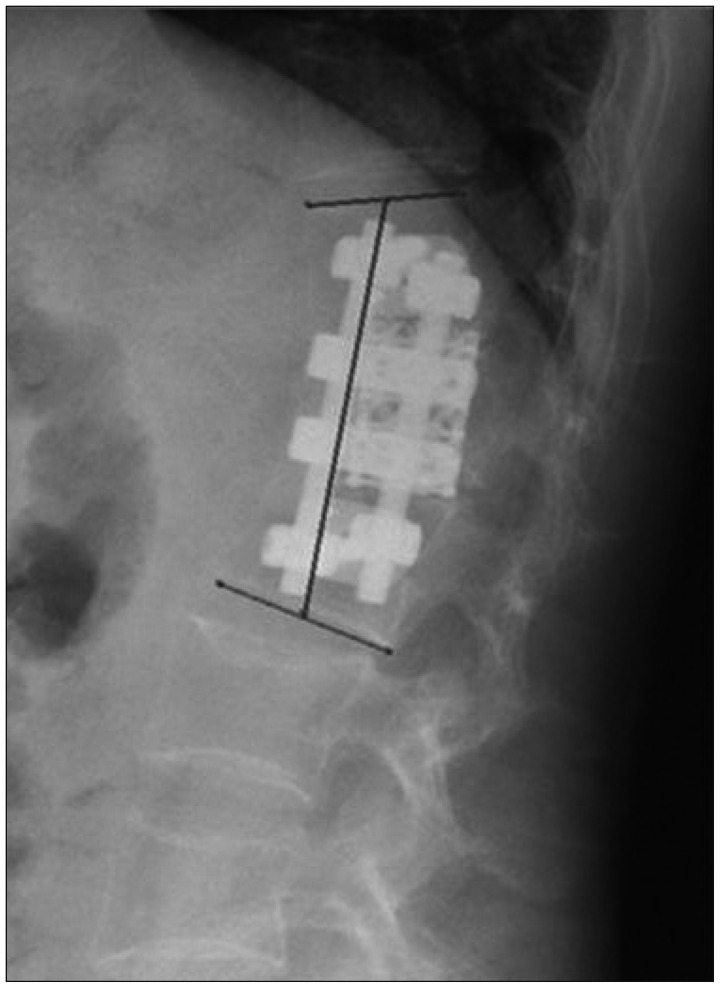
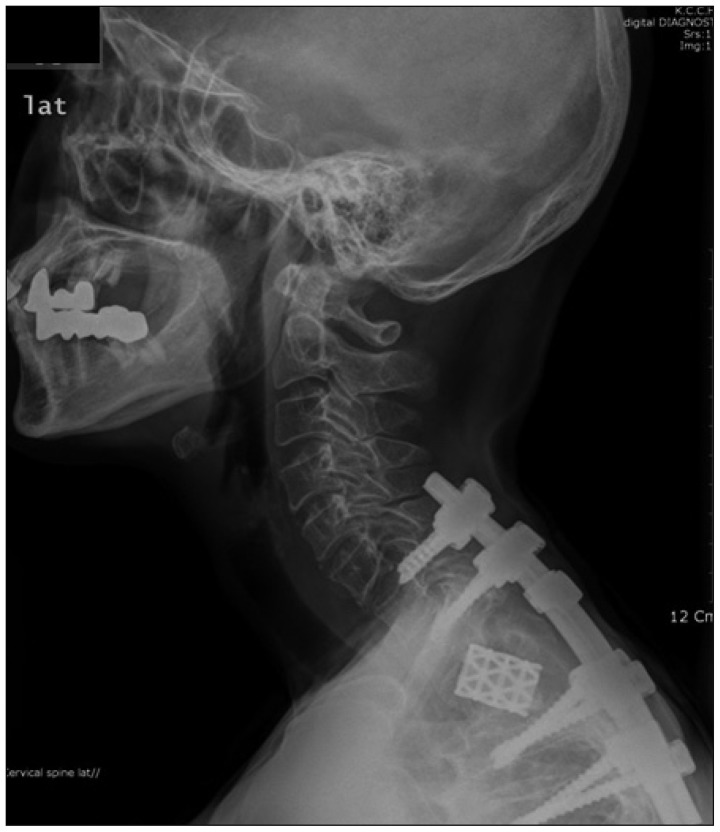
16). However, no study was performed with regards to the longevity of various kinds of non-fusion grafts in spinal reconstruction after metastatic vertebral body removal. In our series, both spinal angular change and cage settlement were not different between fusion group and non-fusion group. Radiological changes were not related to the pain aggravation, either. In case 1, TMC filled with bone cement was inserted after T8 corpectomy through posterior approach. On 67 months follow-up, angular change was 3.4° in coronal plane and 2.5° in sagittal plane. Cage settlement was 4.2 mm. On last follow-up, pain was successfully controlled. Even though bone fusion was not achieved, spinal construct could be maintained for a long time. Our data show that TMC filled with non-fusion material can play a role as durable anterior column support in long term survivor who underwent surgery for spinal metastasis. In case 16, T2 corpectomy was performed through posterior approach. After corpectomy, bone cement-filled TMC was inserted with posterior pedicle screw fixation. Follow-up image showed 8.4 mm settlement and migration of TMC cage, but no aggravation of pain was observed on 47 months follow-up (
Fig. 4).
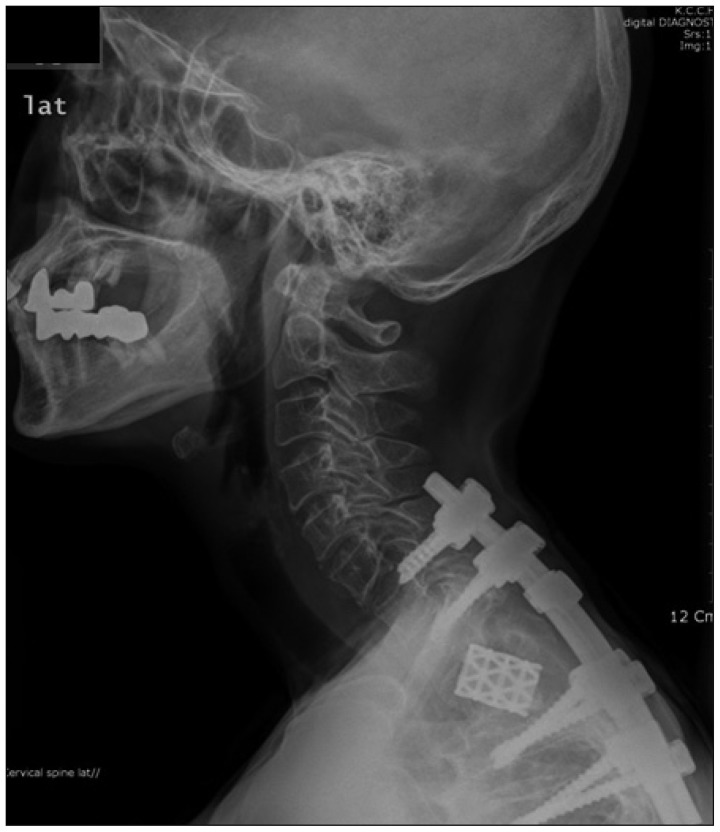 | Fig. 4A case of cage migration. After T2 corpectomy, reconstruction is done with bone cement-filled TMC and tranpedicular screw fixation. Follow-up image showed cage migration, but no aggravation of pain is observed on 47 months follow-up (case 16). TMC : titanium mesh cage. 
|
Although our data provide useful information on spinal tumor surgery, there are a few weak points in our study. First, extent of vertebral body resection, which might be a factor to influence postoperative spinal instability, was different in each case. When partial corpectomy was performed in anterior approach at thoracic and lumbar level, anterior cortex and anterior longitudinal ligament was left intact. On the contrary, in complete removal of vertebral body, they were removed. When transpedicular corpectomy was done via posterior approach, pedicle was removed unilaterally or bilaterally. If unilateral pedicle removal was done, contralateral facet joint and pedicle were saved. However, when bilateral pedicles were involved with tumor mass, bilateral facet removal was done. In those cases, spinal instability may be severer. In this study, extent of vertebral body resection or facet resection was not considered. Second, follow-up period was various. It ranged from 6 months to 68 months. Eleven cases whose follow-up period was shorter than one year were included. If follow-up period is extended, different outcome might be presented.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download