Abstract
A 66-year-old man presented with typical trigeminal neuralgia (TN). Magnetic resonance angiography (MRA) revealed a primitive trigeminal artery (PTA) that came into contact with the trigeminal nerve. Based on MRA, we performed microvascular decompression (MVD). In the operational field, we confirmed the PTA location and performed MVD successfully. Postoperatively, the patient's pain subsided without any complications.
Trigeminal neuralgia (TN), a neuropathic pain syndrome, is defined by the International Association for the Study of Pain as "a sudden and usually unilateral severe brief stabbing recurrent pain in the distribution of one or more branches of the fifth cranial nerve"3). Vascular compression and resultant injury to the trigeminal nerve at its root entry zone (REZ) are the proposed mechanisms of TN5). The vessel that most often causes TN is the superior cerebellar artery (SCA), other known offending vessels include the anterior inferior cerebellar artery (AICA) and the vertebrobasilar trunk and vein. Case reports have also rarely described TN caused by a primitive trigeminal artery (PTA)2,4,8,9). We introduce a case of TN caused by PTA that was successfully treated with surgery.
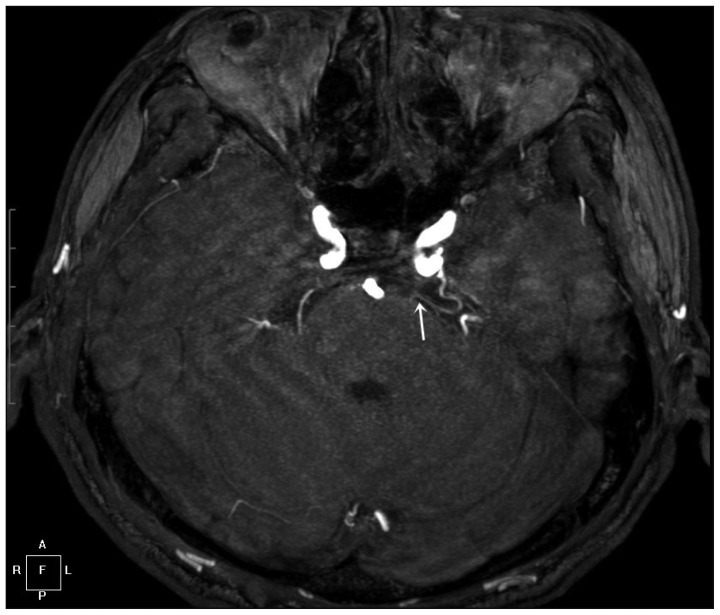
A 66-year-old male presented to our hospital with a 9-year history of typical left trigeminal neuralgia symptoms that gradually became refractory to medical treatment. Magnetic resonance angiography (MRA) revealed a PTA arising from the postero-lateral aspect of the posterior genu of the cavernous segment of the left internal carotid artery. The PTA coursed postero-laterally and inferiorly around the dorsum sellae. In its lateral course, it came into contact with the left trigeminal nerve (Fig. 1). A three-dimensional time-of-flight MRA showed a PTA coursing around the trigeminal nerve (Fig. 2).
The patient underwent microvascular decompression via the left retrosigmoid approach. After 25×45-mm craniectomy, the dura was opened in a Y shape. Then, with adequate drainage of cerebrospinal fluid and gentle retraction of the cerebellum, we observed the trigeminal nerve and vessel, which were compressed into the caudomedial part of the nerve. In the operational field, we confirmed that the vessel came into contact with the trigeminal nerve with a loop in the posterolateral direction (Fig. 3). The field was consistent with the MRA imaging. We transposed the PTA laterally away from the nerve, and decompressed the nerve by interposing Teflon between the vessel and the nerve. The operation was completed without any complications. Postoperatively, the patient's pain disappeared completely without sequelae. After receiving medication for 1 year, the patient remained pain-free without medication thereafter.
A persistent PTA is an uncommon vessel with a reported incidence of 0.03-2.2% in the literature10). Cases of PTA-induced TN are even rarer. During embryonic intracranial vascular development, four main temporal anastomoses arise between the carotid and vertebral-basilar systems10). The trigeminal artery is the largest of the fetal carotid-basilar anastomotic arteries, and it persists for the longest embryonic period6,7). The artery usually involutes after the development of the posterior communicating artery10). The exact causes of the persistence of this primitive vessel into adulthood are not completely clear1). The PTA of adulthood courses through the cavernous sinus and emanates from the posterior wall of the cavernous sinus, following either a para- or intrasellar course1,6,7). The PTA reaches the posterior cranial fossa in two ways : by 1) penetrating the sella turcica, running in its own groove, and perforating the dura mater near the clivus in about half of cases; or by 2) running extradurally after leaving the cavernous sinus and traveling between the sensory trigeminal root and the lateral side of the sella in a groove of the posterior clinoid process in the other half. In our case, we visualized the PTA coursing postero-laterally and inferiorly around the dorsum sellae. Furthermore, we were able to identify the cause of the patient's TN by the PTA's proximity to the trigeminal nerve.
Several reported cases of PTA-induced TN utilized cerebral angiography for verification of the PTA4,8,9). In our case, we intended to implement cerebral angiography for PTA identification; however, we used MRA only. MRA can fully confirm the vessel that induces TN, so patients who need surgical treatment may undergo an operation without being exposed to the risks of cerebral angiography. Cerebral angiography has the advantage of accurately displaying the vessels, but it cannot show the relationship of the vessels to the nerve structures. Preoperative visualization of the specific vessel causing TN is important in patients who require surgery. When the patient's condition is unable to tolerate cerebral angiography or when the patient is refusing further invasive evaluation, preoperative MRA or computed tomography angiography (CTA) may confirm the vessel. In addition, proper visualization may reveal the orientation of the vessel around the nerve, aiding in surgical planning. In the present case, we used MRA to verify the causal vessel. Furthermore, we evaluated the vessel and its surrounding structures using CTA and evaluated the relationship between dural structures and the nerve on MRA. The combination of MRA and CTA was useful for understanding the anatomy of the surgical field. Preoperative imaging led to a straightforward operation, even without cerebral angiography.
As shown in our case, the usefulness of MRA and CTA has been confirmed by the similarity of MRA images and operative findings. In this way, we were able to properly plan and execute surgical treatment while avoiding invasive cerebral angiography.
References
1. Azab W, Delashaw J, Mohammed M. Persistent primitive trigeminal artery : a review. Turk Neurosurg. 2012; 22:399–406. PMID: 22843453.
2. Fukuda M, Kameyama S, Takahashi H, Tanaka R. Trigeminal neuralgia caused by the vertebral artery associated with primitive trigeminal artery and agenesis of the internal carotid artery. Neurol Med Chir (Tokyo). 1998; 38:367–370. PMID: 9689822.

3. Garg RK, Malhotra HS, Verma R. Trigeminal neuralgia. J Indian Med Assoc. 2011; 109:631–636. PMID: 22480095.
4. Lee SH, Koh JS, Lee CY. Trigeminal neuralgia caused by an anomalous posterior inferior cerebellar artery from the primitive trigeminal artery : case report. Cerebellum. 2011; 10:199–203. PMID: 21279490.

5. Liu JK, Apfelbaum RI. Treatment of trigeminal neuralgia. Neurosurg Clin N Am. 2004; 15:319–334. PMID: 15246340.

6. O'uchi E, O'uchi T. Persistent primitive trigeminal arteries (PTA) and its variant (PTAV) : analysis of 103 cases detected in 16,415 cases of MRA over 3 years. Neuroradiology. 2010; 52:1111–1119. PMID: 20309534.
7. Schmid AH. Presistent trigeminal artery. An autopsy report. Neuroradiology. 1974; 7:173–175. PMID: 4842039.
8. Tamura Y, Shimano H, Kuroiwa T, Miki Y. Trigeminal neuralgia associated with a primitive trigeminal artery variant : case report. Neurosurgery. 2003; 52:1217–1219. discussion 1219-1220. PMID: 12699569.

9. Tokimura H, Atsuchi M, Kawasaki T, Sato E, Todoroki K, Asakura T, et al. [Trigeminal neuralgia associated with primitive trigeminal artery : report of two cases]. No Shinkei Geka. 1990; 18:209–213. PMID: 2336149.
10. Vasović L, Jovanović I, Ugrenović S, Vlajković S, Jovanović P, Stojanović V. Trigeminal artery : a review of normal and pathological features. Childs Nerv Syst. 2012; 28:33–46. PMID: 22071960.

Fig. 1
A : Magnetic resonance image showing a primitive trigeminal artery (white arrowhead) in contact with the left trigeminal nerve (black arrow). B : Magnetic resonance angiography revealing a primitive trigeminal artery (white arrow) originating from the left internal carotid artery.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download