Abstract
Objective
To report long-term clinical and radiological outcomes of minimally invasive posterior cervical foraminotomy (MI-PCF) performed in patients with unilateral single-level cervical radiculopathy.
Methods
Of forty-six patients who underwent MI-PCF for unilateral single-level radiculopathy between 2005 and 2013, 33 patients were included in the study, with a mean follow-up of 32.7 months. Patients were regularly followed for clinical and radiological assessment. Clinical outcome was measured by visual analogue scale (VAS) for the neck/shoulder and arm, and the neck disability index (NDI). Radiological outcome was measured by focal/global angulation and disc height index (DHI). Outcomes after MI-PCF were evaluated as changes of clinical and radiological parameters from the baseline. Mixed effect model with random patients' effect was used to test for differences in the clinical and radiological parameters repeat measures.
Results
There were no complications and all patients had an uneventful recovery during the early postoperative period. VAS scores for neck/shoulder and arm improved significantly in the early postoperative period (3 months) and were maintained with time (p<0.001). NDI improved significantly post-operatively and tended to decrease gradually during the follow-up period (p<0.001). There were no statistically significant changes in focal and global angulation at follow-up. Percent DHIs of the upper adjacent or operated disc were maintained without significant changes with time. During the follow-up, same site recurrence was not noted and adjacent segment disease requiring additional surgery occurred in two patients (6%) on the contra-lateral side.
The most prevalent surgical approaches for the treatment of patients with cervical radiculopathy refractory to conservative management are anterior cervical discectomy and fusion (ACDF) and posterior cervical foraminotomy (PCF). Although most surgeons may be more familiar with ACDF using anterior approaches for the surgical treatment of cervical radiculopathy, PCF has some advantages over ACDF. It avoids the possible approach-related complications of ACDF, which include post-operative swallowing difficulty and hoarseness. PCF results in preservation of the intervertebral disc and the motion segment, lessening the need for fusion, thus potentially avoiding graft-related complications and reducing adjacent segment disease5,14,16,22).
Despite being considered as the most rewarding procedure in neurosurgery20), traditional open PCF has major drawbacks to disrupt deep extensor with extensive subperiosteal dissection of the muscular and tendinous insertion, while exposing the lamina and lateral mass. This may cause persistent axial pain, paraspinal muscle spasm, and malalignment of the spine2,5,12,14). Recently, minimally invasive approaches for PCF have been introduced to minimize the problems related to this extensive dissection1,6). The minimally invasive (MI)-PCF technique typically involves a muscle-splitting approach via a small paramedian incision with placement of a tubular retractor system using a microscope or an endoscope. This technique resulted in a lower operative blood loss, shorter surgical time and hospitalization, and lower infection rate than the open technique4). In spite of these promising initial results, only a few reports have addressed long-term clinical results of minimally invasive approaches for PCF.
The purpose of this study was to evaluate the long-term outcomes of MI-PCF in both clinical and radiological aspects, following surgery in patients with unilateral single-level cervical radiculopathy.
Between 2005 and 2013, MI-PCF was performed in 46 patients with unilateral single-level cervical radiculopathy. The patients underwent relevant clinical and radiological investigation initially, and adequate follow-up was possible in 33 patients. Data was analyzed retrospectively via electronic medical record and image software review. The questionnaires and radiologic images were prospectively collected at the scheduled times. Surgical indication included cervical radiculopathy due to lateral herniated disc or stenosis. Foraminal stenosis accompanied by a herniated disc was also included. All patients underwent continuous conservative treatment including medicine, physical therapy, and injection therapy for a minimum of 6 weeks before the operation. Patients who had multilevel pathologies and instability, and those who had undergone prior cervical surgery were excluded. Patients who required surgery for traumatic or neoplastic disease were also excluded from this analysis. The institutional review board of our hospital approved the study protocol (IRB No. : KBC 14130). Informed consent was waived by the board.
Pain was measured separately for the neck/shoulder and the arms according to self-assessment on a 10-point visual analogue scale (VAS). Functional disability was assessed using the author's translation of the original version of neck disability index (NDI)23) from January 2005 to December 2006. The published version of NDI for Korean-language speakers was used for evaluation since January 200717).
The site and severity of the lesion were verified by magnetic resonance imaging. For preoperative surgical planning, additional three-dimensional reconstructed computerized tomography was performed if needed. Lateral X-ray on neutral standing position was also examined to identify focal/global alignment and change in disc height. Dynamic lateral radiographs with flexion and extension postures were also taken to determine cervical instability.
The focal angulation was calculated by the Cobb's angle of the operated level, which was formed by lines drawn at the superior margin of the superior vertebra and the inferior margin of the inferior vertebra on a straight lateral film. The global angulation was defined as the Cobb's angle from C2 to C7, which showed whole alignment of the cervical spine. The disc heights were measured at the operated and upper adjacent levels. The disc height expressed as the disc height index (DHI) was calculated as the ratio of the mean of three point disc heights to the sagittal diameter of upper body at mid-vertebral level, as previously described13). Changes in the DHI of the operated or upper adjacent disc were normalized to the preoperative DHI and expressed as a percent DHI [(postoperative DHI/preoperative DHI)×100]. Measurement was repeated 2 times by an independent observer and the mean value was adopted. Radiological instability was defined as motion over 2 mm at the operated segment or any adjacent segments on dynamic imaging. Radiographs were analyzed using the PiViewSTAR program (INFINITT Healthcare, Seoul, Korea).
Outcomes after MI-PCF were analyzed using changes of clinical and radiological parameters from the baseline. Post-operatively, the parameters were measured at 3 months, 6 months, 1 year, and yearly thereafter. For the patients following more than 3 years, the last follow-up values were selected for analysis. Questionnaires were conducted by an independent clinical research coordinator at the time of follow-up. In cases of failed in clinic follow-up, data were collected over the phone.
Under general anesthesia, the patient was placed in a prone position with the neck slightly flexed and secured with a Mayfield head holding frame. Correct positioning of the incision was verified using C-arm fluoroscopy. A 2-cm longitudinal skin incision was made approximately 1 cm off midline at the level of the lesion site. Then subcutaneous tissue was dissected and underlying fascia was exposed. Before the serial dilatation using tubular dilators, incision of cervical fascia using a No.15 blade, and splitting of deep muscles such as semispinalis cervicis or multifidus and blunt dissection over the lamina and lateral mass were performed with the Metzenbaum scissors and Penfield dissector to identify the lamina-facet junction. Fluoroscopy was repeated to verify the operative level. Then a specially designed muscle retractor was placed into the surgical field and muscles were retracted to the lateral side (Fig. 1A). Medial to this retractor, small first dilator was inserted on the laminar-facet junction, the central location of a tubular retractor. Other larger dilators were then sequentially placed into the surgical field and an 18-mm diameter tubular retractor was applied over the dilators. The retractor was then docked in position at the lamina-facet junction after removal of the dilators and secured with a table mount system. Because of the muscle retractor located lateral to tubular retractor, the surgical view through the tube was quite clear without intervening muscle laterally (Fig. 1B). Using this method, angulation of the working tube intra-operatively was possible without slippage of muscle underneath the tube. Angular movement of the tube provided various surgical trajectories for adequate decompression under a limited surgical view through the tube.
The microscope was then introduced into the surgical field. A remnant of muscle and soft tissue overlying the facet was coagulated with a bipolar coagulator. Special care was taken not to violate the facet capsule. After careful detachment of the ligamentum flavum from the inferior edge of the superior lamina, the lamino-foraminotomy was started using a 2 mm bayoneted Kerrison punch. Lateral angulation of the working tube was done once the nerve root was identified. Foraminotomy was done using a long curved drill and a 1 mm bayoneted Kerrison punch. Angular surgical trajectory permitted thorough decompression along the nerve root, with maximal sparing of facet removal. This inclined undercutting of the facet provided 60-70% sparing of the facet3). The foraminotomy proceeded to the lateral pedicle border while ensuring that the nerve root was free of compression. If a herniated disc was entrained, the venous plexus surrounding the nerve root was carefully dissected and the root was gently retracted to expose the disc fragment. Using a micro hook dissector and pituitary forceps, the fragment was released and removed. After meticulous bleeding control and surgical field irrigation, Gelfoam was applied to the operative hole. Then the fascia and subcutaneous tissue were sutured closed, and the skin was closed with adhesive strips.
Mixed-effect model was used to test for differences from baseline in VAS scores of neck/shoulder, VAS scores of arm, and NDI measured repeatedly within a patient. Random effects were each parameter for patients, and error. Fixed effects were times at baseline and post-operative periods. Multiple comparisons between baseline and each follow-up time value were adjusted by Bonferroni method. The intraclass correlation coefficient (ICC) using the two-way mixed model with absolute agreement was used to determine intra-observer reliability for the radiological parameters. The values of the ICC can range from 0 to 1. The ICC above 0.75 was considered to represent excellent reliability7). Data were analyzed using the IBM SPSS 18.0 (IBM Co., NY, USA). p value<0.05 was considered statistically significant.
Adequate long-term clinical and radiological follow-up were available in 33 patients. Mean follow-up was 32.7 months [median, 24.0; interquartile range (IQR), 14-39]. Average age at the time of the surgery was 50.8 years (range, 34-73 years). Twenty-one patients were men and 12 were women. Four patients (12%) had surgery at C4-5, 11 patients (33%) had surgery at C5-6, and 18 patients (55%) had surgery at C6-7. Of the procedures performed, 22 (67%) were left sided, 11 (33%) were right sided. Nineteen patients (58%) had foraminotomy only, and 14 patients (42%) had additional discectomy for concomitant herniated disc. All patients tolerated the procedures well and responded to the surgery. No complications occurred and none of the patients required a revisional operation due to sustained or aggravated symptoms in the early post-operative period.
Mean baseline VAS scores of neck/shoulder (nVAS), VAS scores of arm (aVAS), and NDI were 5.3 (median, 5.5; IQR, 4.0-7.0), 5.4 (median, 5.5; IQR, 4.0-7.0), and 35.6 (median, 34.8; IQR, 24.9-42.7), respectively. The 3-month follow-up values [nVAS; 1.7 (median, 2.0; IQR, 0.0-3.0), aVAS; 1.6 (median, 1.0; IQR, 0.0-3.0), NDI; 14.7 (median, 13.3; IQR, 4.4-16.0)] showed significant improvements vs. the baseline values (p<0.001, respectively). Long-term trend analysis using the mixed-effect model showed that both VAS scores improved significantly in the early post-operative period (3 months) and maintained at plateau with time, and NDI improved significantly post-operatively and tended to decrease more gradually over the follow-up period (p<0.001) (Fig. 2).
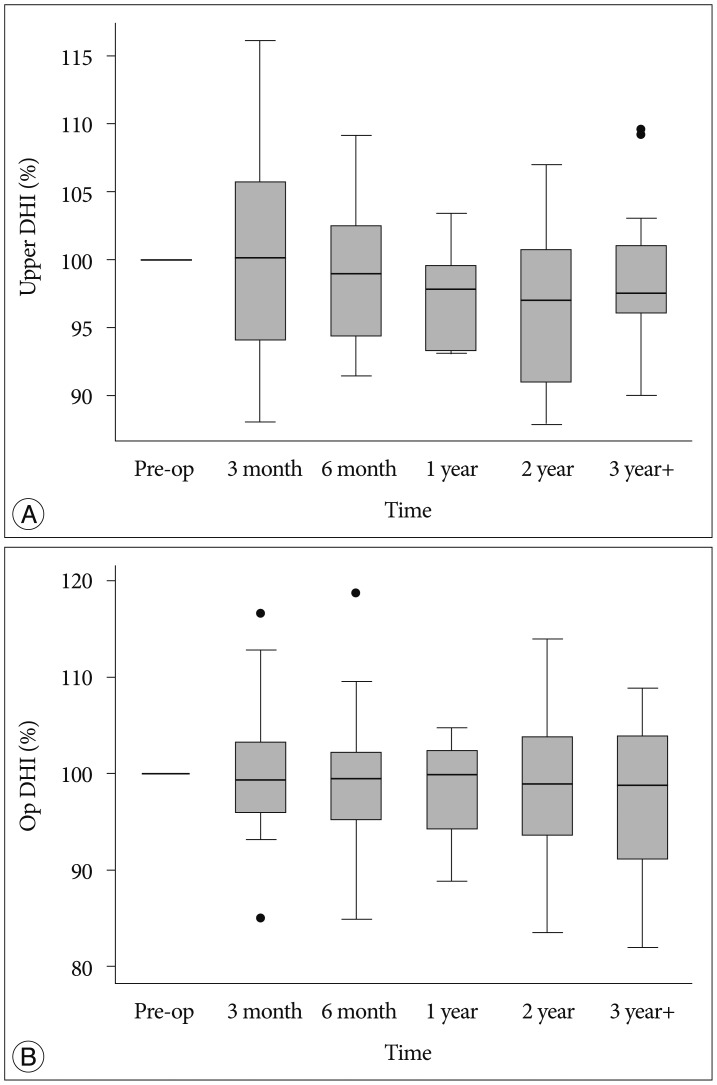
Baseline pre-operative mean focal angulation was 2.3° (median, 3.0; IQR, -0.7-5.1), and the mean global angulation between C2 and C7 was 6.3° (median, 5.1; IQR, -1.3-13.3). Baseline mean disc height at upper adjacent level was 6.1 mm (median, 6.2; IQR, 5.5-7.0), and the mean disc height at operated level was 6.0 mm (median, 6.0; IQR, 5.4-6.7). Changes in post-operative follow-up values of disc height at upper adjacent or operated level were calculated with percent DHIs. The 3-month follow-up values of focal and global angulation increased slightly, compared with the baseline values, despite no statistical significance, reflecting the slight restoration of lordosis. The other follow-up values were maintained without significant changes (Fig. 3). Overall, there were no statistically significant changes in focal and global alignment over the follow-up time (p=0.797, p=0.137, respectively). Percent DHIs of the upper adjacent or operated disc were maintained without changes with time, suggesting that no further degenerations developed at the discs after operation (p=0.186, p=0.758, respectively) (Fig. 4). The ICCs of radiological parameters showed excellent intra-observer reliability (focal angulation : 0.95, global angulation : 0.99, DHIs of the upper adjacent disc; 0.98, DHIs of the operated disc; 0.98).
Follow-up images on dynamic X-ray showed no instability at operated, or any adjacent segments causing clinical symptoms. There were 2 additional surgeries after initial MI-PCF during the follow-up. A 54-year-old man who underwent MI-PCF on the left side of C6-7, five and half years later, needed two-level PCF on the right side of C5-6 and C6-7. The other patient had received a left C5-6 MI-PCF and complained of right arm radiculopathy during the follow-up. She had an ACDF at C6-7 five years after the initial surgery.
PCF has been widely used as the surgical treatment of lateral cervical disc herniations and foraminal stenosis since the 1940s10,20,21). The advantages of this posterior approach include direct and targeted decompression of the involved nerve root under direct visualization, without disruption of the disc space itself and avoidance of fusion. Moreover, it avoids the possible anterior approach-related problems. Despite these theoretical advantages (over anterior approaches) to treat cervical radiculopathy, open PCF requires a long midline incision with extensive subperiosteal dissection to detach deep muscles, such as semispinalis and mutifidus, acting as dynamic stabilizers of the lamina and facet joint, which may cause long lasting postoperative neck spasm and pain12). Other concerns for PCF are post-operative instability at the surgical level, and loss of lordosis (kyphosis) that may accelerate the disc degeneration due to the wide detachment of muscle and ligament surrounding the facet and excessive facet joint resection2,5,14).
Since Foley and Smith8) first described a microendoscopic discectomy using a tubular retractor for the treatment of lumbar radiculopathy, the technique was adopted for cervical spine disease1,6). Minimal access techniques, under a small surgical incision, using a percutaneous tubular retractor system and a microscope or endoscope, allows for a safe and effective decompression of neural structures, while preserving anatomical structures, thus maintaining spinal stability. However, MI-PCF has a long and steep learning curve and may be associated with an increased risk of peri-operative complications related to the placement of a tubular retractor and to a limited surgical corridor through the retractor19). Blind serial dilatation of the paraspinal muscle through the thick posterior cervical fascia may be associated with unintended placement of K-wire or small diameter dilator, into the interlaminar space causing injury to the dura or spinal cord. Laterally placed K-wire or dilators and resultant location of misplaced tubular retractor can cause nerve root or vertebral artery injury and loss of a surgical landmark, the laminar-facet junction. The surgery via improperly placed retractor and loss of the landmark may inadvertently cause excessive facet removal, resulting in postoperative instability.
To solve this limitation, before the serial dilatation, incision of cervical fascia and blunt dissection using a scissor or a dissector over the lamina and lateral mass provide direct identification of the laminar-facet junction, the central location of a tubular retractor15,16). Dilatations centered on the surgical landmark provide proper positioning of the tubular retractor that facilitates precise removal of the facet joint and root unroofing in a limited and narrow surgical field through the retractor. To achieve safe and effective decompression through a limited surgical corridor, the author performed modified MI-PCF to do partial undercutting of facet with a specially designed muscle retractor located lateral to the tubular retractor. This method provided a wider tilted surgical view through the angulation of the working tube intra-operatively, for adequate decompression without intervening muscle from the lateral side. And this facet-sparing (60-70% of total facet) approach provided additional stability with maximal root decompression3), which may result in good long term clinical and radiological outcomes.
Clinical studies have reported symptomatic relief ranging from 87% to 97% for the initial outcome of these minimally invasive approaches1,6). Recently, in a systematic review comparing minimally invasive and open PCF, MI-PCF provided equivalent efficacy with a significant decrease in intra-operative blood loss, surgical time, use of analgesics, length of hospitalization, and other morbidities due to wide exposure of surgical field, compared to open PCF4). As such, many studies have shown that MI-PCF is a good surgical option in the treatment of cervical radiculopathy in the initial postoperative period; however, only a few studies have published the long-term clinical outcomes. Recently, in a mean of 24.5 months follow-up, statistically significant improvements in VAS scores and NDI were seen in patients at 1 year, 2 year, and 3-6 years post-operatively16). A retrospective analysis for a mean of 32.1 months follow-up reported that VAS scores and NDI improved significantly from baseline immediately post-operatively and maintained to decrease over the follow-up period22).
Complications related to the MI-PCF are rare. Complication rates after this operation ranged from 2% to 9%, with cerebrospinal fluid leaks, infections, wound hematoma, and radicular numbness secondary to nerve manipulation9,11,18,22). Another issue is delayed symptomatic operated or adjacent disc degeneration requiring a fusion surgery. From 2.6% to 7.1% of patients required an ACDF at the operative or adjacent level on an average 44.4 to 56 months after the initial MI-PCF16,22).
In the present study, the author presented long-term results of MI-PCF for cervical radiculopathy using both clinical and radiological parameters. Mixed-effect model was used to adjust for missing data for the parameters. This model was useful in the retrospective analysis of this prospectively designed cohort with long term follow-up. VAS scores improved significantly from baseline in the immediate post-operative period (3 months) and maintained at plateau with time (p<0.001). NDI improved significantly post-operatively and tended to decrease more gradually during the follow-up (p<0.001). This result was comparable to other long term clinical outcomes after MI-PCF16,22).
To the author's knowledge, this is the first report to address long-term radiologic outcome after MI-PCF. Jagannathan et al.14) described long term radiological follow-up after unilateral single-level open PCF. The open technique involved a more radical facetectomy and pediculotomy with a subperiosteal stripping of muscles. The study showed no statistically significant changes in sagittal alignment or disc height in the cervical spine with time. However, they reported post-operative instability at the surgical level was 8 patients (4.9%), of which 7 patients had no further treatment.
The present series showed no changes of focal and global angulation from baseline on follow-up. Rather, slight restoration of lordosis in the early post-operative period was noted, caused by relaxation of neck/shoulder muscles, due to pain control. The disc height in the upper adjacent or operated level was well maintained post-operatively during the follow-up, suggesting that no further disc degenerations occurred after surgery. Radiological instability on dynamic X-ray was not noted at the operated or any adjacent segments. The modified MI-PCF using the specially designed retractor might result in lower incidence of radiological instability while preserving more facet during adequate decompression, compared with open technique with more radical removal of facet as described above. Same site recurrence was not noted, and adjacent segment disease requiring additional surgery occurred in 6% (2/33) of patients on the contra-lateral side. Despite lack of evidence related to these occurrences with the initial surgery, the rate was comparable to another long-term follow-up study on operated or adjacent segments disease following single-level open PCF. The study showed symptomatic operated and adjacent segment disease in 3.3% (10/303) and 4.9% (15/303) of patients, respectively, including 12 (4.0%) of 303 patients requiring additional surgery5).
This observational study of a long-term follow-up period, involved a relative small number of patients. To confirm the current results of MI-PCF for cervical radiculopathy, prospective controlled comparative trials in a larger population with other techniques such as open PCF, ACDF, or cervical arthroplasty are mandatory.
Acknowledgements
Ms. Mi-yeon Lee and Keun-young Park provided the support for data and statistical analysis. The author thanks for their commitment to this study.
References
1. Adamson TE. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy : results of a new technique in 100 cases. J Neurosurg. 2001; 95(1 Suppl):51–57. PMID: 11453432.

2. Cağlar YS, Bozkurt M, Kahilogullari G, Tuna H, Bakir A, Torun F, et al. Keyhole approach for posterior cervical discectomy : experience on 84 patients. Minim Invasive Neurosurg. 2007; 50:7–11. PMID: 17546536.

3. Chang JC, Park HK, Choi SK. Posterior cervical inclinatory foraminotomy for spondylotic radiculopathy preliminary. J Korean Neurosurg Soc. 2011; 49:308–313. PMID: 21716632.

4. Clark JG, Abdullah KG, Steinmetz MP, Benzel EC, Mroz TE. Minimally invasive versus open cervical foraminotomy : a systematic review. Global Spine J. 2011; 1:9–14. PMID: 24353931.
5. Clarke MJ, Ecker RD, Krauss WE, McClelland RL, Dekutoski MB. Same-segment and adjacent-segment disease following posterior cervical foraminotomy. J Neurosurg Spine. 2007; 6:5–9. PMID: 17233284.

6. Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy : an initial clinical experience. Neurosurgery. 2002; 51(5 Suppl):S37–S45. PMID: 12234428.
7. Fleiss JL. Reliability of measurement : The design and analysis of clinical experiments. Hoboken, NJ: John Wiley & Sons, Inc.;1999. p. 1–32.
8. Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997; 3:301–307.
9. Franzini A, Messina G, Ferroli P, Broggi G. Minimally invasive disc preserving surgery in cervical radiculopathies : the posterior microscopic and endoscopic approach. Acta Neurochir Suppl. 2011; 108:197–201. PMID: 21107959.
10. Frykholm R. Deformities of dural pouches and strictures of dural sheaths in the cervical region producing nerve-root compression; a contribution to the etiology and operative treatment of brachial neuralgia. J Neurosurg. 1947; 4:403–413. PMID: 20260241.

11. Gala VC, O'Toole JE, Voyadzis JM, Fessler RG. Posterior minimally invasive approaches for the cervical spine. Orthop Clin North Am. 2007; 38:339–349. abstract v. PMID: 17629982.

12. Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. A noticeable complication. Spine (Phila Pa 1976). 1996; 21:1969–1973. PMID: 8883196.
13. Inoue H, Ohmori K, Miyasaka K, Hosoe H. Radiographic evaluation of the lumbosacral disc height. Skeletal Radiol. 1999; 28:638–643. PMID: 10591927.

14. Jagannathan J, Sherman JH, Szabo T, Shaffrey CI, Jane JA. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease : a single-surgeon experience with a minimum of 5 years' clinical and radiographic follow-up. J Neurosurg Spine. 2009; 10:347–356. PMID: 19441994.

15. Kwon YJ. Early surgical results of minimally invasive posterior foraminotomy using tubular retractor for cervical radiculopathy. J Korean Soc Spine Surg. 2007; 14:67–72.

16. Lawton CD, Smith ZA, Lam SK, Habib A, Wong RH, Fessler RG. Clinical outcomes of microendoscopic foraminotomy and decompression in the cervical spine. World Neurosurg. 2014; 81:422–427. PMID: 23246739.

17. Lee H, Nicholson LL, Adams RD, Maher CG, Halaki M, Bae SS. Development and psychometric testing of Korean language versions of 4 neck pain and disability questionnaires. Spine (Phila Pa 1976). 2006; 31:1841–1845. PMID: 16845361.

18. Minamide A, Yoshida M, Yamada H, Nakagawa Y, Maio K, Kawai M, et al. Clinical outcomes of microendoscopic decompression surgery for cervical myelopathy. Eur Spine J. 2010; 19:487–493. PMID: 19956984.

19. Perez-Cruet MJ, Fessler RG, Perin NI. Review : complications of minimally invasive spinal surgery. Neurosurgery. 2002; 51(5 Suppl):S26–S36. PMID: 12234427.
20. Scoville WB, Dohrmann GJ, Corkill G. Late results of cervical disc surgery. J Neurosurg. 1976; 45:203–210. PMID: 939979.

21. Scoville WB, Whitcomb BB. Lateral rupture of cervical intervertebral disks. Postgrad Med. 1966; 39:174–180. PMID: 5903648.

22. Skovrlj B, Gologorsky Y, Haque R, Fessler RG, Qureshi SA. Complications, outcomes, and need for fusion after minimally invasive posterior cervical foraminotomy and microdiscectomy. Spine J. 2014; [Epub ahead of print].

23. Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991; 14:409–415. PMID: 1834753.
Fig. 1
Specially designed retractor and its application into the surgical field. A specially designed muscle retractor (arrow) is located lateral to tubular retractor (A). The operative field through the tube is clear without intervening muscle laterally, due to lateral retraction of the muscle with the retractor (arrow) (B).
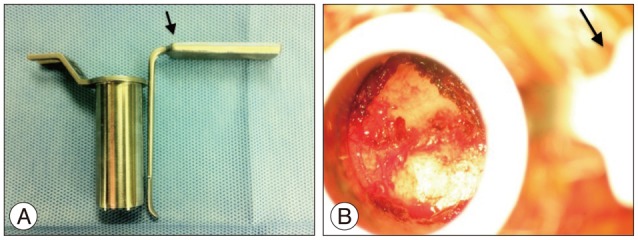
Fig. 2
Clinical outcomes measured by visual analogue scale (VAS) and neck disability index (NDI). VAS scores of neck/shoulder (nVAS) (A) and arm (aVAS) (B) decrease immediately in the early post-operative period and maintain at plateau with time. NDI (C) tends to decrease more gradually over the follow-up period. The bottom and top of the box are the first quartile and third quartile, and the band inside the box is the median. The circles represent outliers beyond 1.5 interquartile ranges.
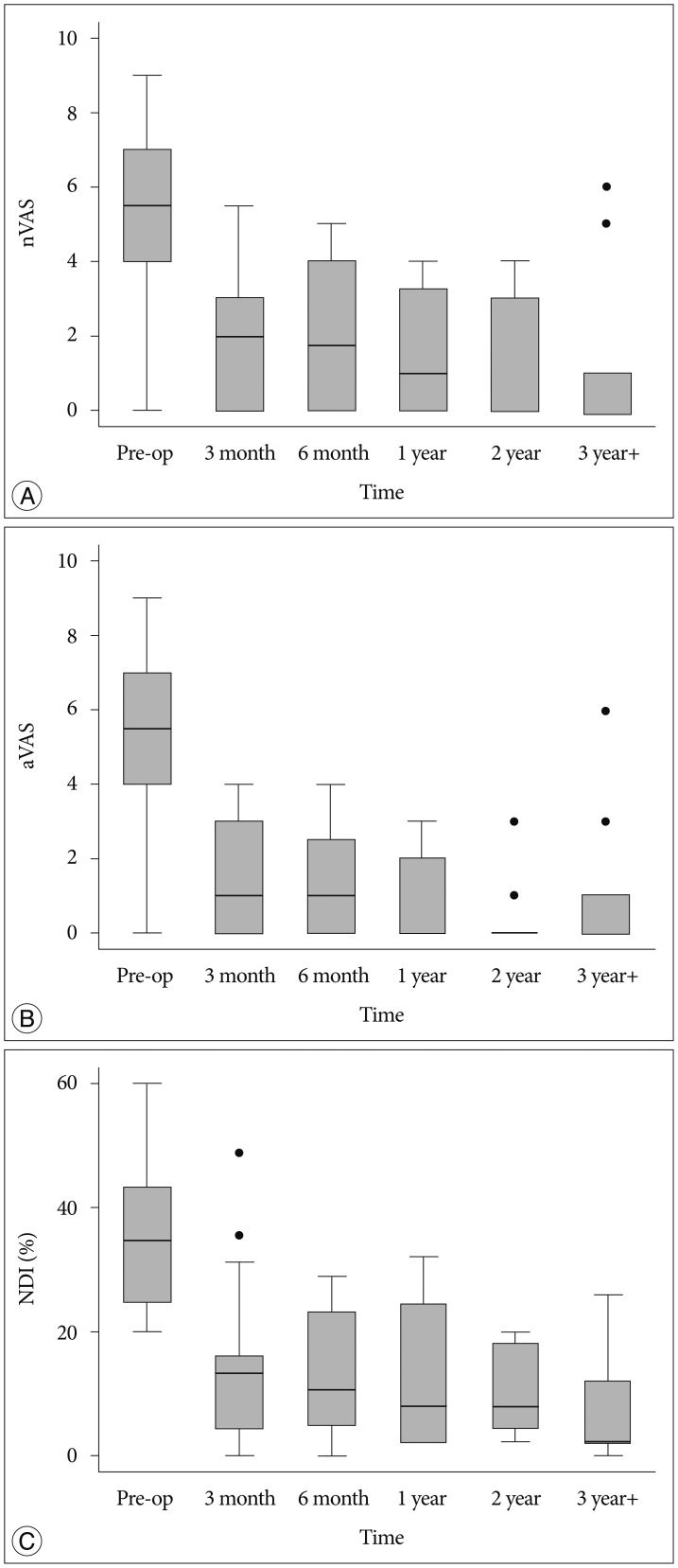
Fig. 3
Radiological outcomes measured by focal and global angulation. The 3-month follow-up values of focal (A) and global (B) angulation increase slightly from the baseline values, and the other follow-up values are maintained without significant changes. The bottom and top of the box are the first quartile and third quartile, and the band inside the box is the median. The circles represent outliers beyond 1.5 interquartile ranges.
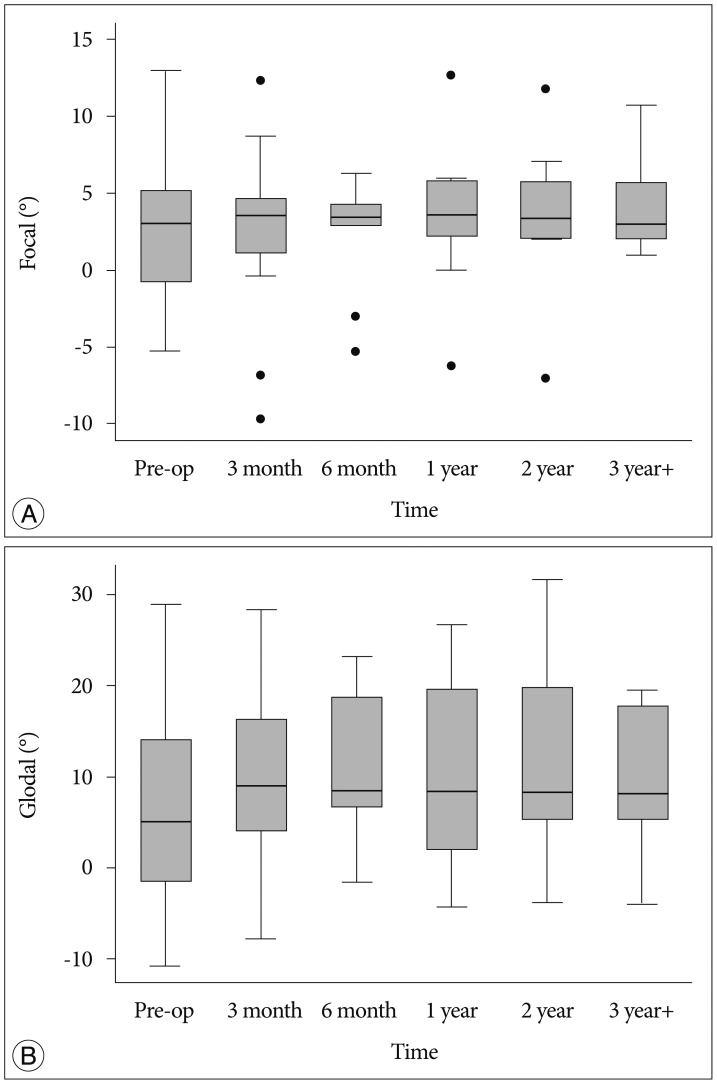
Fig. 4
Radiological outcomes measured by disc height index (DHI). Percent DHIs of the upper adjacent (upper DHI) (A) or operated (Op DHI)(B) disc are maintained without changes during the follow-up. The bottom and top of the box are the first quartile and third quartile, and the band inside the box is the median. The circles represent outliers beyond 1.5 interquartile ranges.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download