CASE REPORT
A 53-year-old woman presented with right periorbital swelling and pain in eyeball over 2 months. She had known Grave's disease but there were neither other neurologic deficits nor limitation of the extraocular muscle movement. Visual acuity and field were normal findings. Magnetic resonance (MR) imaging revealed a well-enhancing mass surrounding optic nerve and ocular muscles in the right retrobulbar area (
Fig. 1). We suspected lymphoma or pseudotumor, and decided to explore because of persistent ocular pain and purpose of pathological confirmation. We approached via right frontotemporal craniotomy. After opening of the periorbita, we observed the bulky mass intermingled with right medial rectus muscle and superior oblique muscle. It was hard to define the exact origin of tumor in the medial aspect of the orbit. Therefore, we excised the voluminous mass appearing grossly like hypertrophied muscle and subtotal removal of the lesion was attained, leaving its remnant to avoid the injury to extraocular muscles.
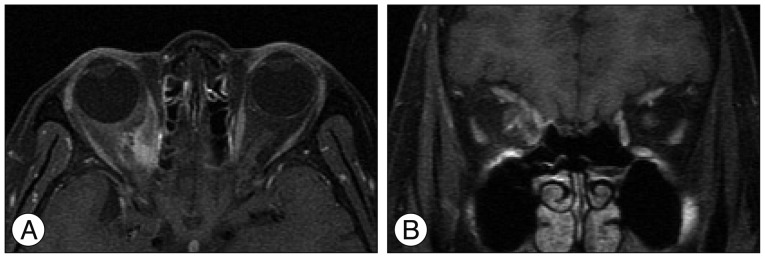 | Fig. 1Preoperative orbital enhanced magnetic resonance (MR) images. A : Axial MR image showing a well-enhanced mass in the medial portion of right orbit. B : Coronal MR image demonstrating a well-enhanced mass in the supero-medial portion of right orbit. 
|
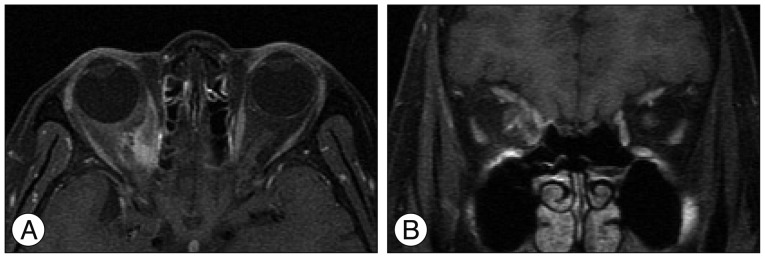
Surgical specimen was a dark brownish measuring 1.3×1.0 cm in size, and it was proven to be the findings of the skeletal muscle suspecting the right medial rectus muscle on the initial pathological report. On the microscopic examination, specimen showed the findings composed of well-differentiated skeletal muscle and nerve fibers. Each bundle size was quite variable (
Fig. 2A). According to the immunohistochemical report, the tumor was immunoreactive to S-100 protein, which is common marker of neural tissue (
Fig. 2B). Complex network of myelinated nerve fibers associated with well-differentiated striated muscle fiber were observed by Luxol-fast blue staining (
Fig. 2C). After operation, her optic nerve function was well preserved and ocular pain was improved, but she developed diplopia possibly by the injury of medial rectus muscle. Even though she has been undergone reconstructive surgery for the medial rectus muscle by ophthalmology department, her diplopia was persisted. There was no recurrence of tumor about 10 years after surgery.
 | Fig. 2Photomicrograghs of the resected lesion. A : H & E staining shows nerve fibers admixed with skeletal muscle (×200). B : Immunohistochemical staining reveals diffuse immunoreactivity to S-100 protein suggesting neural elements (×200). C : Luxol-fast blue staining demonstrates dark bluish colored muscle fibers in the striated fashion (×200). 
|
Go to :

DISCUSSION
BTTs are extremely rare reported that less than 20 cases have been reported in the English language literatures
2,
3,
4,
5,
6,
14). The name triton has been originated from the amphibian triton salamander, in which the normal nerve seems to induce regeneration of skeleton muscle
8). These tumors commonly occur in infants and children, however, it has been rarely reported in adults
13,
14). The most common sites of invasion are the large peripheral nerves, especially the brachial and sciatic nerves
16). A few cases been reported in the head and neck region
5,
6,
11,
13). These tumors have about 2.4 : 1 female predominance in literature reviews
6).
Daley et al.
5) have analyzed previous 9 cases developed in the head and neck of children and adults, and they suggested that BTTs have been categorized into two groups by their location; 1) a more aggressive central type and 2) a non-aggressive peripheral type. A more aggressive central type involves large intracranial nerve or infratemporal fossa nerve trunks with extension into multiple adjacent spaces, sometimes associated with muscle atrophy and weakness, and usually associated with destructive growth. Involvement of the fifth cranial nerve in or near the middle cranial fossa (specifically Meckel's cave) with extension through the foramen ovale into the infratemporal fossa is most common
4,
12,
13,
14,
15). These cases typically appear infants and children, and require extensive surgical treatment.
A non-aggressive peripheral lesions are subcutaneous or submucosal, non-encapsulated lumps that are asymptomatic, non-destructive, and enlarge slowly, if at all. They are found at a later age, including adulthood
6,
11). Surgical excision is simple and curative. Daley et al.
5) also reviewed 9 cases with BTTs in the head and neck, and residual or recurrent cases have been developed in one case of 5 central BTTs associated with trigeminal nerve and only case of 4 peripheral BTT, respectively. Our case may be categorized into the former type. Four theories have been suggested to explain the origin of this unusual tumor; 1) Hamartomatous growth of muscle spindles : Markel and Enzinger
8) suggested that these lesions may represent only muscle spindle hamartomas because of its structural resemblance to the neuromuscular spindle organ. 2) Entrapment of skeletal muscle fibers within nerves during embryogenesis : This theory was initially postulated by Markel and Enzinger
8) after treating a patient with a tumor composed of mature muscle cells and fibrous tissue in the vicinity of the sciatic nerve. Louhimo and Rapola
7) suggested that mesenchymal tissue might become incorporated by the extending peripheral nerves and ensheathed by the neurilemma. 3) Differentiation of neuroectoderm into skeletal muscle : This theory was proposed initially by Masson
9). He suggested that neuroectodermal cells could undergo mesenchymal differentiation. This is based on his observation of the histological development of the cranial meninges and intraocular muscles, both of which are derivatives of the ectodermal cells, the ectomesenchyma
9,
10). 4) Epigenetic or acquired alteration of the motor end-plate : This recent theory was suggested by Daley et al.
5). They propose that there is an alteration, either epigenetic (infants) or acquired (adults), in which there is a motor end plate/synaptic junction defect. Thereafter, this leads to reactive proliferation of neural and skeletal muscle tissue in an organoid pattern. They indicated two meaningful points : 1) There would be no contraction of the tumor mass despite the abundant highly innervated skeletal muscle. 2) The nerve involved would be a motor nerve. No single theory adequately explains all of reported neuromuscular hamartoma.
Clinical manifestations are variable ranged from asymptomatic to pain or developement of neurologic deficits. Most BTTs do not cause symptom, however, depending on the site of involvement, pain, neurologic dysfunction in the form of muscle weakness, parasthesia, and headache including oculomotor ophthalmoplegic migraine, could be occured
1,
4,
14). Radiographic features of BTT show a wide spectrum. Most tumors enhance after intravenous contrast infusion on the computed tomography scans and MR images. Histopathologically, these tumors are multi-nodular, subdivided by collagenous connective tissue into smaller nodules and fascicles. The fascicles are comprised of mature striated muscle fibers intimately associated with nerve fibers, and enclosed within the same perimysial-like fibrous sheath
2).
Treatment options are excision with more aggressive central type and conservative for the peripheral tumors. Incomplete resection could relieve symptoms. Post-resection nerve palsies are always crucial, thus, preservation of neural function is essential
3,
5,
8,
16). In our case, patient developed diplopia postoperatively. We must consider whether aggressive treatment or not for patients satisfaction and favorable prognosis. Although prognosis is good in the most cases, recurrence has been reported
6). Therefore, we should be kept in mind the close follow-up of patients.
Go to :

CONCLUSION
Although this tumor rarely occurs, its frequent connection with large nerves or cranial nerves often makes complete resection difficult or impossible. Moreover, surgical treatment of these tumors may develop residual neural dysfunction. In consideration of their extremely low recurrence and benign lesion, BTT should be removed subtotally and save the involved nerve to avoid neurological deficits.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download