Abstract
Objective
This study analyzed clinical and radiological outcomes of a zero-profile anchored spacer (Zero-P) and conventional cage-plate (CCP) for single level anterior cervical discectomy and fusion (ACDF) to compare the incidence and difference of postoperative dysphagia with both devices.
Methods
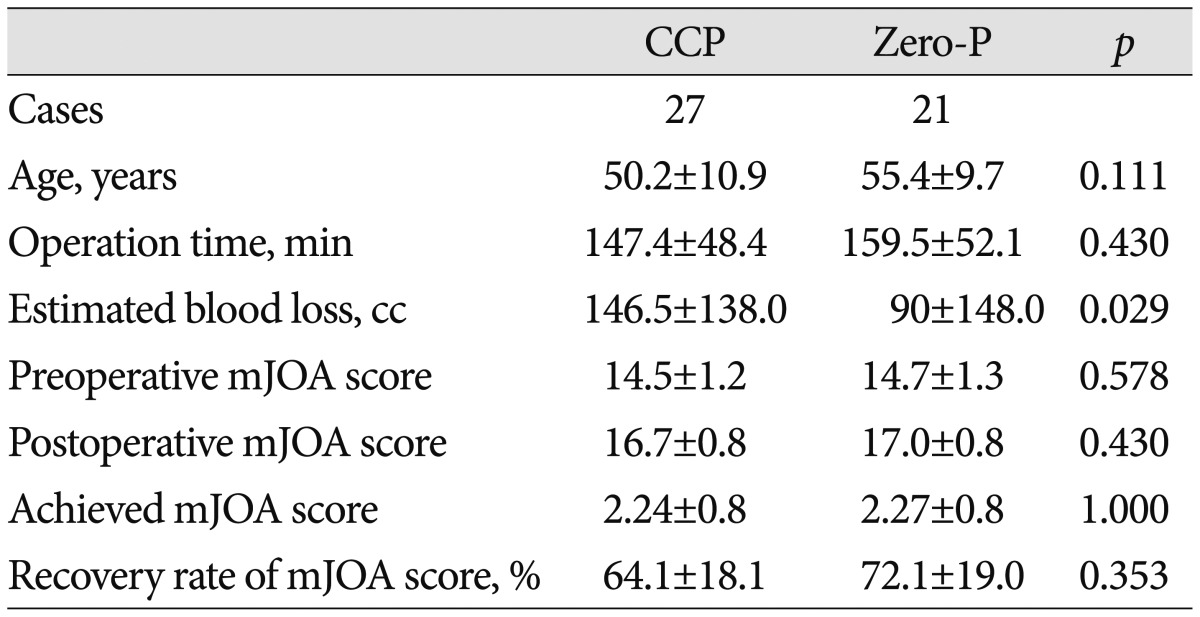
We retrospectively reviewed our experiences of single level ACDF with the CCP and Zero-P. From January 2011 to December 2013, 48 patients who had single level herniated intervertebral disc were operated on using ACDF, with CCP in 27 patients and Zero-P in 21 patients. Patients who received more than double-level ACDF or combined circumferential fusion were excluded. Age, operation time, estimated blood loss (EBL), pre-operative modified Japanese Orthopaedic Association (mJOA) scores, post-operative mJOA scores, achieved mJOA scores and recovery rate of mJOA scores were assessed. Prevertebral soft tissue thickness and postoperative dysphagia were analyzed on the day of surgery, and 2 weeks and 6 months postoperatively.
Since the introduction of anterior cervical discectomy and fusion ACDF in 19584), the procedure has become the gold-standard operation for single or multiple level degenerative cervical spondylosis, especially for the patients with herniated intervertebral cervical discs9,12). Earlier, iliac bone graft was used after removal of cervical intervertebral discs. With the advent of iliac bone graft, cervical cages were introduced to avoid donor site complications and reduce patient pain. More recently and with extensive surgeon-mediated modifications combined with technological refinements, the anterior cervical plate cage technique has gained global popularity.
Advantages of this technique include improved sagittal alignment, prevention of interbody graft dislocation, and increased interbody fusion rate and stability8,14,16). However, the application of anterior cervical plate may face with some complications ; increased incidence of dysphagia, tracheo-esophageal injuries, and adjacent level degeneration2,7,13,18).
To lessen potential complications while maintaining the benefits of anterior cervical plating, the zero-profile anchored spacer (Zero-P; Synthes GmbH, Oberdorf, Switzerland) was invented for use in patients with degenerative cervical spondylosis (Fig. 1A).
The present study analyzed clinical outcomes and radiological findings after application of the Zero-P device and the conventional cage-plate (CCP) device for single level ACDF, and sought to compare the incidence and difference of postoperative dysphagia for both devices.
This retrospective and comparative study of clinical outcomes initially involved 92 patients who received single level ACDF using the CCP or Zero-P device. Of these, 19 patients were excluded because of identified use of a different procedure such as combined ACDF with circumferential fusion and cage-only ACDF. Another 25 patients were excluded since surgery involved two or more levels (adjacent or distant). Thus, 48 patients were included in this study (30 men, 18 women; mean age 52.3 years, range, 36-78 years). All patients suffered from typical symptoms, such as posterior neck pain, radiating pain, and limb numbness. These patients were divided into two groups based on the device used : the CCP group comprised 27 patients and the Zero-P group comprised 21 patients. Most of the patients were followed-up around 6 months post-operatively; thus, this study focused on short-term results. The characteristics of both groups are summarized in Table 1-1.
Zero-P utilized the standard anterior Smith-Robinson approach. The patients were in the supine position with slight head extension. After routine skin preparation and drape, a skin incision was made with a left side approach. Gently dissection identified the platysma, which was divided in line with the skin incision using a monopolar coagulator. The sternocleidomastoid was retracted laterally to allow palpation for deep structures of neck and extension of exposure. After confirmation of operation levels, Casper distractor (Aesculap, Burlingame, CA, USA) blade was placed beneath the elevated longus colli. Disc material was removed using a pneumatic drill and Kerrison punch. After trial spacers were used to confirm the suitable polyetheretherketone (PEEK) spacer, a Zero-P implant filled with allograft material was inserted at the operation level. Fluoroscopy at the antero-posterior and lateral view was used to establish the best position for the Zero-P spacer. The first pilot hole was drilled with an aiming device and a one-step first locking screw was fixed through the first pilot hole with a torque limiter (1.2 Nm). The remaining three lock-ing screws were similarly fixed. The locking screws formed a bone wedge with a 40±5° cranial/caudal angle and 2.5° medial/lateral angle. Their diameter was 3 mm. Lengths of 12, 14, and 16 mm were assessed; 16 mm screws provided the best suitable length in most patients. A plain film image of a representative successful procedure is shown in Fig. 1B.
Surgery similarly utilized the standard anterior Smith-Robinson approach and similar intraoperative processes. A PEEK cage with a Zephir anterior cervical plate (Medtronic Spine, Minneapolis, MN, USA) was used as the CCP system. The Zephir plate was 15 mm in width and about 1.6 mm in thickness. The length varied from 22.5 mm to 70 mm with a 2.5 mm differential, with the suitable length determined on a case-by-case basis.
All cases were routinely examined on the admission date or pre-operative work-up period for the operation with cervical spine plain film with antero-posterior, lateral, and oblique views, with excessive flexion and extension series, computed tomography (CT) and magnetic resonance imaging (MRI) used for analysis of radiologic findings. Follow-up was ≥6 months on an outpatient basis; plain film examination, CT scan, and MRI were also performed. Prevertebral soft tissue thickness was assessed during the pre-operative work-up period, the day of surgery, and 2 weeks and 6 months post-operatively. Using the lateral images of cervical plain film, prevertebral soft tissue thickness was calculated as the mean value of the distance between the anterior surface of each vertebral body or plate and the air shadow of the airway (Fig. 2). These data were subtracted from the pre-operative data to identify the difference between the CCP and Zero-P groups. All radiological image analyses were performed three separate times by an independent person to ensure accuracy.
Clinical outcomes were evaluated pre-operatively on the date of admission and post-operatively 6 months after surgery with the modified Japanese Orthopaedic Score (mJOA) proposed by Benzel3). The achieved mJOA score was calculated as postoperative mJOA-preoperative mJOA. Recovery rate (RR, %) was also calculated as [(postoperative mJOA-preoperative mJOA)/(18-preoperative mJOA)]×1006). The operation time and estimated blood loss (EBL) were also estimated.
Statistical analyses were performed using PASW stastistics 18.0 software (SPSS Inc., Chicago, IL, USA). All values are expressed as the mean±standard deviation. The Mann-Whitney test was performed for quantitative analyses. Chi-square test and the Fisher's exact test were performed for qualitative analyses. A p value <0.05 was considered statistically significant.
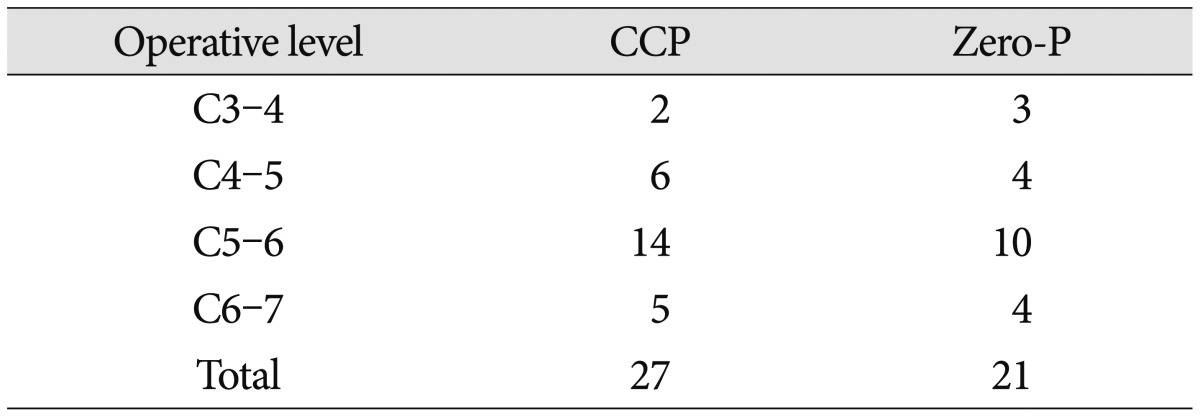
The location of surgery was C3-4 (CCP, n=2; Zero-P, n=3), C4-5 (CCP, n=6; Zero-P, n=4), C5-6 (CCP, n=14; Zero-P, n= 10), and C6-7 (CCP, n=5; Zero-P, n=4) (Table 1-2).
The CCP group had a mean EBL of 146.5±138 cc and an average operation time was 147.4±48.4 minutes. Pre- and postoperative mJOA score of the CCP group was 14.5±1.2 and 16.7±0.8, respectively. Achieved mJOA score and recovery rate of mJOA score was 2.24±0.8% and 64.1±18.1%, respectively. The Zero-P group had a mean EBL of 90±148 cc and an average operation time was 159.5±52.1 minutes. Pre- and postoperative mJOA score of the Zero-P group was 14.7±1.3 and 17.0±0.8, respectively. Ac-hieved mJOA score and recovery rate of mJOA score was 2.27±0.8% and 72.1±19.0%, respectively. All clinical outcomes were statistically similar between the groups, except for EBL (p=0.029).
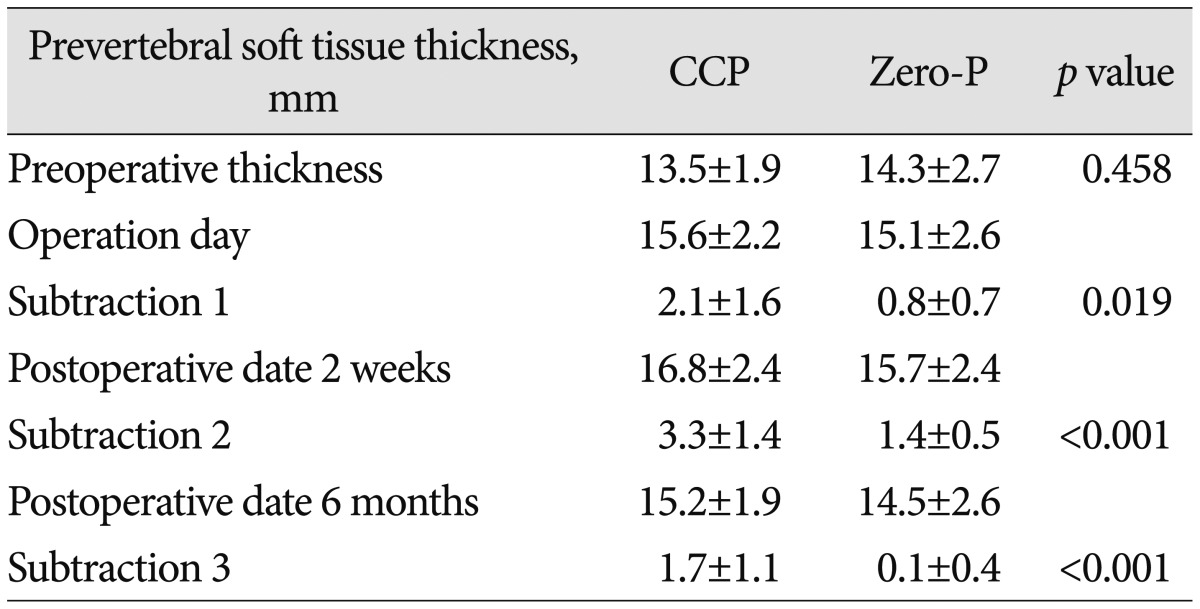
Concerning prevertebral soft tissue thickness, the pre-operative, immediate post-operative, 2 weeks post-operative, 6 months post-operative value was 13.5±1.9, 15.6±2.2, 16.8±2.4 and 15.2±1.9 mm in the CCP group, respectively, and 14.3±2.7, 15.1±2.6, 15.7±2.4, and 14.5±2.6 mm in the Zero-P group, respectively. The calculated subtraction was 2.1±1.6 mm as subtraction 1, 3.3±1.4 mm as subtraction 2, and 1.7±1.1 mm as subtraction 3 in the CCP group, and 0.8±0.7 mm as subtraction 1, 1.4±0.5 as subtraction 2, and 0.1±0.4 as subtraction 3 in the Zero-P group. Although the initial prevertebral soft tissue thicknesses of the both groups were statistically the same, their subtractions were statistically different (Table 2).
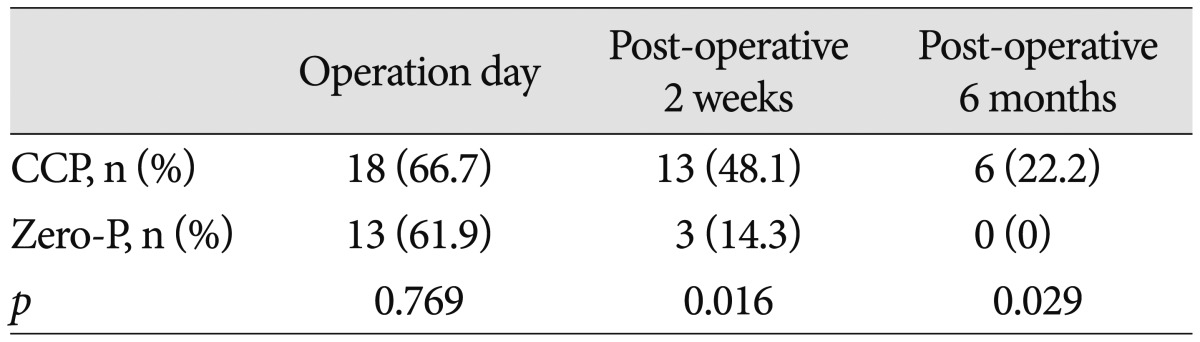
Post-operative dysphagia was determined on the day of operation, 2 weeks post-operatively, and 6 months post-operatively date. In the CCP group, 18 patients immediately complained of dysphagia on the operation day, 13 patients had dysphagia 2 weeks post-operatively, and 6 patients still suffered from dysphagia 6 months after the operation. In the Zero-P group, 13 patients immediately complained of dysphagia on the operation day, 3 patients had dysphagia 2 weeks post-operatively, and no patient had dysphagia 6 months after the operation (Table 3).
ACDF has advantages or complications. Chronic dysphagia is a common complication of ACDF; authors have reported this complication with a wide variability from 3% up to 21%2,7,10,15). Post-operative soft tissue swelling, hematoma at the operative site, esophageal injury, and adhesion formation around implanted cervical plates may be possible reasons for dysphagia5). Dysphagia has been related to the thickness of the anterior plate at the fusion level10). The Zero-P device has a smaller volume than the CCP device, which allows a smaller incision. The smaller incision allows more limited resection, less exposure, and avoids mechanical stimulus to the related structures. In this study, we focused on the post-operative radiologic changes of prevertebral soft tissue swelling after ACDF with both devices. We hypothesized that this swelling would be comparatively mild in the Zero-P group. Analyzing the radiologic finding of cervical plain films, the Zero-P device definitely had an advantage of mild post-operative prevertebral soft tissue swelling (p<0.001). We also confirmed that the incidence of chronic dysphagia was low in the Zero-P group (0%) compared to the 22.2% in the CCP group. Pre-viously described above, other studies have reported an incidence of chronic dysphagia of ≥20% after ACDF. Thus, we conclude that application of the Zero-P assures mild post-operative prevertebral soft tissue swelling and less dysphagia after ACDF.
To date, many authors also have identified that application of the Zero-P spacer can provide favorable clinical outcomes after ACDF. Wang et al.17) reported a retrospective study that both the Zero-P spacer and traditional titanium plate with cage were effective for single level cervical spondylotic myelopathy, but that the Zero-P spacer was associated with less dysphagia. The authors also conjectured that application of the Zero-P spacer might reduce adjacent level spondylosis since these devices conveyed less stress to adjacent level. Li et al.11) studied a prospective and randomized clinical trial compared the clinical outcomes between the Zero-P and CCP devices. The Zero-P spacer was superior to the CCP device in reducing the post-operative speed of degeneration. The authors also analyzed post-operative dysphagia using the dysphagia score2) at 1, 3, 6, and 12 months after surgery. Dysphagia scores were low in the Zero-P group at every follow-up. However, no statistically differences were evident between the groups at 12 months follow-up, while 4 patients still suffered from mild dysphagia in the CCP group. Barbagallo et al.1) prospectively analyzed a series of patients treated with single- or multi-level ACDF with the Zero-P spacer for up to 4 years after surgery. They concluded that the Zero-P spacer was judged safe and efficient, even in multilevel ACDF as focused on radiological outcomes, complications, and technical hints.
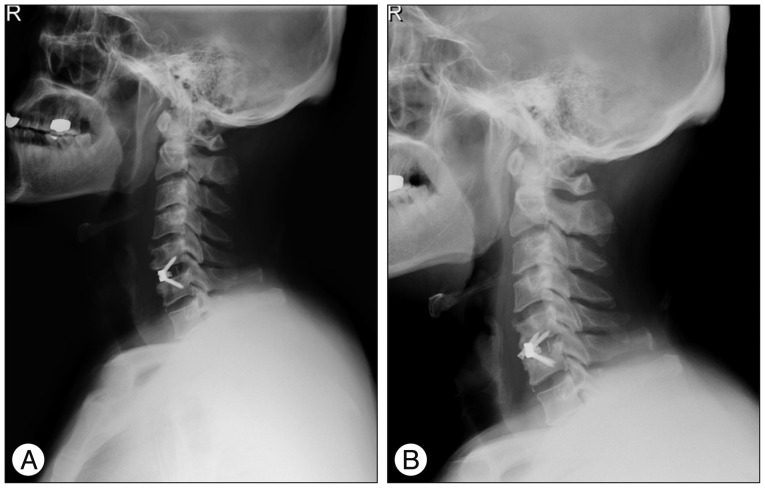
Presently, there was a complication with screw loosening in a Zero-P spacer used in. 51-year-old patient who suffered from typical symptoms of cervical intervertebral disc herniation including neck pain and radiating pain. ACDF was at the C5-6 level with the Zero-P spacer. After the operation, he recovered appropriately without any complications. However, he complained of radiating pain on left C6 dermatome 1 month after the operation. Radiologic findings revealed loosening and nonunion of the left upper screw from the vertebral body (Fig. 3). Insufficient screw length and low screw instrumentation angle were thought to be the reasons. We had prepared for the second operation to correct the loosen screws. However, the patient refused additional management and was lost from follow-up. To the best our knowledge, no other such case has been reported. More studies would be need-ed for confirming the suggested reasons of non-union.
This study has several limitations. More patients and longer follow-up are required to confirm our hypothesis. Analysis of two or more operation levels would be helpful for understanding the advantages of this instrument. Despite these limitations, the study demonstrates the efficacy and satisfactory clinical outcomes of the Zero-P spacer. As another limtation, prevertebral structures are different between the upper cervical and lower cervical vertebrae. At the upper cervical level, only the posterior wall of the hypopharynx comprise the prevertebral structures. On the contrary, more complex structures as transverse arytenoid muscle, larynx, trachea and esophagus are components of the prevertebral structures at the lower cervical level. Thus, the calculated subtractions may be influenced by these differences. More detailed analysis of the relationship between the components of each operative level and soft tissue swelling is necessary for the definitive conclusions. Finally, although there was a statistically difference of EBL between the two groups, we consider that its standard deviation was too large to conclude significance. This result might be due to different anesthesiologist's records of EBL.
ACDF is a verified procedure in the treatment of cervical disc disease. In this study, both Zero-P and CCP devices were effective for single level ACDF, and application of the Zero-P spacer resulted in minimal prevertebral soft tissue swelling and decreased post-operative dysphagia 6 months after the operation. Additional long-term follow-up, larger scale, prospective, randomized controlled studies may be helpful for determining this conclusion.
Acknowledgements
This study was supported by Research institute for Convergence of biomedical science and technology (30-2012-009), Pusan National University Yangsan Hospital.
References
1. Barbagallo GM, Romano D, Certo F, Milone P, Albanese V. Zero-P : a new zero-profile cage-plate device for single and multilevel ACDF. A single institution series with four years maximum follow-up and review of the literature on zero-profile devices. Eur Spine J. 2013; 22(Suppl 6):S868–S878. PMID: 24061968.
2. Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery : a prospective study. Spine (Phila Pa 1976). 2002; 27:2453–2458. PMID: 12435974.
4. Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958; 15:602–617. PMID: 13599052.

5. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007; 32:2310–2317. PMID: 17906571.

6. Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976). 1988; 13:870–876. PMID: 3143157.

7. Kalb S, Reis MT, Cowperthwaite MC, Fox DJ, Lefevre R, Theodore N, et al. Dysphagia after anterior cervical spine surgery : incidence and risk factors. World Neurosurg. 2012; 77:183–187. PMID: 22155226.

8. Kim SW, Limson MA, Kim SB, Arbatin JJ, Chang KY, Park MS, et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J. 2009; 18:218–231. PMID: 19127374.

9. Korinth MC. Treatment of cervical degenerative disc disease - current status and trends. Zentralbl Neurochir. 2008; 69:113–124. PMID: 18666050.

10. Lee MJ, Bazaz R, Furey CG, Yoo J. Influence of anterior cervical plate design on Dysphagia : a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech. 2005; 18:406–409. PMID: 16189451.
11. Li Y, Hao D, He B, Wang X, Yan L. The efficiency of zero-profile implant in anterior cervical discectomy fusion : a prospective controlled long-term follow-up study. J Spinal Disord Tech. 2013; [Epub ahead of print].
12. Mummaneni PV, Kaiser MG, Matz PG, Anderson PA, Groff MW, Heary RF, et al. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine. 2009; 11:130–141. PMID: 19769492.

13. Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am. 2005; 87:558–563. PMID: 15741622.

14. Pitzen TR, Chrobok J, Stulik J, Ruffing S, Drumm J, Sova L, et al. Implant complications, fusion, loss of lordosis, and outcome after anterior cervical plating with dynamic or rigid plates : two-year results of a multi-centric, randomized, controlled study. Spine (Phila Pa 1976). 2009; 34:641–646. PMID: 19287352.

15. Scholz M, Schnake KJ, Pingel A, Hoffmann R, Kandziora F. A new zero-profile implant for stand-alone anterior cervical interbody fusion. Clin Orthop Relat Res. 2011; 469:666–673. PMID: 20882376.

16. Song KJ, Choi BW, Kim HY, Jeon TS, Chang H. Efficacy of postoperative radiograph for evaluating the prevertebral soft tissue swelling after anterior cervical discectomy and fusion. Clin Orthop Surg. 2012; 4:77–82. PMID: 22379559.

17. Wang ZD, Zhu RF, Yang HL, Gan MF, Zhang SK, Shen MJ, et al. The application of a zero-profile implant in anterior cervical discectomy and fusion. J Clin Neurosci. 2014; 21:462–466. PMID: 24262773.

18. Zhong ZM, Jiang JM, Qu DB, Wang J, Li XP, Lu KW, et al. Esophageal perforation related to anterior cervical spinal surgery. J Clin Neurosci. 2013; 20:1402–1405. PMID: 23891121.

Fig. 1
A : Schematic images of the Zero-P showing that interbody fusion is reinforced within two cranial and caudal locking screws and polyetheretherketone (PEEK) cage. B : The Zero-P spacer is visualized in plain films of antero-posterior and lateral view after successful operation.
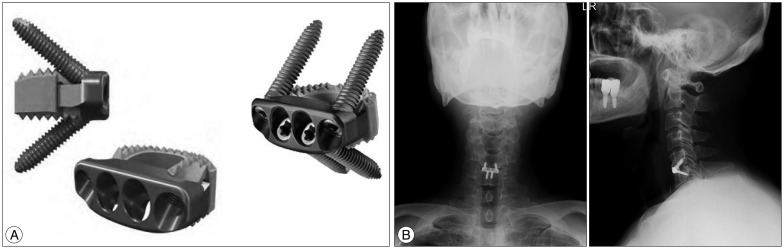
Fig. 2
Prevertebral soft tissue thickness was calculated as mean value of the distance between the anterior surface of each vertebral body (Zero-P) or plate (CCP) and the air shadow of the airway. A : CCP group. B : Zero-P group. *Thickness=(A+B)/2.
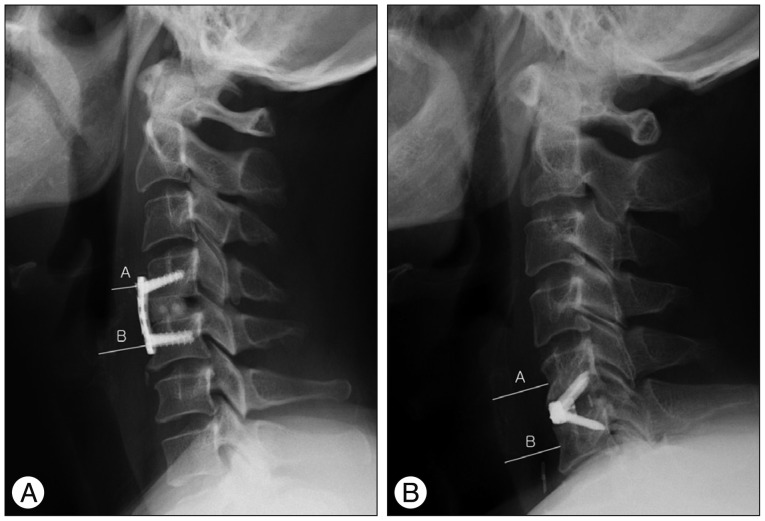
Fig. 3
Plain films demonstrated the loosening and nonunion of screws to the vertebral body. A : On the day of the operation. B : One-month post-operatively.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download