This article has been
cited by other articles in ScienceCentral.
Abstract
Vascular complications after percutaneous angiography include hematoma, pseudoaneurysm, arteriovenous fistula, thromboembolism, arterial laceration and infection. Hematomas may occur in the groin, thigh, retroperitoneal, intraperitoneal, or abdominal wall. A 54-year-old female underwent percutaneous transfemoral angiography for the evaluation of cerebral aneurysm. Renal subcapsular hematoma developed 3 hours after the procedure. Renal subcapsular hematoma after percutaneous angiography is very rare. We investigated the possible causes of renal subcapsular hematoma. To avoid this rare complication, we need to perform guide-wire passage carefully from the beginning of the procedure under full visual monitoring.
Go to :

Keywords: Renal artery, Anatomy, Catheterization, Vascular injuries
INTRODUCTION
Vascular problems after percutaneous angiography are major and serious complications. Vascular complications include hematoma, pseudoaneurysm, arteriovenous (AV) fistula, thromboembolism, arterial laceration and infection
3,
4,
9). It is important to know the risk of complications and how to avoid possible causes that may cause such problems. We experienced an unusual renal subcapsular hematoma after percutaneous angiography. We investigated the possible causes of renal subcapsular hematoma. The presence of an accessory renal artery is not uncommon variation, and this could function as the cause of unusual renal subcapsular hematoma.
Go to :

CASE REPORT
A 54-year-old female was admitted to our hospital for the evaluation of unruptured cerebral aneurysm. She had a 5-year history of diabetes mellitus and hypertension. Eighteen months earlier, she had chest pain and underwent transfemoral cardiac angiogram at a different institute. Since then, she had been taking aspirin 100 mg under the diagnosis of angina. Percutaneous cerebral angiogram was performed through the right femoral artery. She was diagnosed as having multiple aneurysms in both the anterior communicating artery and in the paraclinoid portion of the internal carotid artery. The whole procedure of percutaneous cerebral angiogram was uneventful. However, about 3 hours later, she complained of left flank pain. Her blood pressure was 90/60 mm Hg and the body temperature was 36.4℃. On physical examination, the abdomen was soft but tender on the left upper quadrant. There was no evidence of puncture site bleeding or petechiae. Laboratory findings were white blood cell 6100/mm
3, Hb 10.8 g/dL, platelets 174000/mm
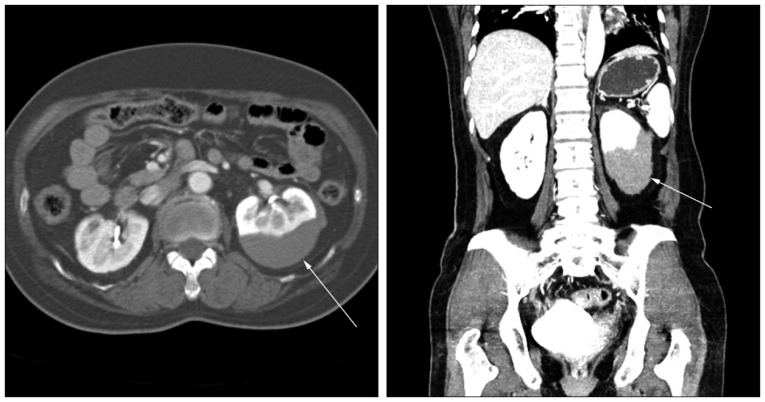
3. We performed abdominal computed tomography (CT). Abdominal CT showed a left renal subcapsular hematoma in the lower pole portion (
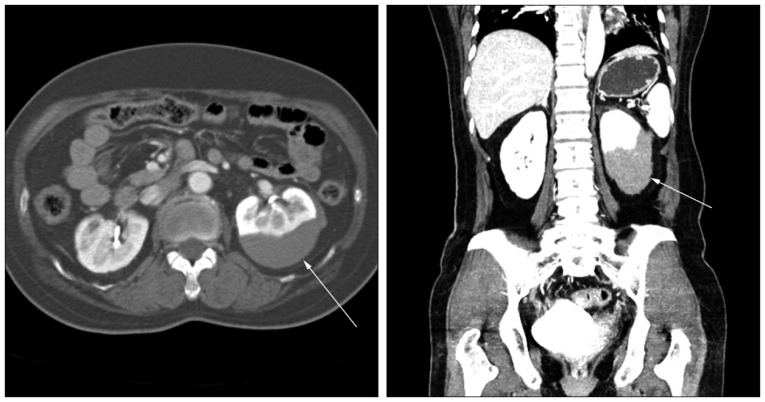
Fig. 1). She was consulted by Urology Department and was advised to undergo supportive treatment. She had a followed-up abdominal CT seven days later. The follow-up abdominal CT showed a slight regression of the hematoma. She was discharged with improved conditions after 14 days of hospital stay. Six months later, her 64-cut multislice CT scan showed complete regression of the subcapsular hematoma (
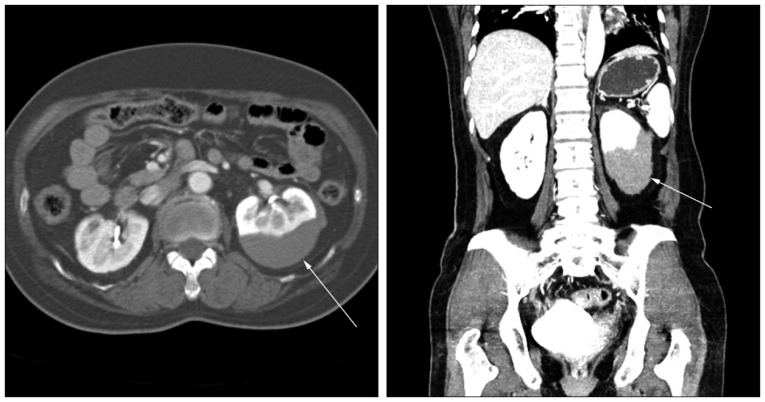
Fig. 2). Interestingly, in her three-dimensional angiogram, small accessory renal arteries supplying the lower pole of the kidney were found at both sides (
Fig. 3). She has remained symptom free since then.
 | Fig. 1Post enhanced abdominal computed tomography (axial and coronal) image shows the left kidney being compressed by the subcapsular hematoma (arrows). 
|
 | Fig. 2Post-enhanced abdominal computed tomography (axial and coronal) after 8 months shows a complete resolution of the hematoma. 
|
 | Fig. 364 Multidetector computed tomography three dimension angiogram shows bilateral accessory arteries (arrows) supplying the lower pole of the kidney. Right side accessory renal artery is located more distal than left. 
|
Go to :

DISCUSSION
Diagnostic cardiac angiography with transfemoral catheterization has 1-2% risk of major complications
5). Vascular complications contribute to about 0.3-1% of all major complications
5,
9). Hematomas are usually located in the femoral puncture site, retroperitoneal space, intraperitoneal region, and abdominal wall
3,
4). Risk factors for cardiac catheterization hematoma formation are age older than 60 years, female, angioplasty instead of angiography alone, hypertension, thrombocytopenia, large-bore catheter size, operator inexperience, poor groin compression after sheath removal, high puncture site, peripheral vascular disease, and anticoagulant-thrombolytic therapy
3,
4,
9).
Renal subcapsular hematomas could happen spontaneously or iatrogenically. Neoplasm, bleeding tendency, vasculitis and infection are the causes of spontaneous bleeding. Regarding iatrogenic causes, renal biopsy, extracorporeal lithotripsy, and anticoagulants are some sources. The incidence of iatrogenic renal artery injury during the percutaneous transluminal angioplasty is about 6.5-22.8%
1,
3). The most common cause is guide-wire perforation. Stable wire position and J-shaped guide-wire could avoid these vascular injury
1). There has been only one paper in English describing renal subcapsular hematoma after femoral artery catheterization
3). In that study, they reported that calcified plaques in the aorto-renal junction may get dislodged during catheter or wire passage. After dislodging of plaques, renal subcapsular hematoma could form through the dissected vessel
3).
Typically, renal arteries branches at the level of the upper margin of the second lumbar vertebral body, 1 cm below the origin of the superior mesenteric artery
6,
7). One or two accessory renal arteries are found in about 23%, especially on the left side
6,
7,
8). Accessory renal arteries usually arise from the aorta
7). Bilateral multiple renal arteries are found in 10% of the population
7,
10). In our case, both accessory renal arteries were found on the follow up CT angiogram (
Fig. 3). Multidetector computed tomography is a very useful tool in most cases for the visualization of abdominal organs and vascular structures
2,
10). Left accessory renal artery branches at the level of the lower margin of the third lumbar vertebral body and supplies the lower pole of the kidney. We reviewed our patient's medical record thoroughly. We used the introducing wire that was straight shape and 45 cm long (Radifocus introducer II, Terumo Co., Tokyo, Japan) for sheath placement. In small height person, relatively short distance from puncture site to opening of accessory renal artery could be possible. We used the 150-cm-long, 0.035-inch nitinol hydrophilic guide-wire with 45-degree angled, 3.0-cm soft tip (Radifocus guide wire M, Terumo Co., Tokyo, Japan). The possibility of injury in the proximal portion of the left accessory renal artery during the wire insertion for sheath placement or the guide-wire passage around the level of the lower lumbar vertebral body was considered. The right femoral approach is the most commonly used access site for percutaneous angiography. In the case of the right side femoral approach, the left side accessory renal artery supplying the lower pole is prone to accidental damage. This insult may lead to subcapsular hematoma around the lower pole of the kidney. Usually the right side accessory renal artery is located more distal than left and should be careful in case of left femoral puncture (
Fig. 3). The previous report also involved a case of left lower pole subcapsular renal hematoma. Furthermore, we were able to detect calcified plaques which might be located in the accessory renal artery supplying the lower pole of the kidney
3).
Go to :

CONCLUSION
Accessory renal arteries are not rare and easy to be injured at the level of the lower lumbar vertebral body. Careful guide-wire passage under full visual inspection is important to avoid inadvertent vascular injury during percutaneous angiography.
Go to :