1. Allen R. Dopamine and iron in the pathophysiology of restless legs syndrome (RLS). Sleep Med. 2004; 5:385–391. PMID:
15222997.

2. Allen R, Chen C, Soaita A, Wohlberg C, Knapp L, Peterson BT, et al. A randomized, double-blind, 6-week, dose-ranging study of pregabalin in patients with restless legs syndrome. Sleep Med. 2010; 11:512–519. PMID:
20466589.

3. Allen RP, Barker PB, Wehrl F, Song HK, Earley CJ. MRI measurement of brain iron in patients with restless legs syndrome. Neurology. 2001; 56:263–265. PMID:
11160969.

4. Allen RP, Earley CJ. Augmentation of the restless legs syndrome with carbidopa/levodopa. Sleep. 1996; 19:205–213. PMID:
8723377.

5. Allen RP, Earley CJ. Restless legs syndrome : a review of clinical and pathophysiologic features. J Clin Neurophysiol. 2001; 18:128–147. PMID:
11435804.
6. Allen RP, Kushida CA, Atkinson MJ. RLS QoL Consortium. Factor analysis of the International Restless Legs Syndrome Study Group's scale for restless legs severity. Sleep Med. 2003; 4:133–135. PMID:
14592343.

7. Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisi J, et al. Restless legs syndrome : diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003; 4:101–119. PMID:
14592341.

8. Bassetti CL, Mauerhofer D, Gugger M, Mathis J, Hess CW. Restless legs syndrome : a clinical study of 55 patients. Eur Neurol. 2001; 45:67–74. PMID:
11244268.

9. Beattie PF, Meyers SP, Stratford P, Millard RW, Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine (Phila Pa 1976). 2000; 25:819–828. PMID:
10751293.

10. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990; 72:403–408. PMID:
2312537.

11. Budhiraja P, Budhiraja R, Goodwin JL, Allen RP, Newman AB, Koo BB, et al. Incidence of restless legs syndrome and its correlates. J Clin Sleep Med. 2012; 8:119–124. PMID:
22505854.

12. Chesson AL Jr, Wise M, Davila D, Johnson S, Littner M, Anderson WM, et al. Standards of Practice Committee of the American Academy of Sleep Medicine. Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder. An American Academy of Sleep Medicine Report. Sleep. 1999; 22:961–968. PMID:
10566915.

13. Cho YW, Shin WC, Yun CH, Hong SB, Kim JH, Allen RP, et al. Epidemiology of restless legs syndrome in Korean adults. Sleep. 2008; 31:219–223. PMID:
18274269.

14. Cirillo DJ, Wallace RB. Restless legs syndrome and functional limitations among American elders in the Health and Retirement Study. BMC Geriatr. 2012; 12:39. PMID:
22834914.

15. Civi S, Kutlu R, Tokgoz S. Frequency, severity and risk factors for restless legs syndrome in healthcare personnel. Neurosciences (Riyadh). 2012; 17:230–235. PMID:
22772928.
16. Comella CL. Restless legs syndrome : treatment with dopaminergic agents. Neurology. 2002; 58(4 suppl 1):s87–s92. PMID:
11909990.
17. Ekbom KA. Restless legs : a clinical study. Acta Med Scand. 1945; 158(suppl):1–123.
18. Erikson KM, Jones BC, Beard JL. Iron deficiency alters dopamine transporter functioning in rat striatum. J Nutr. 2000; 130:2831–2837. PMID:
11053528.

19. Erikson KM, Jones BC, Hess EJ, Zhang Q, Beard JL. Iron deficiency decreases dopamine D1 and D2 receptors in rat brain. Pharmacol Biochem Behav. 2001; 69:409–418. PMID:
11509198.

20. Gupta R, Lahan V, Goel D. Restless Legs Syndrome : a common disorder, but rarely diagnosed and barely treated--an Indian experience. Sleep Med. 2012; 13:838–841. PMID:
22704403.

21. Hemmer B, Riemann D, Glocker FX, Lücking CH, Deuschl G. Restless legs syndrome after a borrelia-induced myelitis. Mov Disord. 1995; 10:521–522. PMID:
7565839.

22. Högl B, Frauscher B, Seppi K, Ulmer H, Poewe W. Transient restless legs syndrome after spinal anesthesia : a prospective study. Neurology. 2002; 59:1705–1707. PMID:
12473756.

23. Hoque R, Chesson AL Jr. Pharmacologically induced/exacerbated restless legs syndrome, periodic limb movements of sleep, and REM behavior disorder/REM sleep without atonia : literature review, qualitative scoring, and comparative analysis. J Clin Sleep Med. 2010; 6:79–83. PMID:
20191944.
24. Inoue Y, Hirata K, Uchimura N, Kuroda K, Hattori N, Takeuchi M. Gabapentin enacarbil in Japanese patients with restless legs syndrome : a 12-week, randomized, double-blind, placebo-controlled, parallel-group study. Curr Med Res Opin. 2013; 29:13–21. PMID:
23121149.

25. Karppinen J, Malmivaara A, Tervonen O, Pääkkö E, Kurunlahti M, Syrjälä P, et al. Severity of symptoms and signs in relation to magnetic resonance imaging findings among sciatic patients. Spine (Phila Pa 1976). 2001; 26:E149–E154. PMID:
11295915.

26. Kim KW, Jhoo JH, Lee SB, Lee SD, Kim TH, Kim SE, et al. Increased striatal dopamine transporter density in moderately severe old restless legs syndrome patients. Eur J Neurol. 2012; 19:1213–1218. PMID:
22435397.

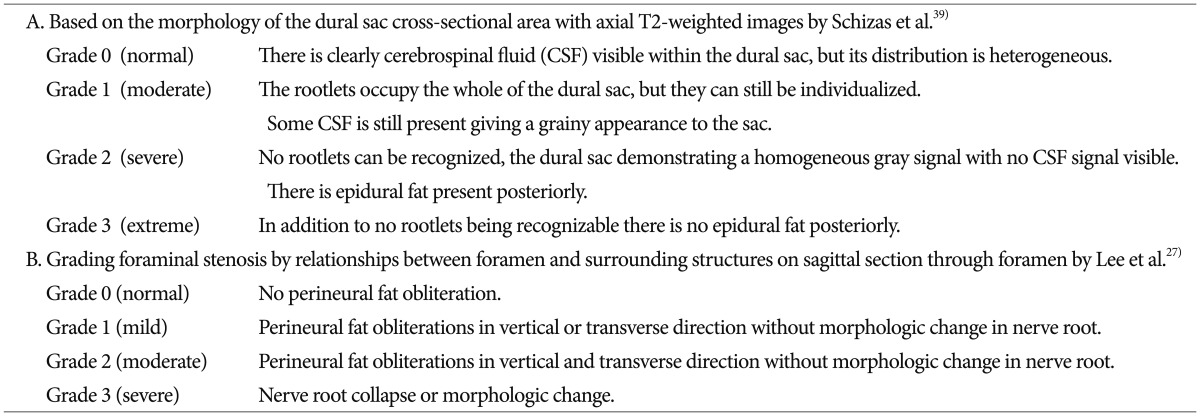
27. Lee S, Lee JW, Yeom JS, Kim KJ, Kim HJ, Chung SK, et al. A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol. 2010; 194:1095–1098. PMID:
20308517.

28. Manconi M, Ferri R, Zucconi M, Oldani A, Giarolli L, Bottasini V, et al. Pramipexole versus ropinirole : polysomnographic acute effects in restless legs syndrome. Mov Disord. 2011; 26:892–895. PMID:
21370262.

29. Michaud M, Chabli A, Lavigne G, Montplaisir J. Arm restlessness in patients with restless legs syndrome. Mov Disord. 2000; 15:289–293. PMID:
10752578.

30. Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lespérance P. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome : a study of 133 patients diagnosed with new standard criteria. Mov Disord. 1997; 12:61–65. PMID:
8990055.

31. Montplaisir J, Karrasch J, Haan J, Volc D. Ropinirole is effective in the long-term management of restless legs syndrome : a randomized controlled trial. Mov Disord. 2006; 21:1627–1635. PMID:
16874755.

32. Mosko SS, Dickel MJ, Ashurst J. Night-to-night variability in sleep apnea and sleep-related periodic leg movements in the elderly. Sleep. 1988; 11:340–348. PMID:
3206054.
33. Ohayon MM, O'Hara R, Vitiello MV. Epidemiology of restless legs syndrome : a synthesis of the literature. Sleep Med Rev. 2012; 16:283–295. PMID:
21795081.
34. Ondo W, Romanyshyn J, Vuong KD, Lai D. Long-term treatment of restless legs syndrome with dopamine agonists. Arch Neurol. 2004; 61:1393–1397. PMID:
15364685.

35. Panda S, Taly AB, Sinha S, Gururaj G, Girish N, Nagaraja D. Sleep-related disorders among a healthy population in South India. Neurol India. 2012; 60:68–74. PMID:
22406784.

36. Peeraully T, Tan EK. Linking restless legs syndrome with Parkinson's disease : clinical, imaging and genetic evidence. Transl Neurodegener. 2012; 1:6. PMID:
23211049.
37. Phillips B, Young T, Finn L, Asher K, Hening WA, Purvis C. Epidemiology of restless legs symptoms in adults. Arch Intern Med. 2000; 160:2137–2141. PMID:
10904456.

38. Rizzo G, Tonon C, Testa C, Manners D, Vetrugno R, Pizza F, et al. Abnormal medial thalamic metabolism in patients with idiopathic restless legs syndrome. Brain. 2012; 135(Pt 12):3712–3720. PMID:
23183234.

39. Schizas C, Theumann N, Burn A, Tansey R, Wardlaw D, Smith FW, et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976). 2010; 35:1919–1924. PMID:
20671589.

40. Scholz H, Trenkwalder C, Kohnen R, Riemann D, Kriston L, Hornyak M. Dopamine agonists for restless legs syndrome. Cochrane Database Syst Rev. 2011; (3):CD006009. PMID:
21412893.
41. Scott LJ. Gabapentin enacarbil : in patients with restless legs syndrome. CNS Drugs. 2012; 26:1073–1083. PMID:
23179641.
42. Tan EK. Restless legs syndrome and Parkinson's disease : is there an etiologic link? J Neurol. 2006; 253(Suppl 7):VII33–VII37. PMID:
17131226.
43. Tan EK, Seah A, See SJ, Lim E, Wong MC, Koh KK. Restless legs syndrome in an Asian population : a study in Singapore. Mov Disord. 2001; 16:577–579. PMID:
11391765.
44. Trenkwalder C, Paulus W. Restless legs syndrome : pathophysiology, clinical presentation and management. Nat Rev Neurol. 2010; 6:337–346. PMID:
20531433.

45. Unrath A, Juengling FD, Schork M, Kassubek J. Cortical grey matter alterations in idiopathic restless legs syndrome : an optimized voxel-based morphometry study. Mov Disord. 2007; 22:1751–1756. PMID:
17566123.

46. Weber M, Lauterburg T, Tobler I, Burgunder JM. Circadian patterns of neurotransmitter related gene expression in motor regions of the rat brain. Neurosci Lett. 2004; 358:17–20. PMID:
15016424.

47. Weimerskirch PR, Ernst ME. Newer dopamine agonists in the treatment of restless legs syndrome. Ann Pharmacother. 2001; 35:627–630. PMID:
11346069.

48. Wetter TC, Eisensehr I, Trenkwalder C. Functional neuroimaging studies in restless legs syndrome. Sleep Med. 2004; 5:401–406. PMID:
15223000.

49. Winkelman JW, Johnston L. Augmentation and tolerance with long-term pramipexole treatment of restless legs syndrome (RLS). Sleep Med. 2004; 5:9–14. PMID:
14725821.

50. Winkelmann J, Schadrack J, Wetter TC, Zieglgänsberger W, Trenkwalder C. Opioid and dopamine antagonist drug challenges in untreated restless legs syndrome patients. Sleep Med. 2001; 2:57–61. PMID:
11152983.

51. Zwartbol RT, Jellema K, Boiten J, Rijsman R. Acute exacerbation of restless legs due to cervical spinal cord ischaemia. BMJ Case Rep. 2013; 2013.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download