Abstract
Hydranencephaly is a rare congenital disease defined as an absence of cerebral hemispheres with an intact thalamus, brain stem, and cerebellum. Generally, patients with hydranencephaly require cerebro-spinal fluid diversion due to progressive hydrocephalus. An excellent view of the choroid plexus and advancement of the neurosurgical endoscope were possible, leading to easy coagulation of the choroid plexus to balance cerebro-spinal fluid production without the use of a shunt device. We present this rare case and good treatment outcome from endoscopic coagulation of the choroid plexus.
Hydranencephaly is known as an absence of cerebral hemispheres, with the associated space filled with cerebro-spinal fluid (CSF), and an intact skull and meninges10). Though cerebral hemispheres are not present completely, the cerebellum, thalami, choroid plexus, and brain stem are generally preserved. In some cases, occipital lobes also remain intact. The exact cause of the disease is undetermined, but vascular occlusion, intrauterine infection, and traumatic disorder after the first trimester of pregnancy are suggested. The prognosis of patients is very poor due to various complications3).
Because of continuous CSF production by the choroid plexus and poor absorption of CSF, many patients suffer from increasing head size and intracranial pressure. The standard treatment for excess CSF is a diversion, usually preformed by ventriculoperitoneal shunt (VPS). However, VPS is associated with many complications such as infection, disconnection, malfunction, skin breakdown over the shunt system, over drainage, and CSF leakage14).
The coagulation and removal of the choroid plexus in the lateral ventricle as a treatment for hydrocephalus was first reported by Dandy in 19182). However, this procedure has disappeared due to its low success rate and high rate of complications. Recently, because of the excellent view of the choroid plexus in hydranencephaly and the advancement of the neurosurgical endoscope, choroid plexus coagulation has again received attention in the treatment of hydranencephaly. Many studies with high success rates have been published regarding endoscopic coagulation of the choroid plexus to treat hydrocephalus in hydranencephaly5,7,13). We present a case of hydranencephaly treated with endoscopic coagulation of the choroid plexus.
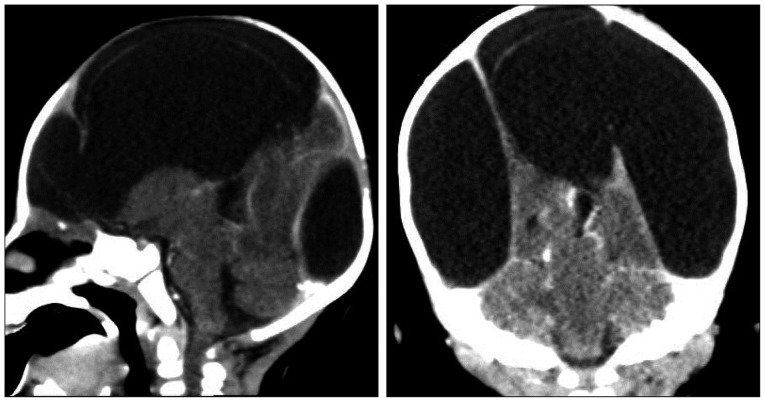
The patient was diagnosed with hydranencephaly by maternal ultrasound in the prenatal period and was born at full term in our hospital. The patient was female, weighed 3500 g, and was 52 cm in height. Chromosomal study was normal and no other anomalies except hydranencephaly were found on physical examination and imaging studies. At birth, the patient's head circumference was 32 cm and the fontanel was soft and flat; however, the head circumference increased progressively and the fontanel became tenser day by day. A computed tomographic (CT) scan revealed hydranencephaly with loss of cerebral hemispheres except a small portion of the occipital lobe, normal shape of thalamus, and intact brain stem and cerebellum (Fig. 1). The choroid plexus was clearly revealed between both thalami on contrast CT scan. Most of the intracranial space was filled with low density fluid thought to be CSF, and the space was separated by a thin membrane. Magnetic resonance imaging (MRI) showed similar findings to the CT scan. The vertebro-basilar artery and posterior cerebral arteries had a normal-sized signal void except for faint anterior and middle cerebral arteries.
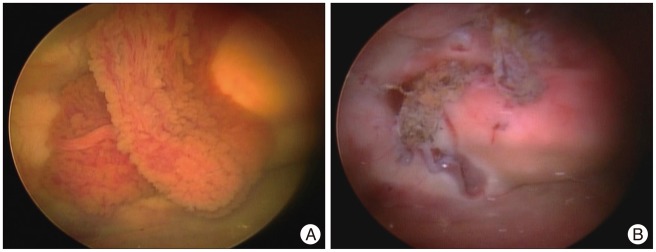
We performed endoscopic coagulation of the choroid plexus 2 weeks after birth due to clinical symptoms of intracranial hypertension such as poor oral intake and irritability. Under general and endotracheal anesthesia, the patient was placed in the supine position with the head rotated to the right side. We made a semicircular skin incision and the periosteum was carefully dissected away to reveal the left parietal bone. A standard small craniotomy was performed beside the coronal and sagittal suture with a high-speed drill. After a semicircular incision in the dura matter, we introduced a rigid endoscope into the intracranial space filled with CSF. There were intact thalami, a small portion of occipital lobe and two choroid plexus-like masses between the thalami. We identified that the choroid plexus originated from the third ventricle between the thalami. The whole visible choroid plexus was coagulated using monopolar and bipolar electrocautery through a working channel in the endoscope (Fig. 2). No attempt was made to coagulate the origin of the choroid plexus by force in the third ventricle because of the risk of thalamus damage. After we confirmed the stoppage of bleeding of the choroid plexus, the endoscope was withdrawn. The dura was closed in a watertight fashion and the bone flap was placed on it. The scalp was sutured layer-by-layer.
Postoperatively, the fontanel was sunken, and the patient recovered. CSF leakage was not observed prior to discharge from the hospital. After 6 months, the fontanel of patient remained soft and her head circumference was 35 centimeters, which was within the 65 percentile of the head growth curve. The patient had no evidence of intracranial hypertension. The choroid plexus was not visible on CT scan with enhancement (Fig. 3). A fluid collection under the operation site and skin breakdown was not found.
Hydranencephaly is a rare malformation of the central nervous system, which is described as an absence of the cerebral hemispheres. Typically the cranium, meninges, and brain stem are preserved, however. Hydranencephaly with thin cortical nerve tissue is referred to as near hydranencephaly. The space the cerebral hemispheres usually occupy is filled with CSF. The choroid plexus usually originates from the third ventricle between the thalami and is exposed in the CSF space. The cause of this disease remains unclear, but is hypothesized to result from bilateral carotid occlusion in utero, infections, and genetic factors4,11). The patients have visual disturbance, lack of growth, deafness, spastic quadriparesis, marked intellectual deficit, and progressive macrocephaly. The life expectancy of patients is around 2 years and they die due to various complications3). Hydrocephalus is also a common problem and treatment is needed because of progressive growth of the head circumference and increased intracranial pressure. Though the typical treatment for hydrocephalus is CSF diversion using a ventriculoperitoneal shunt, it has many complications.
In 1918, Dandy2) reported an open technique for destruction of the choroid plexus (choroid plexectomy) as a treatment for hydrocephalus to control CSF production. However, this operation had a low success rate and a high mortality rate. In later studies reporting the use of choroid plexectomy to treat hydrocephalus, only 55% of the patients who underwent choroid plexectomy had good outcomes; thus, choroid plexectomy never became a preferred treatment for hydrocephalus9). However, due to advancements in the use of neurosurgical endoscope, endoscopic coagulation of the choroid plexus has been revisited as a treatment for hydrocephalus. Warf12) published an excellent success rate for endoscopic choroid plexus coagulation with third ventriculostomy as primary treatment for hydrocephalus in 2005.
There have been four reports published about choroid plexectomy or endoscopic choroid plexus coagulation for the treatment of hydranencephaly or near hydranencephaly with minimal cortical mantle. Albright1) reported 3 patients who underwent percutaneous choroid plexus coagulation in 1981. Two patients had controlled CSF production after the procedure; however, the other patient required CSF diversion due to the presence of a minimal amount of choroid plexus and coagulation. In 2002, Wellons et al.13) published results of a direct comparison of a shunt procedure with choroid plexectomy in hydranencephaly or near hydranencephaly. No revision, readmission, or complications were found in 4 patients of whom underwent choroid plexectomy were achieved. However, 2 revisions, 4.35 days of readmission, and 7 complications occurred in the 9 patients who underwent a shunt procedure. Malheiros et al.5) reported the first prospective and randomized study of endoscopic choroid plexus coagulation and VPS in 2010. Eight of 10 patients who were underwent endoscopic choroid plexus coagulation had successfully controlled CSF production, but 2 patients needed VPS due to failed CSF control. Seven patients underwent randomized VPS and 2 patients among them required shunt revisions during the follow-up period. There was no difference in success rate between the endoscopic choroid plexus coagulation group and the VPS group, and endoscopic choroid plexus coagulation was more economical than VPS. In 2012, Sandburget al.7) retrospectively studied endoscopic choroid plexus coagulation for hydranencephaly and near hydranencephaly. Eight patients underwent endoscopic choroid plexus coagulation, but 4 patients required a shunt procedure after endoscopic surgery. Except failure to control hydrocephalus in 4 patients, there were no additional complications noted after endoscopic surgeries. In all previous studies, endoscopic coagulation of the choroid plexus was a viable treatment modality to avoid the morbidities associated with VPS in hydranencephaly.
VPS is the traditional CSF diversion treatment for hydrocephalus. However, it has many complications, such as infection, CSF leakage, disconnection, shunt malfunction, over-drainage, and skin breakdown over the shunt device. Especially in hyranencephalic patients, CSF leakage and CSF collection along the shunt device arise more frequently due to loss of cortical sealing, which can occur in an absent or thin cortical hemisphere. Also, skin breakdown due to the scalp thinning associated with increasing head size may occur. Therefore, endoscopic coagulation of choroid plexus has good indications for avoiding complications of VPS in hydranencephaly. Patients with hydranencephaly have an intracranial space filled with clear CSF, which allows for excellent view of the bilateral choroid plexus; thus, endoscopic approach to the choroid plexus is easy compared with pure hydrocephalus. Endoscopic coagulation of the choroid plexus is an acceptable treatment for control of CSF production in hydranencephaly.
There were no reports addressing the extent of coagulation of the choroid plexus. The coagulation of all visible choroid plexus within endoscopic view may make good outcomes and the problem with associated that is not reported yet. Because CSF production is performed by not only the choroid plexus, but also the brain ependyma, in cases of hydranencephaly with minimal brain parenchyma, CSF production is well controlled by only coagulation of the visible choroid plexus6,8). In the present case, we identified a massive amount of choroid plexus with enhanced CT scan preoperatively, and the outcomes of coagulation of all visible choroid plexus were very good.
The endoscopic coagulation of the choroid plexus is the preferable treatment for hydrocephalus without foreign body insertion, such as a shunt device. In particular, in cases of hydranencephaly with an excellent view of the choroid plexus, the procedure had good indications for avoiding the complications associated with VPS. Because hydranencephaly is very rare and the follow-up period is typically short due to disease characteristics, a large number of patients and long-term follow-up are needed to determine the effectiveness of this procedure.
References
1. Albright L. Percutaneous choroid plexus coagulation in hydranencephaly. Childs Brain. 1981; 8:134–137. PMID: 7249814.

2. Dandy WE. Extripation of the choroid plexus of the lateral ventricle in communicating hydrocephalus. Ann Surg. 1918; 68:569–579. PMID: 17864025.

3. Hunziker K. Uber einen Fall von Hydranenzephalie. Mschr Psychiat Neurol. 1947; 114:129.
4. Kang SK, Chang SK, Kang JK, Song JU. Two cases of infantile hydranencephaly. J Korean Neurosurg Soc. 1980; 9:601–608.
5. Malheiros JA, Trivelato FP, Oliveira MM, Gusmão S, Cochrane DD, Steinbok P. Endoscopic choroid plexus cauterization versus ventriculoperitoneal shunt for hydranencephaly and near hydranencephaly : a prospective study. Neurosurgery. 2010; 66:459–464. discussion 464. PMID: 20173541.

6. Milhorat TH, Hammock MK, Chien T, Davis DA. Normal rate of cerebrospinal fluid formation five years after bilateral choroid plexectomy. Case report. J Neurosurg. 1976; 44:735–739. PMID: 1083897.

7. Sandberg DI, Chamiraju P, Zoeller G, Bhatia S, Ragheb J. Endoscopic choroid plexus coagulation in infants with hydranencephaly or hydrocephalus with a minimal cortical mantle. Pediatr Neurosurg. 2012; 48:6–12. PMID: 22832209.

8. Sato O, Bering EA. Extra-ventricular formation of cerebrospinal fluid. No To Shinkei. 1967; 19:883–885. PMID: 5630703.
9. Scarff JE. Evaluation of treatment of hydrocephalus. Results of third ventriculostomy and endoscopic cauterization of choroid plexuses compared with mechanical shunts. Arch Neurol. 1966; 14:382–391. PMID: 5906463.
10. Sutton LN, Bruce DA, Schut L. Hydranencephaly versus maximal hydrocephalus : an important clinical distinction. Neurosurgery. 1980; 6:34–38. PMID: 7354898.
11. Urich H. Malformations of the nervous system, perinatal damage and related conditions in early life. In : Blackwood W, Corsellis JAN, editors. Greenfield's Neuropathology. Chicago: Year Book Medical;1976. p. 394–395.
12. Warf BC. Comparison of endoscopic third ventriculostomy alone and combined with choroid plexus cauterization in infants younger than 1 year of age : a prospective study in 550 African children. J Neurosurg. 2005; 103(6 Suppl):475–481. PMID: 16383244.

13. Wellons JC 3rd, Tubbs RS, Leveque JC, Blount JP, Oakes WJ. Choroid plexectomy reduces neurosurgical intervention in patients with hydranencephaly. Pediatr Neurosurg. 2002; 36:148–152. PMID: 11919449.

14. Wu Y, Green NL, Wrensch MR, Zhao S, Gupta N. Ventriculoperitoneal shunt complications in California : 1990 to 2000. Neurosurgery. 2007; 61:557–562. discussion 562-563. PMID: 17881969.
Fig. 1
CT scan shows an absence of cerebral hemispheres except a small portion of the occipital lobe. However, the thalami, brain stem, and cerebellum are preserved (A and B). Two choroid plexus between thalami are revealed on contrast CT scan (C).





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download