Abstract
Treatment of complex aneurysms usually entails not only direct clipping but also alternative treatment modality. We recently experienced a case of vertebral artery dissecting aneurysm and obtained good treatment outcomes. Our case suggests that the endovascular segmental occlusion with posterior inferior cerebellar artery (PICA) to PICA side anastomosis might be a good treatment option in patients with complex vertebral artery dissecting aneurysms. A 45-year-old woman has a left vertebral dissecting aneurysm with dizziness. Based on the aneurysmal morphology and the involvement of PICA, the patient underwent side to side anastomosis of the PICA. This was followed by the endovascular segmental coil occlusion. The aneurysmal sac was completely obliterated. At a 2-year follow-up, the patient achieved a good patency of both PICA. In conclusion our case suggests that the endovascular segmental occlusion of the parent artery followed by PICA to PICA bypass surgery through a midline suboccipital approach is a reasonable multimodal treatment option in patients with complex vertebral artery dissecting aneurysms.
The treatment of complex aneurysms usually entails not only direct clipping but also alternative treatment modalities such as proximal occlusion, trapping, revascularization, endovascular treatment because of its shape, location, size, previous treatments, the presence or absence of collateral circulation, intraluminal thrombus, and calcification of the aneurysmal wall. The complexity of these lesions poses treatment challenges for clinician, because they are associated with a high incidence of complications. Therefore, considerable expertise is required to manage such lesions.
We recently experienced a case of complex aneurysms. Our case suggests that the endovascular segmental occlusion followed by posterior inferior cerebellar artery (PICA) to PICA side anastomosis might be a good treatment option in patients with complex vertebral artery dissecting aneurysms.
A 45-year-old woman was admitted to our hospital with a chief complaint headache and dizziness. On initial neurologic examinations, the patient had no neurologic signs. A 3-dimensional computed tomography angiography scan on admission showed left vertebral artery stenosis. On day 5, the patient underwent magnetic resonance angiography at a follow-up, showing no interval change of left vertebral artery stenosis (Fig. 1). On day 10, the patient underwent transfemoral cerebral angiography (TFCA) showing complex vertebral dissecting aneurysm of long segment arising from the PICA (Fig. 2). These findings were suggestive of a sign of impending rupture of left vertebral artery dissecting aneurysm because a short-term follow-up radiography revealed a change in the vessel contour. In this patient, we decided on the segmental occlusion using a coil with stent insertion of contralateral vertebral artery after PICA-to-PICA bypass surgery because of the proximity and parallel course of the distal segments of the PICA (Fig. 3). Because simple stenting method had still risk for rupture of aneurysm after intervention and parent artery occlusion had risk for ipsilateral PICA territory infarction, we decided that.
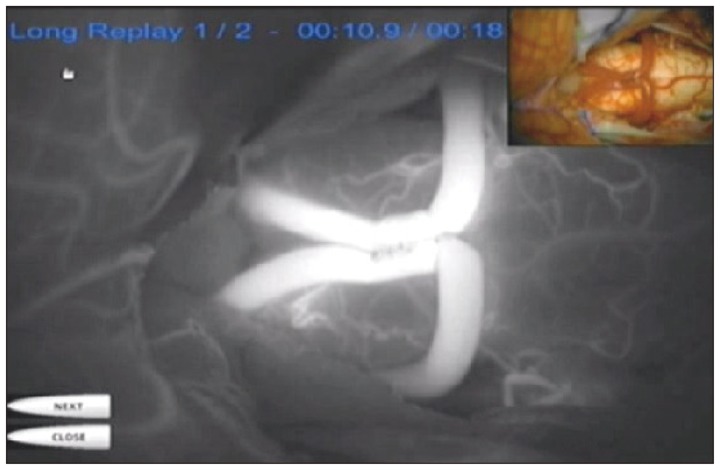
After a midline suboccipital craniotomy, the cisterna magna was opened. After temporary clipping of proximal and distal PICA and perforating artery, a curved incision rather than a straight one along the PICA was done. To do this, the distal end of both PICA was stay-sutured. This was followed by the continuous suture from outside to inside of inner side of the vessel. Then, the final suture was done from inside to outside of the vessel. Following this, the proximal end was also stay-sutured on the external side and then tied with the final inner suture. Moreover, the continuous suture of outer side from outside to inside of the vessel was done in the same manner. After removal of temporary clips, a good patency was also seen on intraoperative indocyanine green angiography (Fig. 4).
On postoperative TFCA, a PICA to PICA anastomosis achieved a good patency of both PICA from the right vertebral artery (VA) (Fig. 5). Then, we performed left VA balloon occlusion test and the both PICA territories showed well. Then, the patient underwent segmental occlusion using a coil with stent insertion of contralateral vertebral artery. The patient finally, achieved a total occlusion of the dissecting aneurysms and a good patency of both PICA territories (Fig. 6). At a 2-year follow-up, the patient underwent uneventful course.
Direct exposure of the aneurysm with clip reconstruction of the parent vessel is the most common treatment strategy. In patients with complex cerebral aneurysms, however, it is somewhat difficult to perform a direct neck clipping of the lesions because of such factors as the shape, location, and size as well as, previous treatments, the presence or absence of collateral circulation, intraluminal thrombus, and calcification of the aneurysmal wall. Therefore, clinicians may often consider alternative modalities such as primary proximal vessel occlusion (Hunterian ligation), distal vessel occlusion, endovascular treatments and trapping with or without flow replacement (bypass)1,2).
Despite recent advancements in the safety and efficacy of endovascular treatments, endovascular modalities reveal their limitations. Rather, the parent artery occlusion with additional bypass surgery is required for complex lesions7). Consequently, the multimodal treatment was both safe and effective in patients with complex aneurysms10).
As mentioned earlier, the dissecting vertebrobasilar aneurysms are one of the complex aneurysms. This poses treatment challenges for clinicians with single standard treatment modality only. It has been proposed that a trapping of the lesion by far-lateral approach be performed to prevent subsequent rupture in patients with a dissecting aneurysm of the vertebral artery. Despite the excellent outcomes of trapping, it does not guarantee resolution of lateral medullary infarction5,6,8). Therefore, but it could be effectively resolved by trapping the aneurysms by far-lateral approach after occipital artery-posterior inferior cerebellar artery (OA-PICA) bypass surgery9). In addition, far-lateral approach enables clinicians to achieve a proximal control and a lateral and parallel view along the axis of the vertebral and basilar arteries. Nevertheless, it causes such complications as lower cranial nerve dysfunction, potential injury to the VA and sigmoid sinus, increased incidence of cerebrospinal fluid leak, occipito-cervical instability and prolonged operation time3,4).
As shown in the current case, however, we could overcome disadvantages of far-lateral approach by performing endovascular segmental occlusion of the parent artery with PICA to PICA bypass surgery. Moreover, we could reduce risks of developing complications and could be less burdened with skull base approach through a midline suboccipital approach. Thus, we could not only avoid lower cranial nerve manipulation, potential injury to the VA and sigmoid sinus, occipito-cervical instability but also shorten the operation time.
The revascularization is effective in occluding the aneurysm without risk of ischemic complications. Then, the superficial temporal artery to middle cerebral artery bypass is a standard treatment modality as one of extracranial-intracranial (EC-IC) bypass surgery. Moreover, the OA-PICA bypass has been used the most frequently as the EC-IC bypass based on the posterior circulation. In recent years, innovative bypass surgeries have been introduced to revascularize the intracranial arteries with other intracranial arteries without extracranial donors. These intracranial-intracranial (IC-IC) bypass surgeries are simple, elegant, and more anatomic than their EC-IC counterparts. In the IC-IC bypass surgeries, there is no need to harvest the extracranial donors, spare patients a neck incision, shorten any interposition grafts, protect them within the cranium, and use caliber-matched donor and recipient arteries. Furthermore, the IC-IC bypass surgeries are more advantageous in treating the complex aneurysms as compared with other types bypass surgeries. Four types of IC-IC bypass techniques, the optimal one is selected based on the aneurysmal anatomy, suitability of the donor artery, depth of the surgical field, and the type of anastomosis. In the current case, we performed the PICA-PICA bypass surgery using a side-to-side anastomosis between the tonsillomedullary segments of both PICAs, for which we required two caudal loops that are sufficiently large and lie next to each other at the entrance to the fourth ventricle.
But a, side-to-side anastomosis is technically more difficult than an end-to-side one because the deep suture line is sewn inside the lumen. It should therefore be avoided in deep, narrow surgical corridors, but can be performed in the Sylvian fissure, cisterna magna, and interhemispheric fissure. But the patients are at risks of developing PICA occlusion when they undergo side-to side anastomosis. Moreover, the IC-IC bypass surgeries may also be performed for patients with aneurysms of the anterior cerebral artery, PICA, basilar apex or, middle cerebral artery, but not to most internal carotid artery (ICA) aneurysms. EC-IC bypasses will remain the preferred choice for ICA aneurysms because they are easier and less risky.
Treatment of complex aneurysms usually entails not only direct clipping but alternative treatment modality. The multimodal treatment was both safe and effective in patients with complex aneurysms. Moreover, we suggest that clinicians perform endovascular segmental occlusion of the parent artery with PICA to PICA bypass surgery through a midline suboccipital approach in patients with vertebral artery dissecting aneurysms. It is effective in occluding the parent artery and obliterating the entire segment of the dissected sites with coils more easily in the posterior fossa. Furthermore, it is a safe modality in protecting the distal side of the parent artery.
References
1. Hacein-Bey L, Connolly ES Jr, Mayer SA, Young WL, Pile-Spellman J, Solomon RA. Complex intracranial aneurysms : combined operative and endovascular approaches. Neurosurgery. 1998; 43:1304–1312. discussion 1312-1313. PMID: 9848843.

2. Hoh BL, Putman CM, Budzik RF, Carter BS, Ogilvy CS. Combined surgical and endovascular techniques of flow alteration to treat fusiform and complex wide-necked intracranial aneurysms that are unsuitable for clipping or coil embolization. J Neurosurg. 2001; 95:24–35. PMID: 11453395.

3. Jamieson KG. Aneurysms of the vertebrobasilar system; surgical intervention in 19 cases. J Neurosurg. 1964; 21:781–797. PMID: 14210010.
4. Kumar CR, Vannemreddy P, Nanda A. Far-lateral approach for lower basilar artery aneurysms. Skull Base. 2009; 19:141–149. PMID: 19721770.

5. Kwon M, Lee JH, Kim JS. Dysphagia in unilateral medullary infarction : lateral vs medial lesions. Neurology. 2005; 65:714–718. PMID: 16157904.

6. Lewis SB, Chang DJ, Peace DA, Lafrentz PJ, Day AL. Distal posterior inferior cerebellar artery aneurysms : clinical features and management. J Neurosurg. 2002; 97:756–766. PMID: 12405360.

7. Pisapia JM, Walcott BP, Nahed BV, Kahle KT, Ogilvy CS. Cerebral revascularization for the treatment of complex intracranial aneurysms of the posterior circulation : microsurgical anatomy, techniques and outcomes. J Neurointerv Surg. 2011; 3:249–254. PMID: 21990836.

8. Redekop G, TerBrugge K, Willinsky R. Subarachnoid hemorrhage from vertebrobasilar dissecting aneurysm treated with staged bilateral vertebral artery occlusion : the importance of early follow-up angiography : technical case report. Neurosurgery. 1999; 45:1258–1262. discussion 1262-1263. PMID: 10549948.
9. Tang ZW, Shi XE, Zhang YL, Zhou ZQ. [Surgical treatment of vertebral artery-posterior inferior cerebellar artery dissecting aneurysms]. Zhonghua Wai Ke Za Zhi. 2010; 48:1805–1810. PMID: 21211386.
10. Xu BN, Sun ZH, Wu C, Jiang JL, Zhou DB, Yu XG, et al. Revascularization for complex cerebral aneurysms. Can J Neurol Sci. 2011; 38:712–718. PMID: 21856573.

Fig. 1
Three dimensional computed tomography angiography shows left vertebral artery mild stenosis on admission day and magnetic resonance angiography shows no interval change of left vertebral artery stenosis on 5th hospital days.
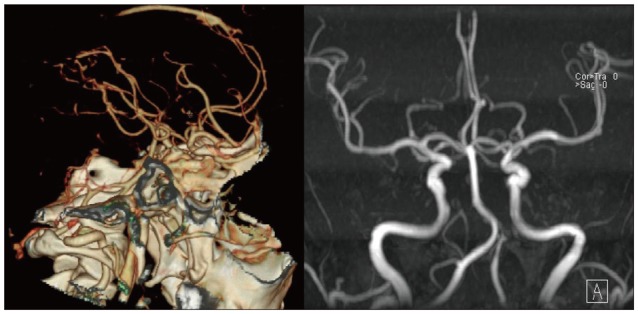
Fig. 2
On day 10, complex vertebral dissecting aneurysm of long segment includs posterior inferior cerebellar artery origin by transfemoral cerebral angiography (AP, Lateral, Oblique view).
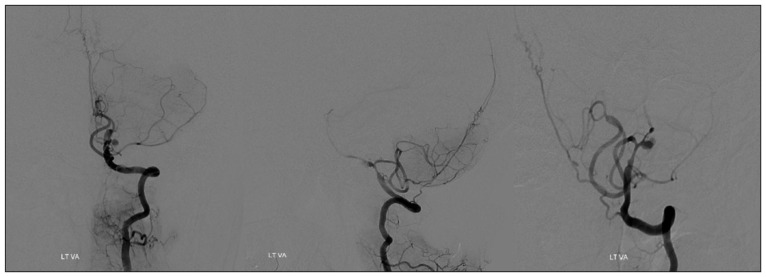
Fig. 3
Tonsilomedullary and telovelotonsilar segments of the right posterior inferior cerebellar artery (PICA) shows parallel course compared with contralateral same segments of PICA.
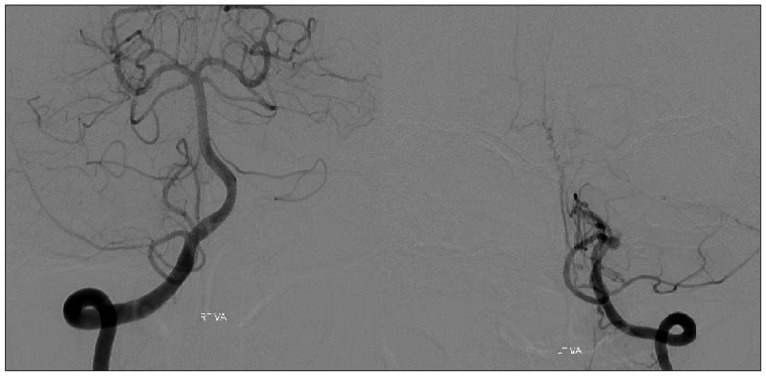
Fig. 4
Posterior inferior cerebellar artery (PICA) to PICA side anastomosis was done and the patency looks well by intraoperative indocyanine green angiography.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download