Abstract
Objective
To evaluate the relationship between postoperative increase in intervertebral disc space height (IVH) and posterior axial neck in cases of degenerative cervical disease treated with anterior cervical discectomy and fusion (ACDF).
Methods
A total of 155 patients who underwent ACDF with more than 1 year follow up were included. Radiologically, IVH and interfacet distance (IFD) of the operated segment were measured preoperatively and postoperatively. We clinically evaluated neck and arm pains according to visual analogue scale (VAS) scores and assessed neck disability index (NDI) scores preoperatively, postoperatively, at 3 months, 6 months, and 1 year postoperatively. The relationship between radiological parameters, and clinical scores were analyzed using a regression analysis.
Results
The mean increase in IVH was 2.62 mm, and the mean increase in IFD was 0.67 mm. The VAS scores for neck pain preoperatively, postoperatively, and at 3 months, 6 months, 1 year postoperatively were 4.46, 2.11, 2.07, 1.95, and 1.29; those for arm pain were 5.89, 3.24, 3.20, 3.03, and 2.18. The NDI scores were improved from 18.52 to 7.47. No significant relationship was observed between the radiological evaluation results regarding the increase in intervertebral height or interfacet distance and clinical changes in VAS or NDI scores.
Conclusion
The increase in intervertebral space or interfacet distance by the insertion of a large graft material while performing ACDF for the treatment of degenerative cervical disease was not related with the change in VAS scores for neck and arm pains and NDI scores postoperatively and during the follow-up period.
Degenerative cervical disease is a major cause of radiating upper extremity pain associated with neurological abnormalities. If the patient does not respond to conservative management, surgical treatment should be considered. Anterior cervical decompression and fusion has been widely accepted as the standard treatment of spinal cord and nerve root compression in the cervical spine since its introduction by Robinson and Smith6,16). After complete decompression of the involved disc space, diverse graft materials such as an autogenous bone block, allograft, or cages are inserted in the decompressed intervertebral spaces. The intervertebral graft is inserted not only for fusion but also for indirect decompression by distraction of the foramina. However, indirect decompression by inserting an oversized graft can lead to subsidence and nonunion3,10). Furthermore, overdistraction by inserting a large graft material was generally considered to lead to postoperative neck pain because of posterior facet joint distraction or posterior neck muscle spasm. However, no evidence that supports the relationship between graft size and postoperative axial neck pain has been available. The purpose of this study was to evaluate the relationship between postoperative increase in intervertebral disc space height and posterior axial neck pain during the postoperative and follow-up periods in cases of degenerative cervical disease treated with anterior cervical discectomy and fusion (ACDF).
Among patients who underwent short-level anterior decompression and fusion for degenerative cervical disc disease between January 2011 and March 2012, 155 were followed up for >1 year and selected as subjects of this study. A total of 107 patients were men and 48 were women, with a mean age of the subjects was 55.1 years (range, 32-78 years). Of the patients, 128 had cervical radiculopathy and 27 had cervical myelopathy. A total of 113 patients had a single-level fusion, whereas 42 had 2-level fusion. The fusion level of surgery was C3-4, C4-5, C5-6, C6-7, and C7-T1 in 13, 31, 95, 55, and 3 cases, respectively.
The surgical method in all the cases involved a standard left approach and anterior decompression. After removal of the anterior longitudinal ligament and disc materials of the involved segment, additional disc space of 2-3 mm was distracted using a Casper pin distracter system. Further decompression was performed by removing the superior and inferior end plates, osteophyte, and remnant disc materials. The posterior longitudinal ligament was resected if necessary. For posterolateral decompression, osteophytic overgrowth in the uncovertebral joint was removed to free the nerve roots. We did not perform total uncovertebral resection. After decompression, the appropriate size of the implant was determined by measuring the length that the nerve root was free. All the patients implanted a stand-alone cage (Zero-P; Synthes GmbH Switzerland, Oberdorf, Switzerland). The implant was packed with local bone tissue obtained from the surgical site and DBX demineralized bone matrix (Musculoskeletal Transplant Foundation, Edison, NJ, USA) before insertion. After confirmation that there was no anterior protrusion by the implant, pilot holes were drilled and four locking screws (14- or 16-mm) were inserted. In cases of C3-4, C6-7, or C7-T1 fusion, drilling and insertion of the locking screws were performed using an angled instrument. All surgeries were performed by a single surgeon. After surgery, the patients each wore a Philadelphia brace for 2 weeks.
Simple radiographs of the cervical lateral views were examined before and after surgery. Postoperative X-ray was checked postoperative 2nd days after removing the hemovac drainage. Plain radiographs of the lateral cervical spine were taken with patients standing with their chins facing forward and their heads placed naturally without tension. Films were centered at the shoulder and the radiation was aligned with the 5th cervical spine and located around 1.8 m from patients to reduce the amplication errors.
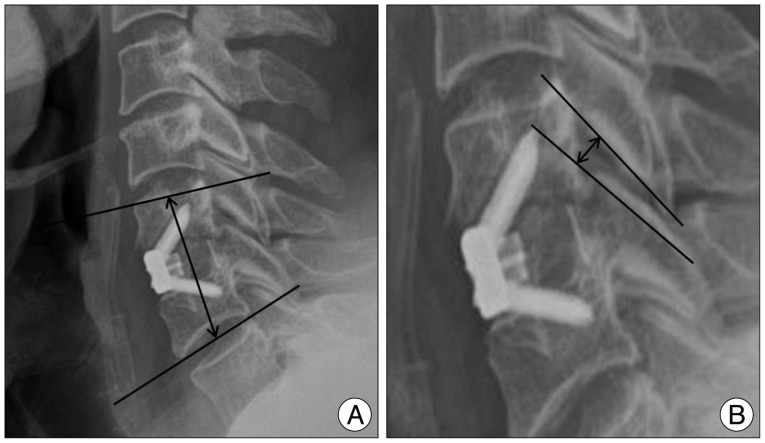
On radiological examination, the intervertebral disc height and interfacet distance of the operated segment were measured preoperatively and postoperatively to evaluate the difference in the values. Increase in postoperative intervertebral disc height was determined based on the difference between the preoperative and postoperative distances of the fusion segment (Fig. 1A). In case of 2-segment fusions, the mean of the 2 values was used. The increase in interfacet distance was evaluated using the difference between the preoperative and postoperative values (Fig. 1B).
We clinically evaluated neck and arm pains according to visual analogue scale (VAS) scores and assessed the neck disability index (NDI) scores preoperatively; postoperatively; and at 3 months, 6 months, and 1 year postoperatively. The incidence of sustained neck pain during the follow-up period was evaluated. The relationships of neck VAS scores between preoperative and follow-up period was also evaluated.
The relationship between the increases in intervertebral space and interfacet distance were evaluated. The relationship between the radiological parameters, and the VAS scores for neck and arm pains and NDI scores were analyzed. The clinical findings were analyzed according to the number of fusion segments.
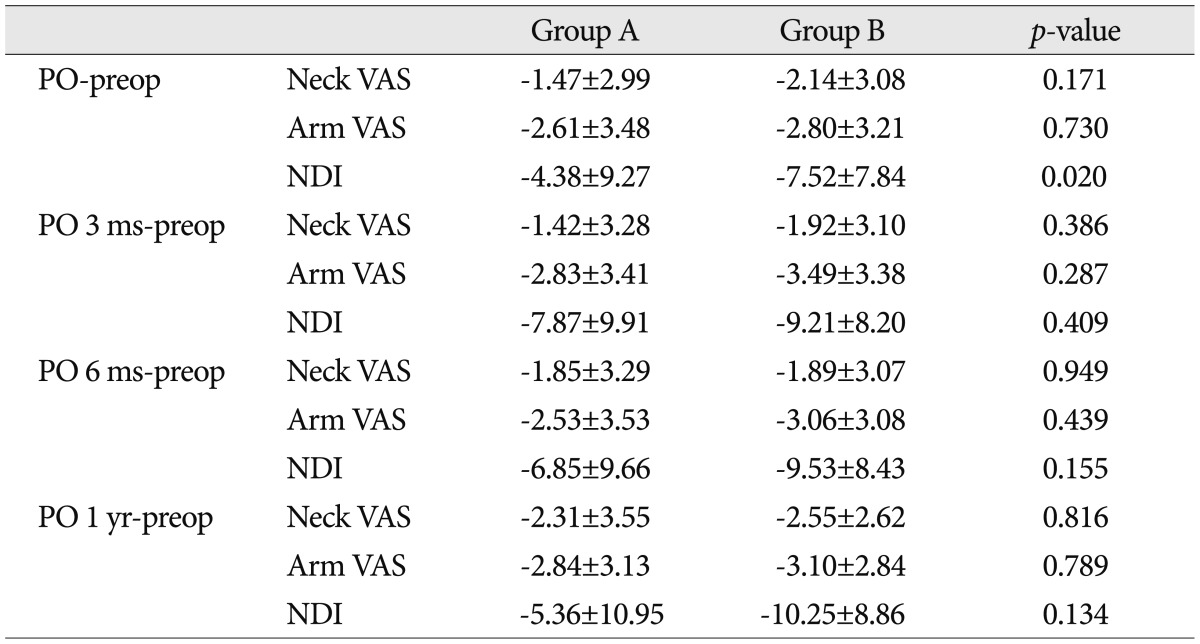
Using the mean increase in intervertebral space of 2.62 mm as reference, the subjects were divided according to the increase in intervertebral space as follows : group A (n=69), <2.62 mm and group B (n=86), >2.62 mm. The changes in neck VAS, arm VAS, and NDI scores at the preoperative and follow-up periods were compared between the 2 groups.
For the statistical analysis, regression analyses were performed to evaluate the relationship between the radiological parameters and clinical outcomes, using SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). A p<0.05 was considered statistically significant.
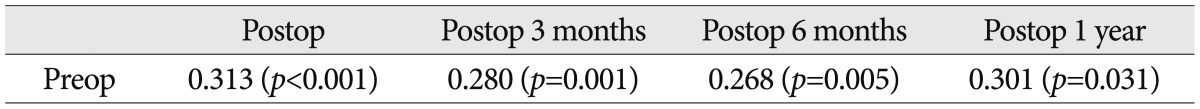
Fifty-five patients (35.4%) showed sustained neck pain during the follow-up period. Thirty patients complained of neck pain at postoperative 3 months; 27, at postoperative 6 months; and 21, until postoperative 1 year. The correlation analysis between preoperative neck VAS scores and neck VAS scores during follow up period showed significant relationship (Table 1). For the treatment of postoperative neck pain, twenty-seven patient performed medical treatment (25 patients of medication, 12 patients of physical therapy, and 2 patients of medial branch block procedure). There showed no significant difference in clinical outcomes according to the treatment method (p=0.39).
The mean increase in intervertebral disc height was 2.62 (±1.47) mm, from 39.04 (±8.13) mm in the preoperative state to 36.42 (±7.65) mm in the postoperative state (2.77 mm for single-level fusion and 2.19 mm for 2-level fusion). The mean increase in the interfacet distance was 0.67 (±0.58) mm, from 2.09 (±0.72) mm in the preoperative state to 2.7 (±0.66) mm in the postoperative state. A significant relationship was observed between the increase in intervertebral space and interfacet distance (p<0.01).
The VAS scores for neck pain preoperatively, postoperatively, and at 3 months, 6 months, and 1 year postoperatively were 4.46, 2.11, and 2.07, 1.95, and 1.29, respectively, whereas those for arm pain were 5.89, 3.24, and 3.20, 3.03, and 2.18, respectively. Meanwhile, the NDI scores were 18.52, 13.0, and 10.7, 10.2, and 7.47, respectively.
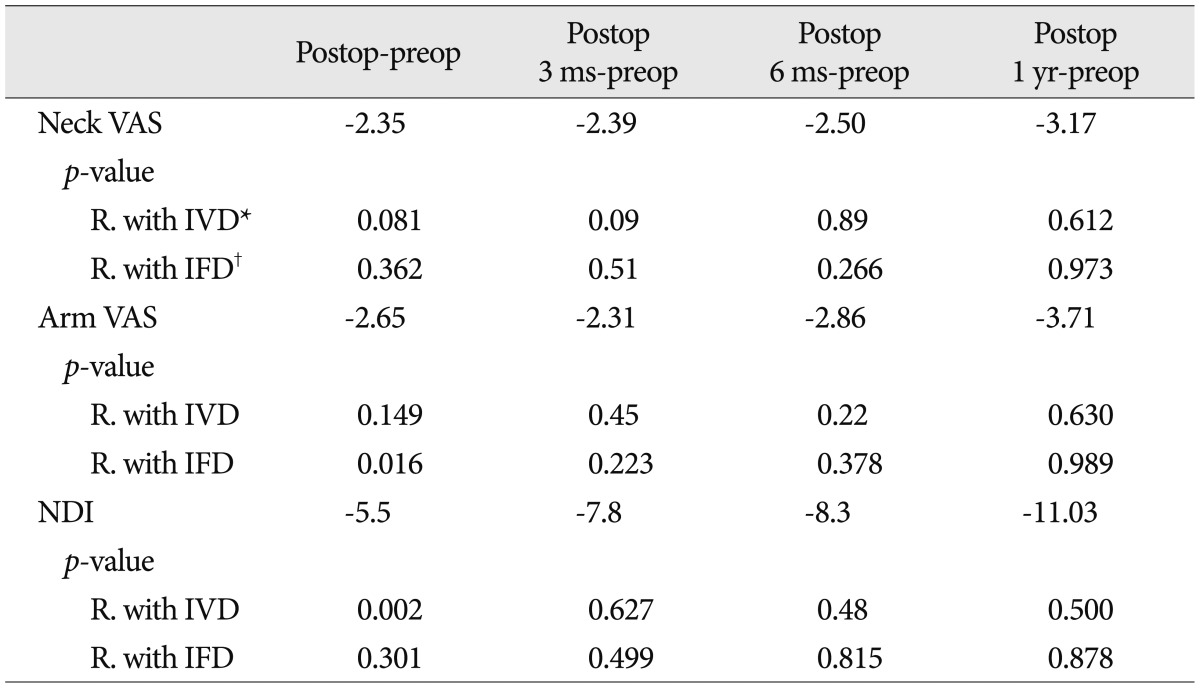
No significant relationship was found between the radiological evaluation results regarding the increase in intervertebral space and clinical scores, except in a postoperative change in the NDI scores (p=0.002) (Table 2).
No significant relationship was observed between the radiological evaluation results regarding the increase in intervertebral space and clinical scores, except in the postoperative change in arm VAS scores (p=0.016) (Table 2).
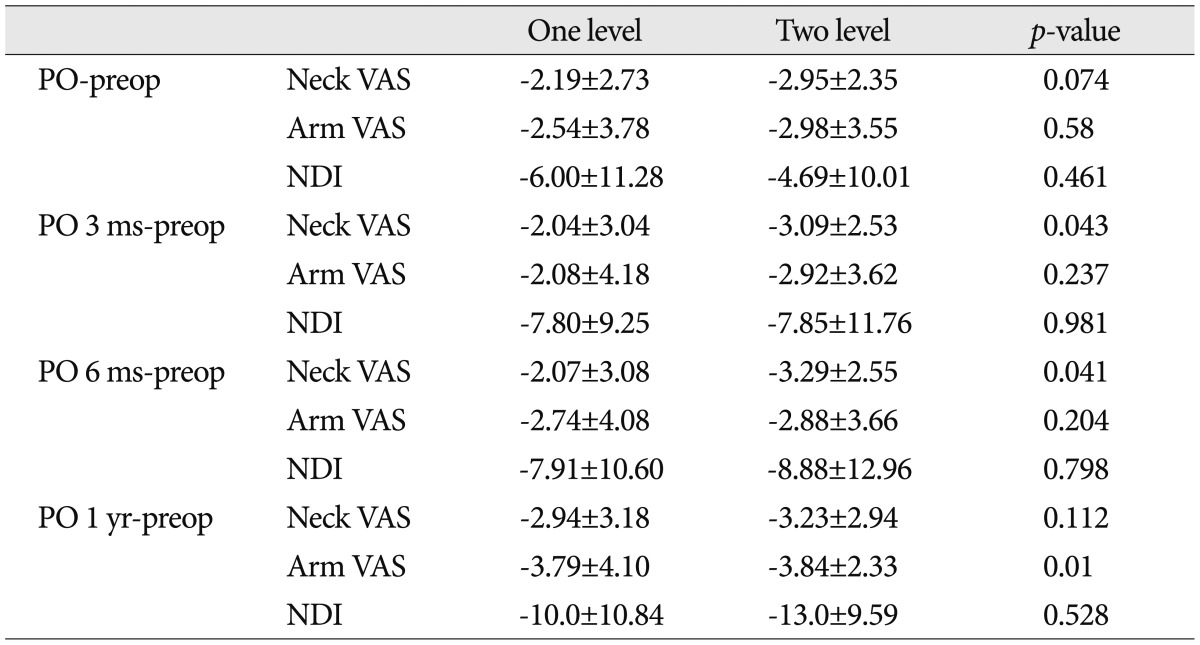
The VAS scores for neck pain were improved in the 2-level fusion cases in comparison with the 1-level fusion cases. However, no significant difference was found between the VAS scores for arm pain or NDI scores (Table 3).
The VAS scores for neck and arm pains, and the NDI scores were much more improved in group B, indicating a greater increase in intervertebral space. However, no significant difference was observed, except in the postoperative change in the NDI scores (p=0.02) (Table 4).
ACDF is a standard surgical treatment method for symptomatic radiculopathy of the cervical spine and myelopathy. Since its initial description and application by Robinson and Smith16), ACDF has shown excellent results based on long-term data, resulting in its current extensive use. However, ACDF can also lead to complications ranging from simple soft tissue swelling to life-threatening conditions such as esophageal rupture or tracheal obstruction. Procedures that involve anterior dissection of the neck can lead to various complications, including dysphonia, dysphagia, and esophageal injuries4). Among the diverse complications, few data exist regarding sustained neck pain after ACDF. Ylinen et al.20) evaluated whether patients acquired normal physical function after anterior cervical surgery compared with the healthy-matched controls. They concluded that more than half (57%) of the patients recovered well after surgery, with still many patients experiencing chronic neck pain and physical dysfunction with decreased neck movement and strength. Another study on neck pain after ACDF was conducted by Matsumoto et al.13), who reported that neck pain was observed in 25.8% of the ACDF patients at the follow-up period. No significant association was observed between neck pain and changes in the cross-sectional area of the posterior muscles over time. Thus, they demonstrated the advantage of ACDF in preserving the posterior muscles, thereby making postoperative axial pain less likely13). In the case of cervical arthroplasty, 25% of patients also reported neck and shoulder pains during follow-up period14). Our result indicated that 35.4% of the patients complained of sustained posterior neck pain.
The underlying mechanism of posterior neck pain has not been fully elucidated. Simple muscle spasm; diseases of the facet joint, intervertebral disc, and ligament; or the instability of the vertebral segment can lead to posterior neck pain. Among the diverse reasons, change in the facet joint is known as an important cause8). Bogduk5) reported that provocative injection in the facet joint led to posterior neck and shoulder pains in asymptomatic volunteers. The mechanism of action of pain provocation by the facet joint was suggested to be via the entrapment of synovial villi, nerve impingement by osteophyte, release of inflammatory mediators, and stretching of the facet joint capsule9,11). Overdistraction by inserting a large graft material was generally considered to lead to postoperative neck pain due to distraction of the posterior facet joint or spasm of the posterior neck muscle15,17). However, no previous study on the relationship between graft size and postoperative axial neck pain has been conducted. Our results demonstrate a significant relationship between the increases in intervertebral disc height and interfacet distance, indicating that a large graft material lead to an increase in interfacet distance. Although 35.4% had posterior neck pain after ACDF, most of the neck pain improved after operation and were relieved during the follow-up period. Moreover, no significant relationship was observed between the radiological evaluation results regarding the increase in the intervertebral space and clinical findings.
During the ACDF procedure, adequate disc height distraction with restoration of sagittal alignment can potentially increase foraminal height and width1). Using cadaveric spines and computed tomographic analysis, the foraminal cross-sectional area in the cervical spine was demonstrated to be increased during ACDF by increasing the interbody graft height2). This increase in foraminal cross-sectional area represents increased space for the existing nerve root; it may result in improved vascular supply and relieves direct compression on an already-compromised nerve. Bayley et al.3) also reported similar results through a cadaver study. They concluded that anterior discectomy and distraction with strut graft can significantly improve the space available for the cord and foraminotomy, which risks iatrogenic injury to the cord, but may not always be necessary for improving clinical radiculopathy and myelopathy. The ideal thickness of the Smith-Robinson graft for anterior cervical fusion seemed to be directly related to the preoperative baseline disc height2). For a preoperative disc height of 3.5-6.0 mm, an interbody graft of 2 mm greater than the baseline thickness was most appropriate. A thicker graft was required when the baseline disc height was smaller (2.0 mm), and a thinner graft was required when the disc height was larger (7.4 mm). In the present study, the postoperative increase in intervertebral space was 2.62 mm.
In the decompression procedure, some authors argue that the optimal and quickest results are achieved through decompression with direct removal of the offending bone spurs7,12). Seo and Ha18) investigated the fate of posterior osteophytes after ACDF using computed tomography. Contrary to previous reports, no evidence of consistent posterior osteophyte resorption was observed during 5 years of follow-up18). Meanwhile, Shen et al.19) evaluated clinical and radiographic outcomes in patients with neck pain and cervical radiculopathy who underwent instrumented ACDF with or without direct uncovertebral joint decompression. They concluded that sacrificing the uncovertebral joint can increase operative time and potentially increase complication rates, and routine direct uncovertebral joint decompression should not be undertaken during ACDF. One of the possible advantages of direct uncovertebral resection is that inserting an oversized graft is not required for indirect decompression. In addition, postoperative neck pain can be attenuated by reducing facet joint distraction. However, our results indicate that overdistraction by the large graft did not lead to the postoperative neck pain. And, there was positive correlation between preoperative neck pain and development of postoperative neck pain during the follow-up period after ACDF. It means not only the overdistraction of facet joint also the other preoperative factor such as degenerative arthritis, muscle spasm, or mal-alignment can be related with the development of postoperative neck pain.
The limitation of this study was due to its retrospective design. Furthermore, our results did not rule out or compensate the diverse possible causes of postoperative neck pain. Therefore, further study is needed to prospectively evaluate the nature of postoperative neck pain after ACDF according to the fusion level, and nature and location of neck pain. And as a tool of analysis, the increased value of intervertebral disc height or interfacet distant after operation cannot be applied equally to all patients due to the difference of preoperative state. However, this is the first study evaluating postoperative neck pain after an ACDF procedure, providing useful information for performing anterior cervical surgery and managing postoperative patients.
Increase in intervertebral space or interfacet distance by the insertion of a large graft material while performing ACDF for the treatment of degenerative cervical disease was not related with the change in VAS scores for neck and arm pains, and NDI scores postoperatively and during the follow-up period. There was positive correlation between preoperative neck pain and development of postoperative neck pain during the follow-up period after ACDF.
References
1. Albert TJ, Smith MD, Bressler E, Johnson LJ. An in vivo analysis of the dimensional changes of the neuroforamen after anterior cervical diskectomy and fusion : a radiologic investigation. J Spinal Disord. 1997; 10:229–233. PMID: 9213279.
2. An HS, Evanich CJ, Nowicki BH, Haughton VM. Ideal thickness of Smith-Robinson graft for anterior cervical fusion. A cadaveric study with computed tomographic correlation. Spine (Phila Pa 1976). 1993; 18:2043–2047. PMID: 8272957.
3. Bayley JC, Yoo JU, Kruger DM, Schlegel J. The role of distraction in improving the space available for the cord in cervical spondylosis. Spine (Phila Pa 1976). 1995; 20:771–775. PMID: 7701388.

4. Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery : a prospective study. Spine (Phila Pa 1976). 2002; 27:2453–2458. PMID: 12435974.
5. Bogduk N. The anatomy and pathophysiology of neck pain. Phys Med Rehabil Clin N Am. 2003; 14:455–472. vPMID: 12948338.

6. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993; 75:1298–1307. PMID: 8408151.

7. Brigham CD, Tsahakis PJ. Anterior cervical foraminotomy and fusion. Surgical technique and results. Spine (Phila Pa 1976). 1995; 20:766–770. PMID: 7701387.

8. Cavanaugh JM, Lu Y, Chen C, Kallakuri S. Pain generation in lumbar and cervical facet joints. J Bone Joint Surg Am. 2006; 88(Suppl 2):63–67. PMID: 16595446.

9. Cavanaugh JM, Ozaktay AC, Yamashita HT, King AI. Lumbar facet pain : biomechanics, neuroanatomy and neurophysiology. J Biomech. 1996; 29:1117–1129. PMID: 8872268.
10. Emery SE, Bolesta MJ, Banks MA, Jones PK. Robinson anterior cervical fusion comparison of the standard and modified techniques. Spine (Phila Pa 1976). 1994; 19:660–663. PMID: 8009330.
11. Igarashi A, Kikuchi S, Konno S, Olmarker K. Inflammatory cytokines released from the facet joint tissue in degenerative lumbar spinal disorders. Spine (Phila Pa 1976). 2004; 29:2091–2095. PMID: 15454697.

12. Jho HD. Microsurgical anterior cervical foraminotomy for radiculopathy : a new approach to cervical disc herniation. J Neurosurg. 1996; 84:155–160. PMID: 8592215.

13. Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, et al. Changes in the cross-sectional area of deep posterior extensor muscles of the cervical spine after anterior decompression and fusion : 10-year follow-up study using MRI. Eur Spine J. 2012; 21:304–308. PMID: 21858566.

14. Pickett GE, Sekhon LH, Sears WR, Duggal N. Complications with cervical arthroplasty. J Neurosurg Spine. 2006; 4:98–105. PMID: 16506475.

15. Ponnappan RK, Nassr A, Kang JD. Anterior decompression, instrumentation, fusion techniques : discectomy, foraminotomy, disc space carpentry. In : Bridwell KH, Dewald RL, editors. The Textbook of Spinal Surgery. ed 3. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins;2011. p. 258–260.
16. Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for the cervical disc syndrome. Bull John Hopkins Hosp. 1955; 96:223–224.
17. Ryu KS, Park CK, Jun SC, Huh HY. Radiological changes of the operated and adjacent segments following cervical arthroplasty after a minimum 24-month follow-up : comparison between the Bryan and Prodisc-C devices. J Neurosurg Spine. 2010; 13:299–307. PMID: 20809721.

18. Seo JY, Ha KY. Fate of posterior osteophytes in fused segments after anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2012; 37:741–747. PMID: 21912323.

19. Shen FH, Samartzis D, Khanna N, Goldberg EJ, An HS. Comparison of clinical and radiographic outcome in instrumented anterior cervical discectomy and fusion with or without direct uncovertebral joint decompression. Spine J. 2004; 4:629–635. PMID: 15541694.

20. Ylinen JJ, Savolainen S, Airaksinen O, Kautiainen H, Salo P, Häkkinen A. Decreased strength and mobility in patients after anterior cervical diskectomy compared with healthy subjects. Arch Phys Med Rehabil. 2003; 84:1043–1047. PMID: 12881832.

Fig. 1
A : Measurement of intervertebral distance. Length between the center of the superior end plate of upper vertebral body and the inferior end plate of lower vertebral body was measured. B : Measurement of interfacet distance. Longest distance was measured between the facet joint of operated segment.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download