Abstract
Objective
The purpose of this study is to demonstrate the technical feasibility and clinical efficacy of emergent carotid angioplasty and stenting (CAS) for acute stroke due to athero-thrombotic occlusion of the cervical internal carotid artery (ICA).
Methods
Review of medical records identified 17 patients who underwent emergent CAS for treatment of athero-thrombotic occlusion of the cervical ICA with acute stroke between 2009 and 2013. Eleven patients (64.7%) presented with concomitant intracranial artery occlusion, which was treated primarily by mechanical thrombectomy after CAS.
Results
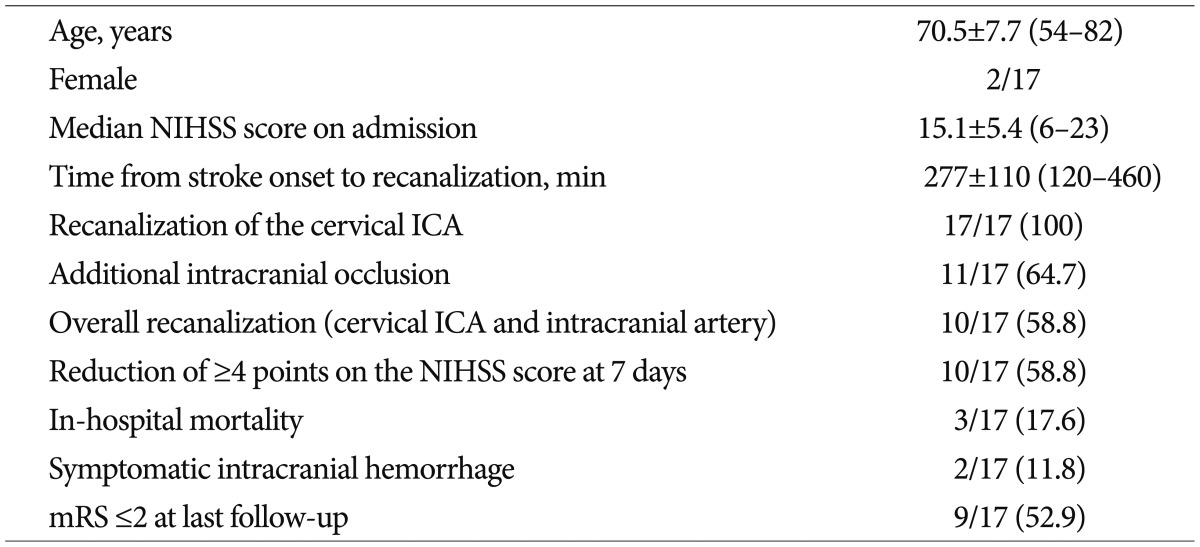
Successful revascularization of the cervical ICA with emergent CAS was achieved in all patients. After CAS, intracranial recanalization with Thrombolysis in Cerebral Infarction ≥2b flow was achieved in four of the 11 patients (36.4%). The overall recanalization rate (cervical ICA and intracranial artery) was 10 of 17 patients (58.8%). Symptomatic intracranial hemorrhage occurred in two patients (11.8%), resulting in death. Ten patients (58.8%) showed improvement (decrease in NIHSS score of ≥4 points) at seven days after recanalization. Nine patients (52.9%) showed a favorable outcome (mRS ≤2) at the last follow-up. A favorable outcome (mRS ≤2) was obtained in four of the six patients with isolated cervical ICA occlusion (4/6, 66.7%) and five of 11 patients with intracranial tandem occlusion (5/11, 45.5%).
The natural history of acute cervical internal carotid artery (ICA) occlusion with serious neurological symptom is unfavorable1). Treatment for acute occlusion of the cervical ICA includes intravenous administration of tissue plasminogen activator (tPA), percutaneous transluminal angioplasty, carotid endarterectomy (CEA), and extracranial-to-intracranial (EC-IC) artery bypass. According to the current literature, the recanalization rate for carotid occlusion with systemic (intravenous) tPA alone ranges from 15% to 35%. A good outcome has been documented for 20% to 44% of patients treated with intravenous tPA alone for acutely symptomatic ICA occlusion4,17). Despite the proven benefit of CEA in prevention of stroke recurrence in patients with a high-grade stenosis of the ICA2,25), few studies of emergency CEA for improvement of their neurologic symptoms and no rigorous clinical trials regarding the efficacy of CEA in an acute stroke stage have been reported3,18). A few studies have attempted to determine whether emergent EC-IC bypass surgery is an effective treatment for main trunk stenosis or occlusion in acute stage12).
Previous studies have supported carotid angioplasty and stenting (CAS) as a technique for secondary prevention in the chronic stroke stage8,29). However, CAS in the acute stage remains challenging because of the limited therapeutic window and risk of hyperperfusion syndrome after revascularization. Nevertheless, there have been some reports on the safety and effectiveness of emergency CAS, even in the acute stage of ischemic stroke7,14,15,19,21,27,28,30).
The purpose of this study is to demonstrate the technical feasibility and clinical efficacy of emergent CAS for acute stroke due to athero-thrombotic occlusion of the cervical ICA.
Medical records identified 17 patients who underwent emergent CAS for treatment of acute stroke related to an athero-thrombotic cervical ICA occlusion between 2009 and 2013. All patients underwent examination by computed tomographic (CT) perfusion imaging, followed by magnetic resonance (MR) imaging before conventional angiography. The indication for emergent CAS was determined by mismatch between the diffusion-weighted MR imaging finding of localized high intensity areas and the CT perfusion finding of decreased CBF related to the occluded ICA. Patients who present within 4.5 hours of symptom onset and without contraindication to systemic thrombolysis are treated immediately with intravenous tPA (0.9 mg/kg) and, unless immediate neurological improvement is observed, are then transferred rapidly to the angiography suite. In contrast, patients who present between 4.5 and 6 hours after symptom onset do not undergo systemic thrombolysis, but are transferred immediately to the neurointerventional suite.
Patients matching the following criteria were included in our analysis : 1) onset of acute stroke symptom and arrival at the hospital within 6 hours, 2) National Institutes of Health Stroke Scale (NIHSS) score on admission ≥5, 3) athero-thrombotic occlusion of the cervical ICA confirmed by catheter-based angiography : as the balloon configuration during inflation and features of residual stenosis after predilatation or the stent configuration before balloon angioplasty, and 4) negative findings on brain CT or limited hypodensities involving less than one-third of the middle cerebral artery (MCA) territory. We excluded patients in whom a dissection of the ICA was diagnosed due to the different nature of the disease. Patients with radiologic signs of chronic ICA occlusions were also excluded. Patients presenting with transient ischemic attack (TIA) were excluded from the analysis. TIA was defined as an acute transient focal neurological deficit caused by vascular disease, which showed a complete reversal within 24 hours, and caused no acute lesion, as confirmed by diffusion-weighted MR imaging.
Interventional procedures were performed in the neuroangiography room equipped with a digital subtraction angiography system (Axiom Artis, Siemens, Germany). All angiographic procedures were performed using a transfemoral approach under local anesthesia using an electrocardiogram, arterial oxygen saturation, and blood pressure monitoring. Four-vessel angiography was performed for estimation of collateral flow from the anterior and posterior communicating arteries, and to determine the presence of concomitant intracranial artery occlusion. The interventional treatment consists of two steps : first, emergent CAS for athero-thrombotic occlusion of the cervical ICA, and second, intracranial recanalization. A loading dose of 300 mg clopidogrel plus 300 mg aspirin was administered before endovascular treatment. Prior to the therapeutic procedure, patients were administered a systemic heparinization and a bolus injection of heparin 3000 IU. An additional 1000 IU bolus of heparin was administered every hour in order to maintain an ACT of >200 seconds throughout the procedure. Coaxial catheter-flushing fluid was mixed with heparin at a concentration of 1000 IU of heparin per 1000 mL of saline.
An 8 Fr guiding catheter (Envoy; Cordis, Miami Lakes, FL, USA) or 6 Fr Shuttle sheath was advanced to the common carotid artery, and it was connected to a continuous saline flush. A 0.014-in microwire (Transend; Boston Scientific, Natick, MA, USA) was placed into the petrous ICA passing the occluded segment. Then, a self-expandable stent was advanced over the microwire and positioned across the occlusion. A stent deployment and balloon angioplasty were performed with or without distal protection device (Spider device, ev3, Plymouth, MN, USA) to prevent distal embolic event.
The entire length of the ICA and the intracranial area was then imaged for determination of whether there was any further stenosis or occlusion of the ICA or MCA. If there was no distal patency of the ICA, we attempted restoration of distal flow using forced arterial suction thrombectomy using a 50-mL syringe. If an additional occlusion was present in the terminal segment of the ICA or MCA, a 6 Fr guiding catheter was advanced as far as possible into the recanalized ICA. The devices used for mechanical thrombectomy were the Penumbra system (Penumbra Inc., Alameda, CA, USA) or the Solitaire AB/FR (ev3 Europe SAS, Paris, France) with or without additional intra-arterial thrombolysis with urokinase. We initially attempted forced arterial suction thrombectomy using a Penumbra reperfusion catheter, but switched to Solitaire in difficult cases, which means failed thrombectomy despite several attempts at recanalization.
Immediately after the therapeutic procedure, we obtained the detailed neurologic history and performed a complete examination of all patients. The patients underwent non-enhanced brain CT imaging for evaluation of possible hemorrhagic complications. Following endovascular stent placement, patients were transferred to a stroke intensive care unit for strict control of blood pressure for prevention of hyperperfusion syndrome.
After the procedure, patients were administered aspirin 100 mg and clopidogrel 75 mg daily. Low-molecular-weight nadroparin calcium (Fraxiparine; GlaxoSmithKline, Marly-le-Roi Cedex, France) 2850 IU was also administered subcutaneously three times per day for at least three days.
Technical success of emergent CAS was defined as restoration of ICA flow with more than 50% recanalization of the cervical ICA. Intracranial arterial recanalization was assessed using the Thrombolysis in Cerebral Infarction (TICI) scores and was recorded prospectively at the end of each case by the treating interventionalist11). Angiographic success of intracranial arterial recanalization was defined as restoration of ICA flow with normal or near-normal perfusion in the ipsilateral ICA territory (TICI ≥2b flow).
For clinical outcome evaluation, the NIHSS was checked on admission and at seven days after the procedure. Improvement of neurological function was defined as reduction of ≥4 points on the NIHSS at seven days after the procedure compared with baseline. In addition, clinical functional outcome was assessed upon discharge from hospital or at the last clinical visit using the modified Rankin Scale (mRS). A score of ≤2 was considered a favorable outcome.
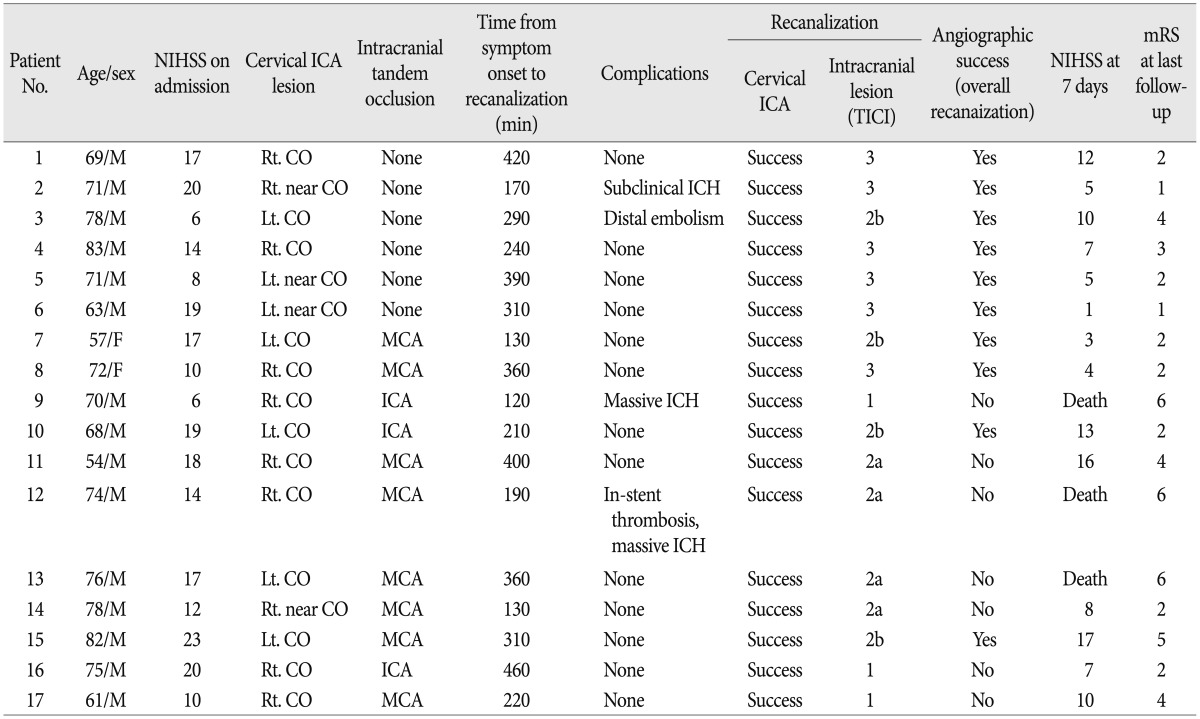
The 17 patients with acute stroke related to athero-thrombotic cervical ICA occlusion were treated by emergent CAS between 2009 and 2013. The mean age of the patients (15 men and 2 women) was 70.5±7.7 years (range, 54-82 years). The patients' mean NIHSS score on admission was 15.1±5.4 (range, 6-23). All patients had an NIHSS score of at least 6 on admission. Six patients had contraindications to intravenous administration of tPA, however, the others received a standard 10% bolus of the maximum dose (0.9 mg/kg body weight). The mean time from stroke onset to recanalization was 277±110 minutes (range, 120-460 minutes).
Angiography showed complete occlusion in 13 patients and near complete occlusion in four. Stents were deployed uneventfully and the cervical ICA was recanalized successfully in all cases. Some difficulties were encountered during passage of the guidewire through the occluded segment; it was possible in all cases. In six patients, no further vessel occlusion was detected after successful recanalization of the cervical ICA (Fig. 1). A distal protection filter was used selectively. The stent used was Protégé (ev3, Plymouth, MN, USA) in 15 patients and Wallstent (Boston Scientific, Natick, MA, USA) in two. Of 17 patients, 11 (11/17, 64.7%) showed an additional intracranial occlusion after flow restoration in the cervical ICA (Fig. 2) : at the level of the terminal segment of the ICA (n=3) and at the level of the MCA in eight patients. Intracranial arterial recanalization to a TICI ≥2b flow was achieved in four of 11 patients (36.4%). The overall recanalization rate (cervical ICA and intracranial artery) was 10 of 17 patients (58.8%).
Procedure-related complications developed in two patients (2/17, 11.8%). In Patient 3, although a distal protection filter was used, distal embolism occurred after CAS. Immediate thrombolysis using a combination of mechanical thrombectomy and intraarterial urokinase led to recanalization to a TICI 2b flow. However, afterward, relevant infarction was observed and his neurological status worsened. In one patient who suffered acute in-stent thrombosis, abciximab was administered intraarterially with a maintenance drip, yielding stent recanalization; however, the patient subsequently developed massive intracranial hemorrhage (ICH) and died (Patient 12). Thus, procedure-related mortality was 5.9% (1/17, Patient 12) and morbidity was 5.9% (1/17, Patient 3), respectively.
Ten of 17 patients (58.8%) showed improvement (decrease in NIHSS score of ≥4 points compared with admission score) during the hospital course at seven days after recanalization. Follow-up CT scan obtained immediately after each intervention showed occasional enhancement around the area of ischemia, which had resolved by the time the scan was repeated later. Three patients (3/17, 17.6%) had an ICH after CAS. These hemorrhages occurred within 48 hours after treatment. In two of them, the ICH was symptomatic with neurologic deterioration, resulting in death (Patients 9 and 12). The other patient suffered an asymptomatic hemorrhage in the basal ganglia (Patient 2). One patient (Patient 13) died secondary to pneumonia and sepsis 21 days after the procedure. Thus, there were three in-hospital deaths (3/17, 17.6%), respectively. At the end of the observational period, nine patients showed a good clinical outcome, with an mRS score of ≤2 (9/17, 52.9%), while the other eight (8/17, 47.1%) were dependent or dead (mRS score, 3-6). All surviving patients were followed up for 6-21 months (mean, 12.5 months). No neurologic deterioration or ischemic event occurred during the follow-up period in all surviving patients. A summary of characteristics and clinical outcomes according to existence of intracranial tandem lesion is shown in Table 3. Near-complete occlusion of the cervical ICA was identified in half of patients without an intracranial tandem lesion, while in only one patient with an intracranial tandem lesion. A favorable outcome (mRS ≤2) was obtained in four of the six patients with isolated cervical ICA occlusion (66.7%) and five of 11 patients with intracranial tandem occlusion (45.5%) at the last follow up. No patient with isolated cervical ICA occlusion suffered from a symptomtic ICH or in-hospital mortality, However, there were two cases of symptomtic ICH (18.2%) and three cases of in-hospital mortality (27.3%) in the patients with intracranial tandem occlusion. More favorable outcomes were achieved in patients without intracranial tandem lesion, compared to a patient population with intracranial tandem lesion. Representative cases are shown in Fig. 1, 2.
The natural history of acute cervical ICA occlusion with serious neurologic symptoms is unfavorable1). For these types of lesions, treatment with standard intravenous thrombolysis alone leads to a good clinical outcome in only 17% of cases with a death rate of as high as 55%18). Currently, there is no consensus treatment for patients with acute ischemic stroke presenting with severe clinical symptoms due to athero-thrombotic occlusion of the cervical ICA.
Acute cervical ICA occlusion resulting in ischemic stroke is different from other forms of acute occlusion of cerebral vessels. Occluded segments in other cerebral vessels, such as the MCA and the terminal segment of the ICA, usually consist of an occlusive embolus in a normal vessel23). The ECASS III showed that intravenous tPA is effective in treatment of acute ischemic stroke if given to patients within 4.5 hours of stroke symptom onset. However, the recanalization rates achieved with intravenous tPA for large vessel arterial occlusion are low, ranging from 4% to 32%, depending on the vessel (4% for ICA occlusions and 32% for MCA occlusions)9). In addition, cervical ICA occlusion is associated with a high incidence of intracranial tandem occlusions. Rubiera et al.26) reported on the presence of a tandem lesion (ICA and MCA) as an independent predictor of poor outcome after intravenous thrombolysis. According to Linfante et al.,17) a significant difference was observed between the proportion of recanalization in MCA-only occlusions (15 of 17 recanalized, 88%) at three days after tPA compared with that in ICA-MCA tandem occlusions (five of 16 recanalized, 31%). Improvement in clinical outcome showed a close association with resumption of MCA flow, and most ICA occlusions did not recanalize after intravenous tPA therapy. The pathophysiologic processes involved in occlusion of the extracranial ICA are similar to processes observed in acute occlusion of the coronary arteries. The occluded segment of the ICA consists of a predominantly atherosclerotic plaque and a superimposed thrombus. Therefore, large contributions of atherosclerotic plaque and platelet activation do not provide an ideal substrate for thrombolytics alone23,24). In acute myocardial infarction, primary stent placement has provided the best treatment outcomes16,31). In summary, the recanalization rate for carotid occlusion with intravenous tPA alone is very low, ranging from 15% to 35%. A good outcome has been documented for 20% to 44% of patients treated with intravenous tPA alone for acutely symptomatic ICA occlusion.
Surgery, specifically CEA, is limited to the cervical region. The intracranial vasculature is beyond reach in the acute setting. Nevertheless, there is currently an interest in "early" CEA after intravenous tPA for prevention of further stroke. However, CEA is not suited for patients in an emergency situation such as acute stroke because control of the intracranial extension of the clot is extremely limited. Surgical bypass may be a natural resolution for ICA occlusion, however, a large international randomized EC-IC bypass trial failed to show any benefit22).
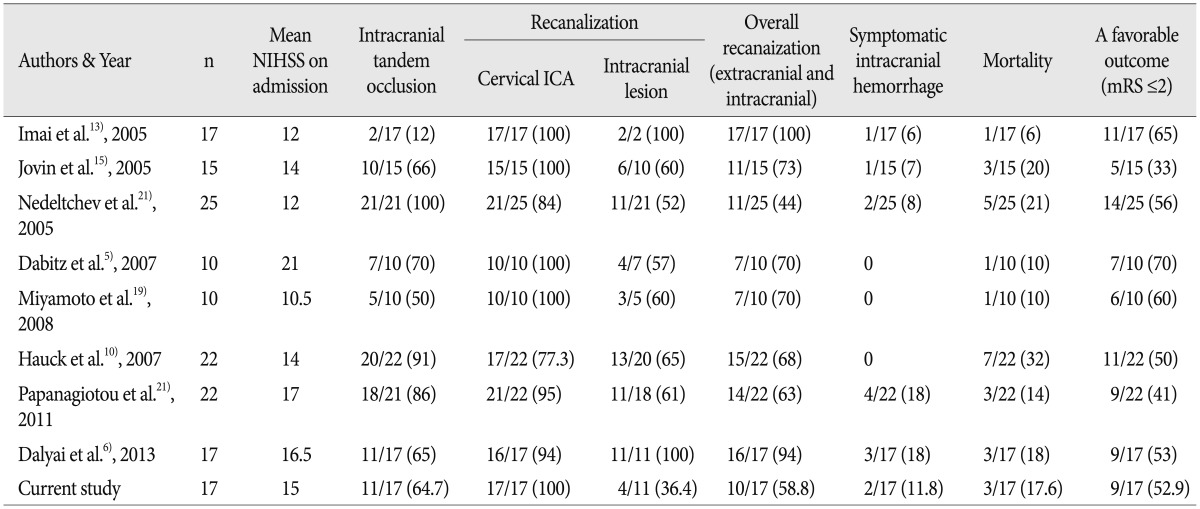
Recently, there has been a surge of interest in endovascular interventions for acute ICA occlusion5,6,10,13,15,19,20,21). We have summarized the reported studies in which more than 10 patients with acute cervical ICA occlusion were treated with CAS in Table 4. Imai et al.13) treated 17 patients with either occlusion or a high-grade stenosis of the ICA with emergent CAS. Median NIHSS scores before emergency stent placement and at seven days were 12 and 5, respectively (p<0.01). Eleven patients (65%) showed favorable outcomes (mRS score, 0-2) at 90 days. Dabitz et al.5) reported on their experience with 10 patients with an average NIHSS score of 21 using a combination of CAS and intra-arterial thrombolysis for treatment of the cervical ICA occlusion; 70% had an mRS of ≤2 after 20 weeks. Hauck et al.10) reported that 17 of 22 patients (77.3%) underwent successful revascularization with CAS and 50% of patients showed good outcomes (mRS ≤2) after a median follow-up of three months. Patients with complete cervical ICA occlusion but partial distal preservation of the vessel were most likely to benefit from the intervention. Papanagiotou et al.21) treated 22 patients with acute atherosclerotic extracranial ICA occlusion with emergent CAS and intraarterial thrombolysis using mechanical thrombectomy. Fourteen of 22 patients (63%) underwent successful overall revascularization and nine patients (41%) had an mRS of ≤2 at 90 days. Dalyai et al.6) reported on their experience with 17 patients using a combination of CAS and intraarterial thrombolysis for treatment of proximal ICA occlusion. Mean NIHSS scores on admission and at discharge were 16.5 and 6.9, respectively. The results of our study combined with the results of these series indicate that this approach is also feasible for athero-thrombotic occlusion of the cervical ICA.
After CAS of an ICA occlusion, an additional occlusion may be present in the terminal segment of the ICA or the MCA. In our study, acute cervical ICA occlusion presented frequently (64.7%) as a tandem lesion with intracranial extension of the clot, usually into the MCA branches or the carotid terminus. In the event of additional intracranial occlusion, further recanalization measures should be taken. A mechanical approach should be the first option for treatment of these lesions. For these cases, we used the Penumbra system or the Solitaire stent. However, the angiographic result was somewhat disappointing, with achievement of a recanalization rate of 36.4%. Revascularization of intracranial artery occlusion requires a significant amount of time; however, the therapeutic time window is narrow because of less collateral flow from the anterior communicating artery and/or posterior communicating artery, compared with that for isolated cervical ICA occlusion. In some cases, we should have stopped further revascularization of intracranial artery occlusion because of exceeding the therapeutic time window. We found that patients without a tandem occlusion were more likely to show rapid neurologic improvement within the first seven days after CAS and a mRS ≤2 at follow-up (Table 3); this has also been previously reported in the literature10,19,21).
However, due to the risk of reperfusion injury, such as hyperperfusion syndrome or hemorrhagic transformation, successful recanalization does not always result in a favorable outcome. Although the incidence of hyperperfusion syndrome after CAS is 5% to 7%, it is expected to be higher in emergent recanalization of the cervical ICA. Symptomatic ICH rate of 12% (n=2) in the current study is similar to the previously reported rates for CAS in acute stroke (6% to 18%)6,13,15,20,21). Due to the aggressive anticoagulation required, the risk of ICH is expected to be higher in acute CAS compared with mechanical recanalization studies. In our series, there was one case of acute in-stent thrombosis; prompt use of intraarterial abciximab yielded thrombolysis, however, subsequently developed massive ICH and died. Strict postoperative control of blood pressure is most important in prevention of this complication. The diffusion/perfusion mismatch indicative of ischemic penumbra is useful for selection of patients who might benefit from recanalization.
In our series, emergent endovascular recanalization of the cervical ICA and distal branches was technically successful in 58.8% (10 patients) overall. At the last follow-up, good clinical outcome (mRS ≤2) with endovascular intervention was observed in nine of 17 patients (52.9%) overall and in seven patients (7/10, 70.0%) in whom revascularization was successful. Our observation that endovascular revascularization of an acutely occluded ICA at the cervical level has a fairly high chance of success exceeding the rate of recanalization with intravenous tPA alone is similar to the findings of several previous reports in the literature. The current study showed that patients with cervical ICA occlusion with acute stroke presentation could benefit from endovascular revascularization, although these findings should be confirmed in a larger study with multivariate logistic regression analysis.
Emergent CAS for acute stroke due to athero-thrombotic occusion of the cervical ICA showed a good technical feasibility and favorable clinical outcome. In particular, emergent CAS is more beneficial in patients with isolated cervical ICA occlusion. Treatment of intracranial tandem occlusions is an issue that must be resolved in order to achieve a favorable outcome.
References
1. Adams HP Jr, Bendixen BH, Leira E, Chang KC, Davis PH, Woolson RF, et al. Antithrombotic treatment of ischemic stroke among patients with occlusion or severe stenosis of the internal carotid artery : A report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology. 1999; 53:122–125. PMID: 10408547.

2. Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998; 339:1415–1425. PMID: 9811916.

3. Brandl R, Brauer RB, Maurer PC. Urgent carotid endarterectomy for stroke in evolution. Vasa. 2001; 30:115–121. PMID: 11417281.
4. Christou I, Felberg RA, Demchuk AM, Burgin WS, Malkoff M, Grotta JC, et al. Intravenous tissue plasminogen activator and flow improvement in acute ischemic stroke patients with internal carotid artery occlusion. J Neuroimaging. 2002; 12:119–123. PMID: 11977905.

5. Dabitz R, Triebe S, Leppmeier U, Ochs G, Vorwerk D. Percutaneous recanalization of acute internal carotid artery occlusions in patients with severe stroke. Cardiovasc Intervent Radiol. 2007; 30:34–41. PMID: 17122887.

6. Dalyai RT, Chalouhi N, Singhal S, Jabbour P, Gonzalez LF, Dumont AS, et al. Stent-assisted endovascular recanalization of extracranial internal carotid artery occlusion in acute ischemic stroke. World Neurosurg. 2013; 79:143–148. PMID: 23022651.

7. Du Mesnil De Rochemont R, Sitzer M, Neumann-Haefelin T, Harmjanz A, Berkefeld J. Endovascular recanalization of acute atherothrombotic carotid artery occlusion holds up progressive stroke. Neuroradiology. 2004; 46:583–586. PMID: 15168098.

8. Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomised trial. Lancet. 2001; 357:1729–1737. PMID: 11403808.
9. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329. PMID: 18815396.

10. Hauck EF, Natarajan SK, Ohta H, Ogilvy CS, Hopkins LN, Siddiqui AH, et al. Emergent endovascular recanalization for cervical internal carotid artery occlusion in patients presenting with acute stroke. Neurosurgery. 2011; 69:899–907. discussion 907. PMID: 21499144.

11. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003; 34:e109–e137. PMID: 12869717.

12. Horiuchi T, Nitta J, Ishizaka S, Kanaya K, Yanagawa T, Hongo K. Emergency EC-IC bypass for symptomatic atherosclerotic ischemic stroke. Neurosurg Rev. 2013; 36:559–564. discussion 564-565. PMID: 23821132.

13. Imai K, Mori T, Izumoto H, Watanabe M, Majima K. Emergency carotid artery stent placement in patients with acute ischemic stroke. AJNR Am J Neuroradiol. 2005; 26:1249–1258. PMID: 15891193.
14. Iwata T, Mori T, Tajiri H, Miyazaki Y, Nakazaki M. Safety and effectiveness of emergency carotid artery stenting for a high-grade carotid stenosis with intraluminal thrombus under proximal flow control in hyperacute and acute stroke. J Neurointerv Surg. 2013; 5:40–44. PMID: 22170821.

15. Jovin TG, Gupta R, Uchino K, Jungreis CA, Wechsler LR, Hammer MD, et al. Emergent stenting of extracranial internal carotid artery occlusion in acute stroke has a high revascularization rate. Stroke. 2005; 36:2426–2430. PMID: 16224082.

16. Le May MR, Labinaz M, Davies RF, Marquis JF, Laramée LA, O'Brien ER, et al. Stenting versus thrombolysis in acute myocardial infarction trial (STAT). J Am Coll Cardiol. 2001; 37:985–991. PMID: 11263625.

17. Linfante I, Llinas RH, Selim M, Chaves C, Kumar S, Parker RA, et al. Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke. 2002; 33:2066–2071. PMID: 12154264.

18. Meyer FB, Sundt TM Jr, Piepgras DG, Sandok BA, Forbes G. Emergency carotid endarterectomy for patients with acute carotid occlusion and profound neurological deficits. Ann Surg. 1986; 203:82–89. PMID: 3942424.

19. Miyamoto N, Naito I, Takatama S, Shimizu T, Iwai T, Shimaguchi H. Urgent stenting for patients with acute stroke due to atherosclerotic occlusive lesions of the cervical internal carotid artery. Neurol Med Chir (Tokyo). 2008; 48:49–55. discussion 55-56. PMID: 18296872.

20. Nedeltchev K, Brekenfeld C, Remonda L, Ozdoba C, Do DD, Arnold M, et al. Internal carotid artery stent implantation in 25 patients with acute stroke : preliminary results. Radiology. 2005; 237:1029–1037. PMID: 16237137.

21. Papanagiotou P, Roth C, Walter S, Behnke S, Grunwald IQ, Viera J, et al. Carotid artery stenting in acute stroke. J Am Coll Cardiol. 2011; 58:2363–2369. PMID: 22115640.

22. Powers WJ, Clarke WR, Grubb RL Jr, Videen TO, Adams HP Jr, Derdeyn CP. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia : the Carotid Occlusion Surgery Study randomized trial. JAMA. 2011; 306:1983–1992. PMID: 22068990.

23. Qureshi AI. Endovascular revascularization of symptomatic acute extracranial internal carotid artery occlusion. Stroke. 2005; 36:2335–2336. PMID: 16239628.

24. Qureshi AI, Luft AR, Sharma M, Guterman LR, Hopkins LN. Prevention and treatment of thromboembolic and ischemic complications associated with endovascular procedures : Part II--Clinical aspects and recommendations. Neurosurgery. 2000; 46:1360–1375. PMID: 10834641.
25. Randomised trial of endarterectomy for recently symptomatic carotid stenosis : final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998; 351:1379–1387. discussion 1375-1376. PMID: 9593407.
26. Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J, et al. Tandem internal carotid artery/middle cerebral artery occlusion : an independent predictor of poor outcome after systemic thrombolysis. Stroke. 2006; 37:2301–2305. PMID: 16888266.

27. Shawl FA. Emergency percutaneous carotid stenting during stroke. Lancet. 1995; 346:1223. PMID: 7475670.

28. Stampfl S, Ringleb PA, Möhlenbruch M, Hametner C, Herweh C, Pham M, et al. Emergency cervical internal carotid artery stenting in combination with intracranial thrombectomy in acute stroke. AJNR Am J Neuroradiol. 2014; 35:741–746. PMID: 24157733.

29. Wholey MH, Wholey M, Mathias K, Roubin GS, Diethrich EB, Henry M, et al. Global experience in cervical carotid artery stent placement. Catheter Cardiovasc Interv. 2000; 50:160–167. PMID: 10842380.

30. Zaidat OO, Alexander MJ, Suarez JI, Tarr RW, Selman WR, Enterline DS, et al. Early carotid artery stenting and angioplasty in patients with acute ischemic stroke. Neurosurgery. 2004; 55:1237–1242. discussion 1242-1243. PMID: 15574205.

31. Zhu MM, Feit A, Chadow H, Alam M, Kwan T, Clark LT. Primary stent implantation compared with primary balloon angioplasty for acute myocardial infarction : a meta-analysis of randomized clinical trials. Am J Cardiol. 2001; 88:297–301. PMID: 11472712.

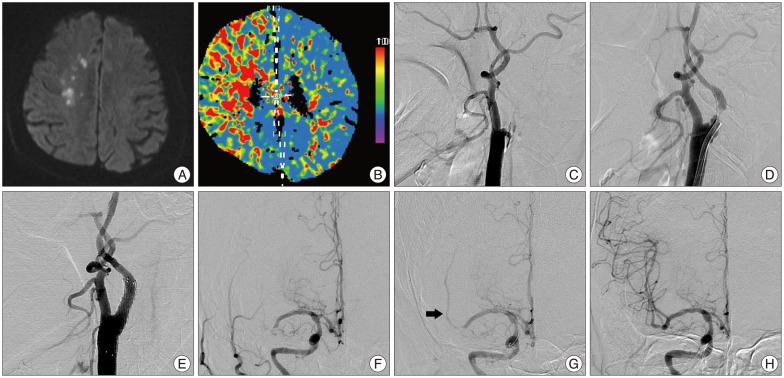
Fig. 1
Patient 4. Acute cervical internal carotid artery (ICA) occlusion without intracranial tandem occlusion. A : Initial diffusion-weighted image reveal small infarction areas in the right hemisphere. B : Computed tomography perfusion scan with mean transit time obtained before intervention. There is significant hypoperfusion of the entire right middle cerebral artery (MCA) territory, indicating widespread mismatch. C : Diagnostic angiography shows complete occlusion of the right cervical ICA. D and E : Anteroposterior and lateral views of the right ICA angiogram show that the intracranial segment of the right ICA and MCA is visualized with poor contrast via the collateral vessels of the external carotid artery and the ophthalmic artery (arrowheads). F : There is no collateralization of the right MCA territory via the left ICA. G : After passing the ICA occlusion using a 0.014-inch microwire, partial recanalization of the ICA showing a high-grade arteriosclerotic stenosis. H : Unsubtracted images acquired immediately after stent deployment show recanalization and residual stenosis. I : After balloon angioplasty, normal ICA outflow is visible. J : Intracranial control angiogram shows normal flow in the intracranial ICA and MCA.

Fig. 2
Patient 8. Acute cervical internal carotid artery (ICA) occlusion with intracranial tandem occlusion. A and B : Initial images demonstrate widespread mismatch between extent of lesion on diffusion-weighted image (A) and computed tomography perfusion scan with mean transit time (B). C : Diagnostic angiography shows acute occlusion just beyond the origin of the right ICA. D : After passing the ICA occlusion using a 0.014-inch microwire, partial recanalization of the ICA showing a high-grade arteriosclerotic stenosis. E : After stent placement and balloon angioplasty, normal ICA outflow is visible. F : There is an additional distal M1 occlusion in the anteroposterior view of the right ICA angiogram. G : Digital subtraction angiogram after deployment of the Solitaire stent shows partial restoration of vessel flow; distal stent markers (arrow) are visible. H : After stent withdrawal, the vessel is fully recanalized to a Thrombolysis In Cerebral Infarction 3 state.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download