Abstract
A case of total spondyloptosis of the cervical spine at C6-7 level with cord compression is described in a 51-year-old male. Because the bodies of C6 and 7 were tightly locked together, cervical traction failed. Then the patient was operated on by a posterior approach. Posterior stabilization and fusion were performed by C4-5 lateral mass and C7-T1 pedicle screw fixation and rod instrumentation with bridging both C4-5's rods to the C7-T1's extended ones. After C6 total laminectomy and foraminotomy, the C6 body was returned to its proper position. Secondly, anterior stabilization and fusion were performed by C6-7 discectomy with a screw-plate system. A postoperative lateral plain radiograph showed good realignment. In this case, we report the clinical presentation and discuss the surgical modalities of C6-7 total spondyloptosis and the failed close reduction.
Traumatic cervical spondyloptosis is a less common injury than lumbar spondyloptosis, and only a few cases have been reported in the literature9,11). Patients usually have complete and irreversible cervical cord injury. Regardless of whether there is a neurologic deficit or not, closed and open reduction and stabilization of the fracture-dislocation are performed mainly in cervical sponyloptosis4). And, a combined anterior and posterior fusion and fixation is preferred for this unstable injury2,9). We present a case of traumatic spondyloptosis of C6-7 with bipedicular fracture of C6 with cord compression. In this case, we discuss the preoperative closed reduction and surgical management modalities.
A 51-year-old male patient was transferred to our clinic's emergency department from a local clinic after a vehicle accident 9 days ago. The patient was drowsy due to cerebral traumatic subarachnoid hemorrhage and minimal subtentorial hemorrhage, seen on the brain computerized tomography scans, and he was intubated. He suffered from severe neck pain and headache. Physical examination revealed that quadriparesis as Medical Research Council (MRC) power grade 1/5. We found hypoesthesia at the C7 level and below, spinal cord injury signs such as spasticity, extensor plantar reflexes, bilateral Hoffman's sign and ankle clonus. The deep tendon reflexes were hyperactive. A plain radiograph and computerized tomography (CT) imaging showed complete C6-7 spondyloptosis and facet dislocation and bipedicular fracture (Fig. 1). The posterior margin of the C6 body was placed at the mid-portion on the anterior margin of C7 body and they were tightly locked to each other. Cervical magnetic resonance imaging (MRI) showed cord's displacement and signal change. The adjacent tissues' high signal intensity was also observed (Fig. 2). Cervical traction was applied for 9 days at the local clinic. Despite the cervical traction applied for 9 days, a comparison of a cervical plain radiograph, before and after traction, showed that there was no significant difference. Somatosensory and motor evoked potentials indicated central sensory and motor conduction pathway defects of both the upper and lower extremities. Electromyography was not attempted, because of mental deterioration.
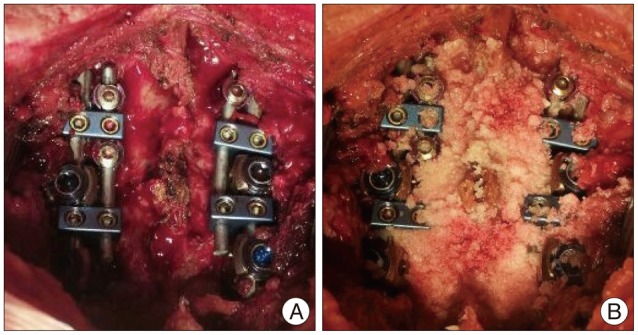
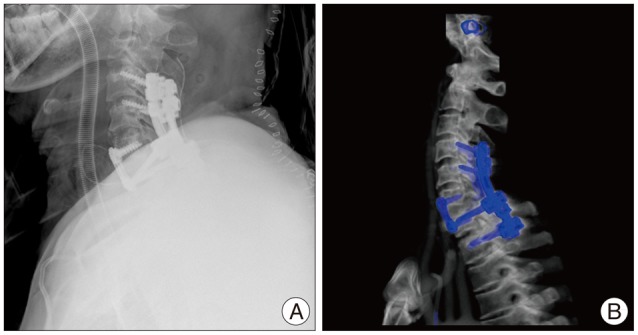
First, we performed a closed reduction, using Gardner-Wells skeleton traction, with 20 lb. But, the C6 body did not move at all, as seen on the cervical plain radiograph, and the cervical cord was still displaced. Because of patient's skull fractures and mental deterioration, Gardner-Wells skeletal traction was hard to keep long. So, we considered performing surgical management that included open reduction and stabilization for the C6-7 spondyloptosis. The patient was initially operated on by the posterior approach. After dissecting the interspinous ligament, we found that the right inferior articular facet and lamina were fracture-dislocated. The posterior stabilization was performed from C4 to T1 by a C4-5 lateral mass and C7-T1 pedicle screw fixation and rod instrumentation (Fig. 3). After the posterior approach, we checked the plain radiography, but the reduction was insufficient. Additional anterior decompression and fusion was achieved by C6-7 discectomy with autologus pelvic bone graft and screw-plate fixation. The anterior and posterior longitudinal ligaments were torn and some free fragments of the disrupted disc compressed spinal cord. A postoperative cervical plain radiography and CT imaging showed good realignment (Fig. 4). Postoperatively, the patient's weakness mildly improved (MRC power grade 2/5), except for finger and wrist flexion and extension. Touch sensation below the C7 sensory dermatome was still decreased, and the pathologic reflexes remained, too. But the neck pain was relieved, and the oro-tracheal tube was removed. Rigid cervical orthosis (Philadelphia cervical collar) was applied for neck immobilization. After surgery, he received rehabilitation treatment for several months. Postoperative follow up neurologic examination after 3 months showed that both upper extremities' motor power was gained as MRC power grade 3/5.
Spondyloptosis is a term for spinal dislocation or Grade V spondylolisthesis, in which one vertebral body is lodged in the anterior or posterior space of the other one9,10). It is more common in the lumbar spine than in the cervical spine, and can be seen following birth trauma3), and congenital conditions2,13) of the cervical spine like absent cervical pedicles, corticated defect in pars interarticularis and neoplastic diseases7) like neurofibromatosis or aneurysmal bone cyst and after vehicle or diving trauma1). It is usually associated with complete cord injury due to cracking of the cord between the arch of the superior vertebra and the posterior surface of the vertebral body below.
The main injury mechanism in our case was hyperflexion-compression. Trauma resulted in crushing of the spinal cord, which led to quadriparesis. Anterior and posterior longitudinal ligaments and bony structures, as well as the intervertebral disc were disrupted, and the physiologic alignment was disturbed.
Generally, a posterior element fracture leads to a spontaneous posterior decompression of the spinal canal and this can preserve the cord by the cord moving posteriorly9). So, severe neurologic deficits are rare in fracture of the posterior elements. But in our patient's case, initial cervical MRI showed diffuse cord signal change in the C4-7 segments. This could have led to severe irreversible neurologic deficits despite spontaneous posterior decompression.
For the stabilization, closed reduction using Gardner-Wells skeleton traction was used with 20 lb. Menku et al.11) suggested that retropulsion of the disc into the spinal canal during traction could compress the spinal cord and worsen the neurologic deficit. On the other hand, some reported that a fracture of the posterior structures decompresses the spinal canal and allows for cervical traction to be safely implemented in spondyloptosis patients15).
The patient's cervical plain radiography showed no reduction compared with before the traction. Despite cervical traction and Gardner-Wells skeletal traction being applied for several days, reduction was not been. Because of patient's skull fractures and irritable mental state, Gardner-Wells skeletal traction was less effective and had possibility to worse skull fracture. So, we decided to perform surgical treatment for reduction, stabilization, and realignment.
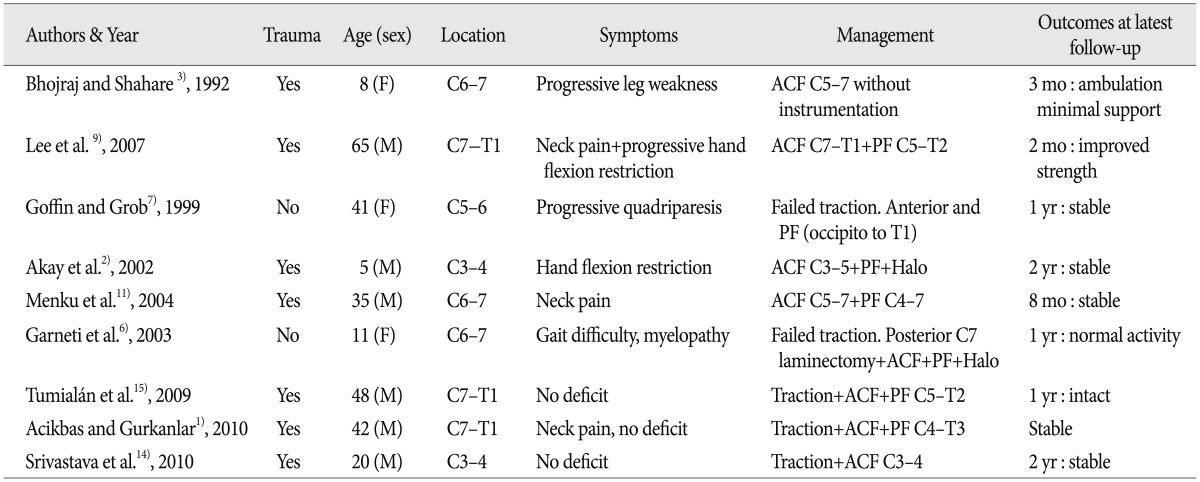
Surgical management can be performed with either an anterior, posterior or combined surgical approach (Table 1).
An anterior and posterior fusion is the standard management2,9), due to greater realignment and stabilization being achieved in unstable injuries, with all ligamentous structures involving the three columns. But some studies reported that closed reduction followed by limited anterior-only fusion supplemented by rigid postoperative immobilization is more safe and effective than combined fusion3) because the fracture of the adjacent vertebrae may affect the treatment strategy. But Ozdogan et al.12) reported that there is a possible risk of graft dislodgment if the initial operation is done anteriorly.
Because the tightly locked vertebrae induced failure of the attempted closed reduction, we selected the posterior approach. We thought that the removal of the fracture fragments and correction of the spinal instability by the posterior approach was more safe and effective in this patient. For avoiding additional cord injury in the surgical field, the C4-5 lateral mass and C7-T1 pedicle screw fixation and rod instrumentation were performed carefully. After C6 laminectomy and foraminotomy, the C6 body returned to its proper position and the snapped cervical cord was released. For spinal stability and preserving the normal cervical lordotic curve, we bridged both C4-5's rods to the C7-T1's extended ones. In some biochemical studies, pedicle screw-rod constructs are superior to the lateral mass screw-rod construct in sharing axial loads5). Johnston et al.8) reported that cervical pedicle screws have higher pullout strength and loosened less than lateral mass screws.
Despite performing posterior decompression and fixation, the realignment was not enough. The ruptured C6-7 intervertebral disc was viewed on the patient's cervical MRI, and the C6-7 body structure was still compressing the spinal cord. So, we performed anterior decompression and fixation using screw-plate fixation. Postoperative imaging showed good realignment. Menku et al.11) also reported that three-dimensional fixations for the cervical spine using the lateral mass and transpedicular screw fixation with an anterior cervical plate offered increased stability.
In the presented case, we performed decompression and stabilization by the anterior and posterior approach immediately. Because closed reduction with cervical and Gardner-Wells skeleton traction were failed, we did not need to maintain the traction system. Also, our case was an unstable injury by complete disruptions of all ligamentous. Therefore, realignment and stabilization of the cervical spine by immediate surgery were more effective.
Reduction and stabilization are the standard treatment in cervical spondyloptosis. If closed reduction fails, regardless of the neurologic deficit, early surgical decompression and stabilization should be considered. The neurologic status and radiologic imaging results are important considerations when selecting the surgical approach. Also, it is important that decompression and fixation be performed carefully until the realignment is correct. We hope that more studies of variable spondyloptosis will be reported for good outcomes.
References
1. Acikbas C, Gurkanlar D. Post-traumatic C7-T1 Spondyloptosis in a patient without neurological deficit : a case report. Turk Neurosurg. 2010; 20:257–260. PMID: 20401855.
2. Akay KM, Ersahin Y, Tabur E. Cervical spondyloptosis : a case report. Minim Invasive Neurosurg. 2002; 45:169–172. PMID: 12353166.
3. Bhojraj SY, Shahane SM. Posttraumatic cervical spondyloptosis at C6-7 with late-onset cord compression : a new clinical entity. Case report. J Neurosurg. 1992; 77:792–794. PMID: 1403125.

4. Dahdaleh NS, Dlouhy BJ, Greenlee JD, Smoker WR, Hitchon PW. An algorithm for the management of posttraumatic cervical spondyloptosis. J Clin Neurosci. 2013; 20:951–957. PMID: 23702373.

5. Dunlap BJ, Karaikovic EE, Park HS, Sokolowski MJ, Zhang LQ. Load sharing properties of cervical pedicle screw-rod constructs versus lateral mass screw-rod constructs. Eur Spine J. 2010; 19:803–808. PMID: 20119837.

6. Garneti N, Dunn D, El Gamal E, Williams DA, Nelson IW, Sandemon DR. Cervical spondyloptosis caused by an aneurysmal bone cyst : a case report. Spine (Phila Pa 1976). 2003; 28:E68–E70. PMID: 12590221.
7. Goffin J, Grob D. Spondyloptosis of the cervical spine in neurofibromatosis. A case report. Spine (Phila Pa 1976). 24:1999; 587–590. PMID: 10101826.
8. Johnston TL, Karaikovic EE, Lautenschlager EP, Marcu D. Cervical pedicle screws vs. lateral mass screws : uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006; 6:667–672. PMID: 17088197.

9. Lee DG, Hwang SH, Lee CH, Kang DH. Clinical experience of traumatic C7-T1 spondyloptosis. J Korean Neurosurg Soc. 2007; 41:127–129.
10. Mamindla RK, Kumar A, Bhattacharjee S, Sahu BP. A novel case of "ambulatory" cervical spondyloptosis : case report with literature review. Eur Spine J. 2014; 23(Suppl 2):161–166. PMID: 23708939.

11. Menku A, Kurtsoy A, Tucer B, Oktem IS, Akdemir H. The surgical management of traumatic C6-C7 spondyloptosis in a patient without neurological deficits. Minim Invasive Neurosurg. 2004; 47:242–244. PMID: 15346323.

12. Ozdogan C, Gogusgeren MA, Dosoglu M. Posttraumatic cervical spondyloptosis 'Case Report'. Turk J Trauma Emerg Surg. 1999; 5:46–48.
13. Song KC, Cho KS, Lee SB. Congenital defect of the posterior arch of cervical spine : report of three cases and review of the current literature. J Korean Neurosurg Soc. 2010; 48:294–297. PMID: 21082064.

14. Srivastava SK, Agrawal KM, Sharma AK, Agrawal MD, Bhosale SK, Renganathan SR. C3-C4 spondyloptosis without neurological deficit-a case report. Spine J. 2010; 10:e16–e20. PMID: 20620981.

15. Tumialán LM, Dadashev V, Laborde DV, Gupta SK. Management of traumatic cervical spondyloptosis in a neurologically intact patient : case report. Spine (Phila Pa 1976). 2009; 34:E703–E708. PMID: 19730203.
Fig. 1
A : Saggital computed tomography imaging reveals spondyloptosis at the C6-7 level. B : The vertebrae are locked to each other at axial view.
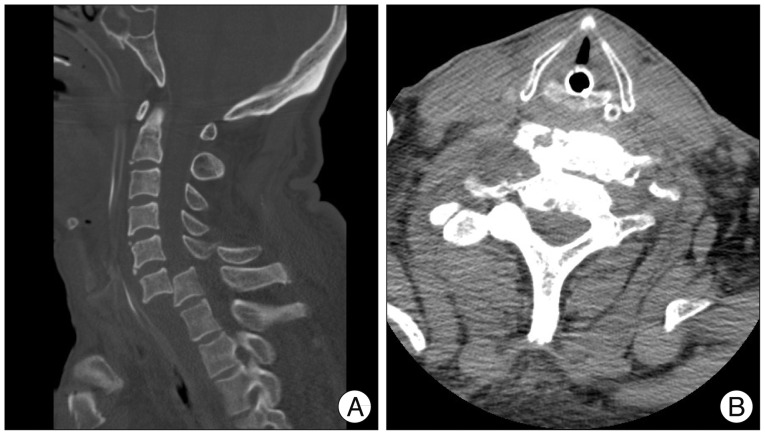
Fig. 2
Axial T2-weighted (A), saggital T2-weighted (B) magnetic resonance imaging of the cervical reveals cord dis-placement and signal change, and high signal intensity of the adjacent tissues.
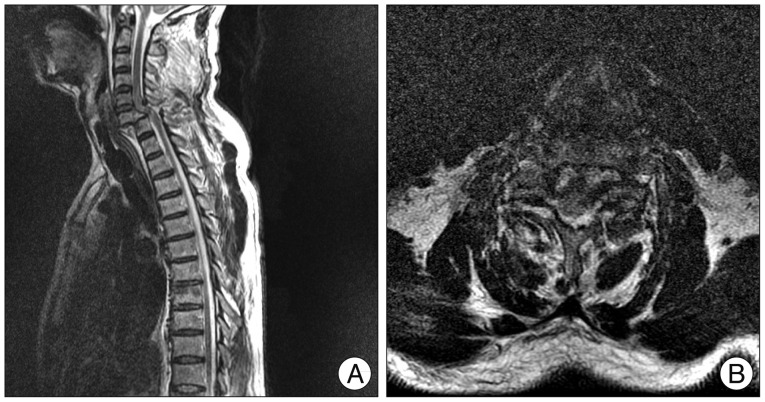
Fig. 3
The posterior stabilization was performed from C4 to T1 by a C4-5 lateral mass and C7-T1 pedicle screw fixation and rod instrumentation with posterior decompression (A) and autologous bone fusion (B).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download