Abstract
Objective
The purpose of this study was to compare the radiological and neurological outcomes between two atlantoaxial fusion method for atlantoaxial stabilization; C1 lateral mass-C2 pedicle screws (screw-rod constructs, SRC) versus C1-2 transarticular screws (TAS).
Methods
Forty-one patients in whom atlantoaxial instability was treated with atlantoaxial fixation by SRC group (27 patients, from March 2005 to May 2011) or TAS group (14 patients, from May 2000 to December 2005) were retrospectively reviewed. Numeric rating scale (NRS) for pain assessment, Oswestry disability index (ODI), and Frankel grade were also checked for neurological outcome. In radiologic outcome assessment, proper screw position and fusion rate were checked. Perioperative parameters such as blood loss during operation, operation time, and radiation exposure time were also reviewed.
Results
The improvement of NRS and ODI were not different between both groups significantly. Good to excellent response in Frankel grade is shown similarly in both groups. Proper screw position and fusion rate were also observed similarly between two groups. Total bleeding amount during operation is lesser in SRC group than TAS group, but not significantly (p=0.06). Operation time and X-ray exposure time were shorter in SRC group than in TAS group (all p<0.001).
C1-2 instability caused by trauma, tumors, congenital or inflammatory conditions is highly dangerous condition and was required fixation instantly to keep stability, and prevent neurological compromise. There are various surgical techniques to treat atlantoaxial instability. Traditionally, posterior wiring technique was introduced by Gallie or Brooks-Jenkins and used to stabilize C1-2 complex. The patients operated by posterior wiring technique have to keep external orthosis after operation, and reported a fair number of neurovascular complication related operation. Posterior atlantoaxial transarticular screw fixation was introduced by Magerl and Seemann in 198616). This technique provides over 90 percent high arthrodesis rate, immediate biomechanical stability to the atlantoaxial complex and not need to keep postoperative external orthosis4,6,10,14,18). However, this technique is technically demanding14). About 20% of patients have anomalous high-riding vertebral artery, which is risky from C1-2 transarticular screws10,11). This method is also contraindicated in patients with damage to the posterior column and a fixed severe anterior dislocation of the atlas15).
Goel and Laheri9) have been introduced C1 lateral mass and C2 pedicle screw, and Harms and Melcher11) have been modified C1 lateral mass and C2 pedicle screw fixation. These techniques have been used popularly by many surgeons to stabilize C1-2 complex.
The aim of this study was to compare the clinical and radiological results between transarticular screw and screw-rod systems based on the data of at least two years follow up patients with atlantoaxial fusion consecutively performed by one surgeon.
This study is a retrospective, single-institute investigation of two fixation technique : C1 lateral mass-C2 pedicle screws (screw-rod constructs, SRC) or C1-2 transarticular screws (TAS) to treat atlantoaxial instability by one surgeon. 41 who presented to single university hospital from May 2000 to May 2011 with atlantoaxial instabilities resistant to conservative treatment and with no history of prior cervical surgery were included. Patients with trauma, infection or neoplasm were excluded. Fourteen patients (8 males and 6 females) were treated with combination TAS fixation and/or posterior wiring from May 2000 to December 2005. 27 patients (14 males and 13 females) were treated with atlantoaxial fixation by SRC fixation from March 2005 to May 2010. Patient information was summarized in Table 1. In SRC group, 13 of 27 patients were C1-2 instability. In TAS group, 5 of 14 patients were C1-2 instability. Diagnosis of patients was summarized in Table 2. The mean follow-up period was 44.1 months (range of 24-84 months) for TAS group and 35.3 months (range of 24-44 months) for SRC group, respectively. The mean age was 51.9 years (range of 35-72 years) in TAS and 48.7 years (range of 32-67 years) in SRC group, respectively.
Under general anesthesia, the patient was placed in the prone position. The head was held in a slightly flexed position using a Mayfield head holder. Lateral radiography was used to confirm atlantoaxial reduction. Any adjustments to the head position were made before preparation and draping of the neck and bone graft donor site. Subperiosteal exposure of C1 and C2 was performed using a usual manner. When transarticular screw fixation was undertaken, the C3 lamina and C2-3 facet joint was exposed to allow selection of the correct screw entry point and, superficially, the dissection was carried out distally to the C7 spinous process to allow the correct angular positioning for drilling through the C1 and C2 lateral masses. The relationship between C1 and C2 was visualized on fluoroscopy and corrected by direct control of the posterior arch of C1 and the spinous process of C2 using a towel clip. The entry point was 2 to 3 mm lateral and above the medial edge of the C2-3 facet. The medial arch of the C2 lamina was exposed subperiosteally and used as a landmark for the drill direction. Using fluoroscopy, K-wire was inserted into the dorsal aspect of the axis at the junction of the lamina with the articular mass strictly in the sagittal plane. Both screws were placed toward the dorsal cortex of C1 with 10 degree medial direction. After satisfactory positioning was achieved a cannulated drill 2.5 mm in diameter was passed over the K-wire and aimed at the top of the tubercle of the anterior arch of the atlas. The drill crosses the isthmic part of C2 and exits the axis in the posterior third of the atlantoaxial joint. After crossing the joint, the drill enters the atlas approximately in the middle portion of the articular process. The drill was left in place until the second drill hole has been made and the corresponding screw has been inserted. A 3.5-mm cortical screw was used originally, whereas lag screws are now available. After screw positioning, bicortical interspinous autograft from iliac bone was performed. The operation time, blood loss and intraoperative complication were checked.
All patients were placed in a prone position under general anesthesia. The neck was fixed with a Mayfield head frame in a flexed and functional position at the craniovertebral junction. After the suboccipital and posterior cervical regions were prepared, a posterior incision in the midline was made from the inion to the third cervical vertebra. We proceeded carefully, exposing the posterior elements of occiput to C3 and taking care to avoid damage to the vertebral artery laterally and the structures inside the spinal canal. Depression of the posterior fossa was established by posterior excision of parts of the posterior atlantal arch (1.5 cm) and the posterior border of the foramen magnum (1.5 cm). Following the procedure, internal fixation between the lateral mass of the atlas and the C2 pedicle was employed (C1-2 SRC). The entry point of atlas is the mid-portion of the lateral mass of C1. The entry angulation is directed between 0 to 10 degrees to medial direction toward the anterior tubercle of C1. The entry point of axis is the inferior mid-portion of the facet joint and directed to 20-30 degrees to medial and superior direction. Two 3.5 mm polyaxial screws were then inserted bilaterally in a cranial and ventral direction. The insertions of the polyaxial screws were aided by fluoroscopy guidance. The atlas displacement was repositioned by pushing the spinous process of the axis in a ventral and caudal direction by using the screw-rod systems, followed by fixation to the rods to maintain alignment.
The repositioning of the atlanto-axial dislocation was performed under the intraoperative monitoring of somatosensory evoked potential (SEP) of the upper extremities. Patients with non-changed or improved SEP (decrease of latency and/or elevated amplitude) were considered to have no additive neurological deficit. For the bone fusion, DBM with local bone from C2 spinous process was grafted around C1-2 facet space after decortication. The operation time, blood loss and intraoperative complication were also checked.
Clinical outcome measurement and radiological outcome of both groups were evaluated and compared at 1, 3, 6, 12, and 24 months after surgery. Clinical outcome measurement include in numeric rating scale (NRS), Oswestry disability index (ODI; the question about sex life was not included) for functional outcome and Frankel grade. Successful pain relief was described as a 50% or more reduction in NRS score, and good or excellent results in Frankel grade were considered to be reflective of 'good' outcomes. Differences before surgery and at final follow-up were evaluated. Perioperative parameters between two groups were compared such as blood loss during operation, operation time and radiation exposure time.
The plain anterior-posterior, lateral cervical spine dynamic radiographs and CT scans with sagittal and coronal reconstruction were performed after surgery to evaluate fusion. Solid fusion was defined by lesser than 2 mm of motion between the segments on the dynamic lateral radiographs and over 60% bony trabecular bridge between the C1 or C2 lamina and grafted bone on sagittal reconstructed CT.
Screw malposition such as medial invasion or vertebral artery invasion was defined as perforating of 50% or more of the screw diameter. Screw malposition whether symptomatic or not, screw breakage, and fusion rate were checked.
Statistical analysis was performed using SPSS version 13.0 (SPSS Inc., Chicago, IL, USA). Data are presented as the mean±SD. Student's t-test and chi-square test were used to assess statistical significance of the changes in clinical and radiological outcome between two groups. Paired t-test was used to compare outcomes before surgery and at final follow-up. A p-value<0.05 was regarded as statistically significant.
NRS was improved from 6.8 to 4.5 in the TAS group and from 7.6 to 3.2 in SRC group on the average, respectively. ODI was also improved in both groups from 59.8% to 15.4% in TAS group and from 51.5% to 17.6% in SRC group, respectively. The Frankel grades were improved in 4 of 12 cases (33.3%) with preoperative neurological deficit in SRC group, and 3 of 7 cases (42.9%) in TAS group (p=0.678). Good or excellent response in clinical outcome is similar in both group, 11 of 14 TAS group (78.6%) and 22 of 27 SRC group (81.5%) (p=0.889). All clinical outcomes were statistically significantly improved from initial to final follow-up, and there was no definite difference between two groups (Table 3). The perioperative parameters between two groups were introduced in Table 4. The intraoperative blood loss were estimated more in TAS group compared to SRC group, but it was statistically not significant (p=0.065). The operation time and radiation exposure time were increased in TAS group than SRC group significantly (p=0.013 and p<0.001) (Fig. 1, 2 and 3).
The overall fusion rate was 85.7% as 12 of 14 patients in TAS group, and 88.9% as 24 of 27 patients in SRC group. There was no statistical difference in overall fusion rate between two groups (p=0.768). The proper positions of screws were observed in 10 patients in TAS group (71.4%) and 20 patients in SRC group (74.0%) (p=0.564). Unfortunately C1 medial invasion, vertebral artery foramen invasion and screw fracture were observed in both groups. The comparisons of screw position were no statistically different between two groups and summarized in Table 5.
The anatomic shape of atlantoaxial segment was shown complex, and surgical attempts to achieve stabilization in case of atlantoaxial instability must address challenge. Traditionally, posterior wiring stabilization and structural bone grafting used to treat atlantoaxial instability1,7). These surgical methods do not provide appropriate stability, which results in union rate about 70%, and additional external stabilization during the immediate postoperative period is required2,3,17,19). Moreover, the subluminal passage of wires can produce irreversible and critical neurovascular injuries4).
Magerl and Seemann16) introduced the technique of C1-2 transarticular screw fixation as an alternative surgical treatment for patients with atlantoaxial instability. Transarticular screw fixation could provide immediate multidirectional stability and the success rate of bony fusion is about 90%. However, there are some drawbacks10,11,15,18,20). Approximately, 20% of patients have aberrant path of vertebral artery which is risk of vertebral artery injury during placement of screws, and also learning curve to train this technique is stiff. There is need for flexion of the patient's neck during procedure to obtain the proper trajectory, which cause hypoglossal nerve injury. Intraoperative reduction is not possible with this technique. Transarticualr screw technique requires preliminary reduction of C1 on C2 before screw placement.
Goel and Laheri9) described atlantoaxial fixation technique using the C1 lateral mass-C2 pedicle screw fixation, which performed in 30 cases in 1994. The result of fusion rate was 100%. Harms and Melcher11) introduced a modification of this technique11). They managed to achieve C1-2 bony fusion in almost 100% of cases. Biomechanically, the overall rigidity achieved using the C1 lateral mass and C2 pedicle screws is similar to that achieved with transarticular screws, but the use of C1 lateral mass and C2 pedicle screws makes to achieve statistically greater axial rotation21). Neither Harms and Melcher nor Goel recorded damage to the vertebral artery or spinal cord following their methods of screw insertion. This technique has many advantages : reduction of an atlantoaxial dislocation can be done through atlas manipulation; immediate rigid fixation, which can affect normal neck movement, can be achieved with less segment fusion; and a fractured lateral mass can be fixed directly using C1 posterior lateral mass screws8). The size of the lateral mass of the C1 is considerably larger and stronger than any other lateral mass of vertebra in the rest of the spine and is sufficient to safely place the longer screws.
In this study, we compared the clinical and radiological results between transarticular screw and screw-rod systems based on the data of at least 2 years long-term follow up patients with atlantoaxial fusion consecutively performed by one surgeon. Result shows there are no difference of fusion rate between two groups and also statistically no significance in neurovascular complication. The only more frequent complication, such as bleeding from the venous plexus around the greater occipical nerve, we now treat by a prompt insertion of the polyaxial screw into the C1 lateral mass and by tamponade. In most patients of our study, the complaints related with screw malposition including medial invasion of screws were subsided spontaneously.
In the present study, the success rate of bony fusion of the Magerl transarticular techniques showed approximately 90% whereas Goel et al. and Harms and Melcher showed 100% of fusion rate using C1 lateral mass-C2 pedicle screw techniques8,9,22). Relative lower fusion rate compared to that of other papers might be caused by using DBM with local bone instead of iliac bone for avoiding donor site pain. Although considering the usage of iliac bone in group of transarticular screw fixation, fusion rate of C1 lateral-C2 pedicle screw group is relatively favorable. Pedicle screws require less extensive skin incisions are applicable to obese or kyphotic patients, and provide longer screw purchase12).
In this study, perioperative pain, satisfaction after treatment were also showed insignificantly different between two groups. Volume of bleeding during operation is smaller in C1 lateral mass-C2 pedicle screw fixation than transarticular screw fixation, but not significant. But, operation time and radiation exposure time due to C-arm is shorter in C1 lateral mass-C2 pedicle screw fixation than transarticular screw fixation significantly. It might be caused by technical difficulties during surgical exposure, which is wider in transarticular screw fixation than C1 lateral mass-C2 pedicle screw fixation, for screw trajectory. Consideration of anatomical relation nearby screw position, such as anomalous course of vertebral artery might be also one of the reasons. And because C1 lateral mass-C2 pedicle screw fixation was performed later than transarticular screw fixation, the surgeon had learned more surgical experience in this regard, and this makes shorter operation time and radiation exposure time in C1 lateral mass-C2 pedicle screw fixation.
Lee et al.13) recently reported the experience of C1 lateral mass-C2 pedicle screws with a polyaxial screw-rod system and posterior C1-2 transarticular screw fixation. This study is only one report that compared the operation time and blood loss between two operation techniques5). The mean operation time and the amount of intraoperative blood loss were 176 min and 360 mL in C1-2 transarticular screw fixation group and 169 min and 730 mL in C1 lateral mass-C2 pedicle screws group, respectively. Although it seems that the operation time is similar between two groups and blood loss is lesser in C1-2 transarticular screw fixation, statistical significance was not assessed and the operators are different between two groups. Authors have indicated that the operation time, which was initially longer than that for the Magerl technique, gradually decreased to between 90 minutes and 120 minutes.
This study has some limitations. Result of the operation might have been changed depending on preference or familiarity of surgeon in surgical method whether transarticular or C1 lateral mass-C2 pedicle screw. Our study is retrospective and the patient sample size was not large. Therefore, further more consecutive data and future prospective clinical studies will be needed to determine more definite conclusion.
Both C1-2 transarticular screws and C1 lateral mass-C2 pedicle screws could be selected as safe and effective treatment options for C1-2 instability. But the perioperative result, which is technical demanding and X-ray exposure might be expected better in C1 lateral mass-C2 pedicle screw group compared to transarticular screw group.
References
1. Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978; 60:279–284. PMID: 348703.

2. Coyne TJ, Fehlings MG, Wallace MC, Bernstein M, Tator CH. C1-C2 posterior cervical fusion : long-term evaluation of results and efficacy. Neurosurgery. 1995; 37:688–692. discussion 692-693. PMID: 8559297.
3. Dickman CA, Crawford NR, Paramore CG. Biomechanical characteristics of C1-2 cable fixations. J Neurosurg. 1996; 85:316–322. PMID: 8755762.

4. Dickman CA, Sonntag VK. Posterior C1-C2 transarticular screw fixation for atlantoaxial arthrodesis. Neurosurgery. 1998; 43:275–280. discussion 280-281. PMID: 9696080.

5. Elliott RE, Tanweer O, Boah A, Morsi A, Ma T, Frempong-Boadu A, et al. Outcome comparison of atlantoaxial fusion with transarticular screws and screw-rod constructs : meta-analysis and review of literature. J Spinal Disord Tech. 2014; 27:11–28. PMID: 23128387.

6. Farey ID, Nadkarni S, Smith N. Modified Gallie technique versus transarticular screw fixation in C1-C2 fusion. Clin Orthop Relat Res. 1999; (359):126–135. PMID: 10078135.

8. Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method : a report of 160 treated patients. Neurosurgery. 2002; 51:1351–1356. discussion 1356-1357. PMID: 12445339.

9. Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien). 1994; 129:47–53. PMID: 7998495.

10. Haid RW Jr, Subach BR, McLaughlin MR, Rodts GE Jr, Wahlig JB Jr. C1-C2 transarticular screw fixation for atlantoaxial instability : a 6-year experience. Neurosurgery. 2001; 49:65–68. discussion 69-70. PMID: 11440461.

11. Harms J, Melcher P. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine. 2001; 26:2467–2471. PMID: 11707712.

12. Jeon SW, Jeong JH, Choi GH, Moon SM, Hwang HS, Choi SK. Clinical outcome of posterior fixation of the C1 lateral mass and C2 pedicle by polyaxial screw and rod. Clin Neurol Neurosurg. 2012; 114:539–544. PMID: 22130046.

13. Lee SH, Kim ES, Sung JK, Park YM, Eoh W. Clinical and radiological comparison of treatment of atlantoaxial instability by posterior C1-C2 transarticular screw fixation or C1 lateral mass-C2 pedicle screw fixation. J Clin Neurosci. 2010; 17:886–892. PMID: 20399666.

14. Low HL, Redfern RM. C1-C2 transarticular screw fixation for atlantoaxial instability : a 6-year experience, and C1-C2 transarticular screw fixation-technical aspects. Neurosurgery. 2002; 50:1165–1166. author reply 1166. PMID: 11987276.

15. Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997; 86:961–968. PMID: 9171174.

16. Magerl F, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In : Kehr P, Weidner A, editors. Cervical Spine I. Vienna: Springer-Verlag;1987. p. 322–327.
17. Papagelopoulos PJ, Currier BL, Hokari Y, Neale PG, Zhao C, Berglund LJ, et al. Biomechanical comparison of C1-C2 posterior arthrodesis techniques. Spine (Phila Pa 1976). 2007; 32:E363–E370. PMID: 17545899.

18. Paramore CG, Dickman CA, Sonntag VK. The anatomical suitability of the C1-2 complex for transarticular screw fixation. J Neurosurg. 1996; 85:221–224. PMID: 8755749.

19. Reilly TM, Sasso RC, Hall PV. Atlantoaxial stabilization : clinical comparison of posterior cervical wiring technique with transarticular screw fixation. J Spinal Disord Tech. 2003; 16:248–253. PMID: 12792338.

20. Solanki GA, Crockard HA. Peroperative determination of safe superior transarticular screw trajectory through the lateral mass. Spine (Phila Pa 1976). 1999; 24:1477–1482. PMID: 10423794.

21. Xie Y, Li Z, Tang H, Li M, Guan Z. Posterior C1 lateral mass and C2 pedicle screw internal fixation for atlantoaxial instability. J Clin Neurosci. 2009; 16:1592–1594. PMID: 19796950.

22. Yeom JS, Buchowski JM, Kim HJ, Chang BS, Lee CK, Riew KD. Risk of vertebral artery injury : comparison between C1-C2 transarticular and C2 pedicle screws. Spine J. 2013; 13:775–785. PMID: 23684237.

Fig. 1
Lateral plain radiographs of a 65-year-old female showing. A : The severely dislocated atlas and axis caused by complication of rheumatoid arthritis. B : Reduction and screw positioning of the C1-2 complex postoperatively.
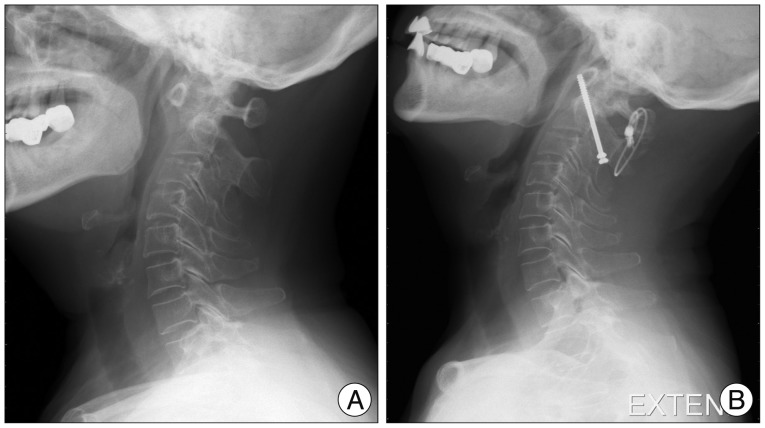
Fig. 2
A 66-year-old female had C1-2 instability due to complication of rheumatoid arthritis. Postoperative X-ray and CT scans show that the screw was safely inserted through the C1 lateral mass and the C2 pedicle. A : Pre-operative MRI. B : Post-operative cervical X-ray. C and D : Postoperative CT scans.

Fig. 3
Comparison of clinical results (operation time, radiation exposure time, blood loss) between transarticular screw fixation and C1 lateral mass-C2 pedicle screw fixation (*p<0.05).

Table 1
Charateristics of patients who underwent C1 lateral mass-C2 pedicle screw fixation or C1-2 transarticular screw fixaion

Table 3
Clinical outcome including NRS, ODI and Frankel grade were no definite difference between 2 groups





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download