Abstract
Objective
Post-traumatic stress disorder (PTSD) is a group of diseases that are observed in patients who had experienced a serious trauma or accident. However, some experienced it even after only a mild traumatic brain injury (TBI), and they are easily ignored due to the relatively favorable course of mild TBI. Herein, the authors investigated the incidence of PTSD in mild TBI using brief neuropsychological screening test (PTSD checklist, PCL).
Methods
This study was conducted on patients with mild TBI (Glasgow coma scale ≥13) who were admitted from January 2012 to December 2012. As for PCL, it was done on patients who showed no difficulties in communication upon admission and agreed to participate in this study. By using sum of PCL, the patients were divided into high-risk group and low-risk group. PTSD was diagnosed as the three major symptoms of PTSD according to the Diagnostic and Statistical Manual of Mental Disorders, fourth-edifion.
Results
A total of 314 TBI patients were admitted and 71 of them met the criteria and were included in this study. The mean age was 52.9 years-old (range: 15-94). The mean PCL score was 28.8 (range: 17-68), and 10 patients were classified as high-risk group. During follow-up, 2 patients (2.7%) of high risk group, were confirmed as PTSD and there was no patient who was suspected of PTSD in the low-risk group (p=0.017).
Post-traumatic stress disorder (PTSD) is a group of diseases observed in patients who feel a sensation of fear with physical and mental symptoms since their experience of severe trauma. The PTSD symptoms are so severe that the patient's normal social activities are often adversely affected4,19,20). The patient's mental anguish is amplified, because PTSD could hardly be diagnosed based on external deformations or image test results. The World Health Organization has designated PTSD as a silent epidemic disease to highlight its seriousness26).
Mild traumatic brain injury (TBI) accounts for more than 85% of all brain injuries, but it is attracting less clinical attention than moderate or severe brain injury because it shows comparatively favorable prognoses1,25). However, some mild TBI patients complain of severe psychological problems for a long period even though their image test results are acceptable11,17,24). Despite its clinical importance, PTSD in mild TBI patients may not be taken seriously because it could be associated with non-medical factors such as receiving insurance coverage from malingering. So, its prevalence has not been sufficiently investigated and easily ignored14,15,21,23,26). In this report, the authors investigated the prevalence of PTSD after mild TBI, and the clinical efficacy of the PTSD checklist (PCL) for screening the PTSD.
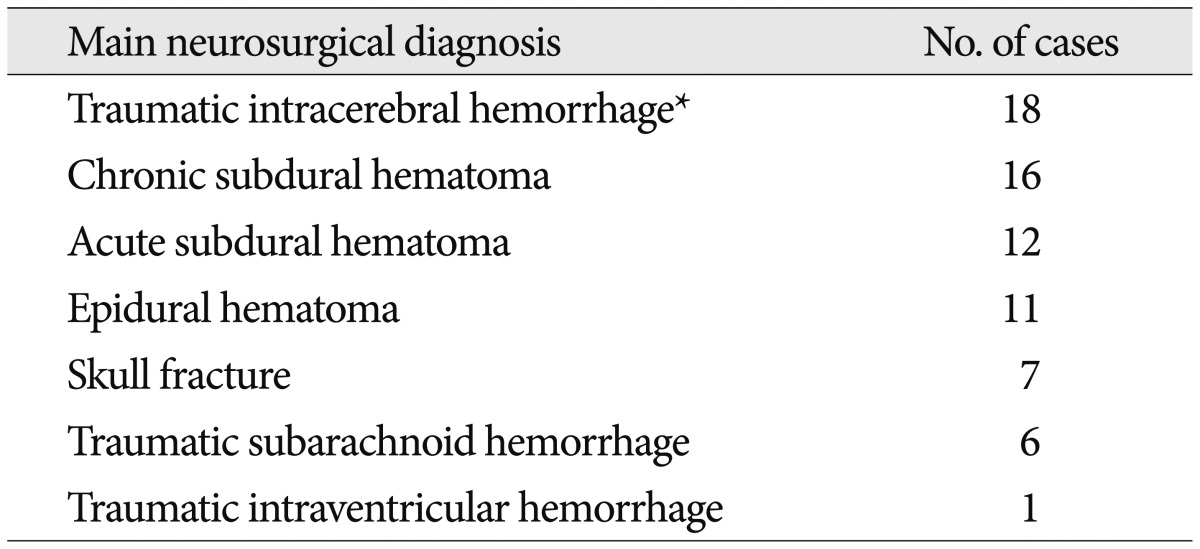
Demographic data for all patients were obtained from a prospectively maintained database. This study was conducted after approval of the institutional review board of Ajou University medical center (AJ IRB-MED-OBS-14-043). All patients were mild TBI patients who were admitted to the emergency center single university hospital between January 2012 and December 2012. Mild TBI was defined as a case with between 13 and 15 of Glasgow coma scale. All patients were given serial cranial computed tomography to check the presence of intracranial hemorrhage or skull fracture accompanied by headache and dizziness. All patients were observed for at least 24 hours from admission to check their neurological progression. The neurological diagnosis was categorized into acute subdural hematoma, chronic subdural hematoma, epidural hematoma, traumatic intracerebral hemorrhage (contusional hemorrhage), traumatic subarachnoid hemorrhage, traumatic intraventricular hemorrhage, or skull fracture, and the patients were categorized according to the main neurological diagnosis. The patients who could communicate by reading and writing were selected for PTSD check list (PCL) after informed consent form was taken.
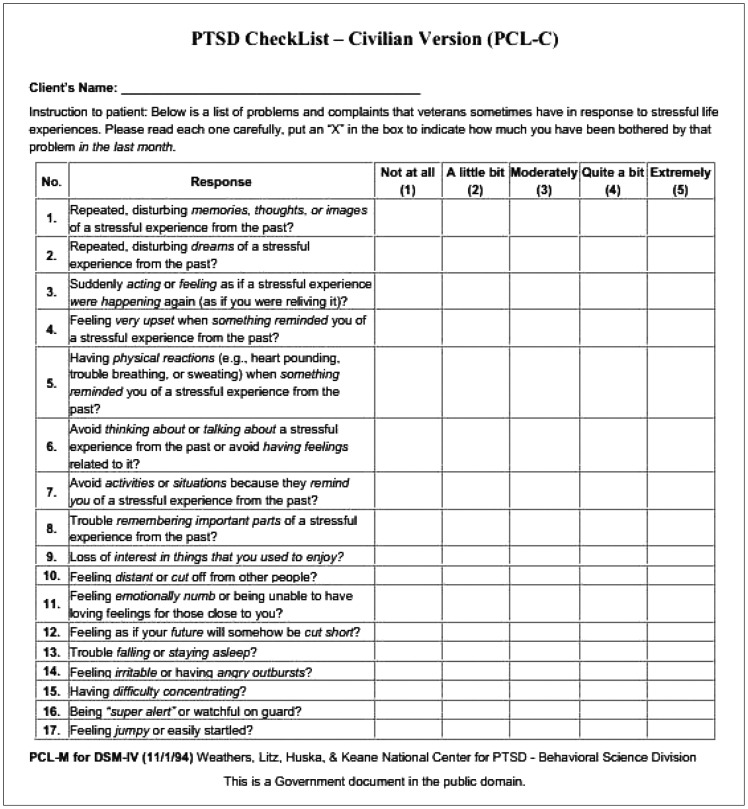
PCL was the US-identified test items translated to Korean2). PCL had 17 questions, and each subject scored between one mark (no symptom) and five marks (severest symptom) according to their severity from owns experience (Fig. 1). Each question referred to the PTSD symptoms such as intrusive recollect, upset by reminders, distressing dreams, physical reactions to reminders, avoid thoughts, avoid reminders, psychogenic amenesia, anhedonia, estrangement from others, psychic numbing, foreshortened future, sleep difficulty, irritability/anger, concentration impaired, hyper-vigilant, and exaggerated startle. PCL score was presented as sum of each item score, and the patients with a total score of 44 or more were classified as high-risk group, and those with less than 44 as low-risk group14,19). The diagnosis of PTSD was followed the Diagnostic and Statistical Manual of Mental Disorders, fourth-edifion diagnostic criteria: experiencing symptoms of recollection, avoidance and hyper-arousal for more than a month during the follow-up period12). During the same period, the improvements and changes in the symptoms were monitored, and the subjects who could not visit the hospital were monitored through telephone interviews.
The numbers of the PTSD-suspected patients in the high and low-risk groups were compared using the chi-square test, and the differences in their clinical features were investigated. For the comparison, SPSS 19.0 (SPSS Inc., Chicago, IL, USA) was used in the Mann-Whitney U test. Statistical significance was defined when p-value was lesser than 0.05.
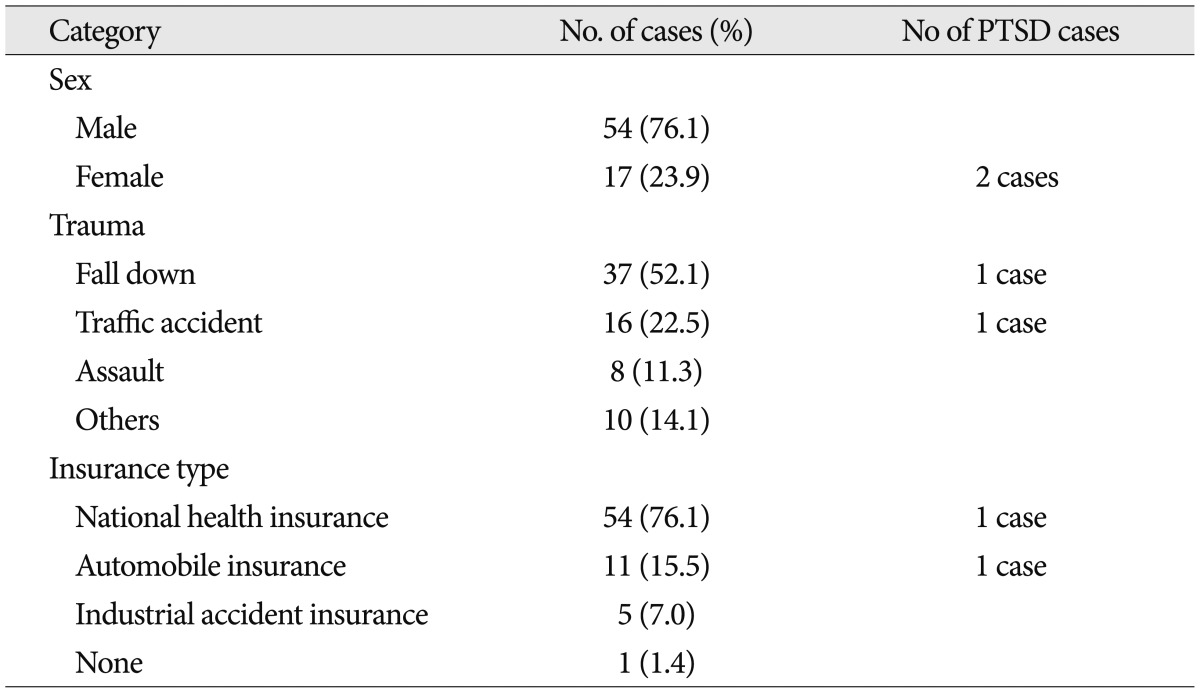
Totally, 341 TBI patients were admitted during the period, and 71 mild TBI patients were met the inclusion criteria and completed the PTSD screening test and the follow-up process. Their mean age was 50.4 (range: 17-84) and 54 cases (76.1%) of them were male (Table 1). Mean follow-up period was 4.0 months (range: 2.2-8.0). Slip down was the most common injury mechanism with 37 cases (52.1%) after fall down, 16 cases (22.5%) after traffic accident, 8 cases (11.3%) with assault, and unknown traumatic event was 10 cases (14.1%). The main neurological diagnosis were followed as 18 cases (25.4%) with traumatic intracerebral hemorrhage (contusional hemorrhage), 16 cases (22.5%) with chronic subdural hematoma, 12 cases (16.9%) with acute subdural hematoma, 11 cases (15.5%) with epidural hematoma, 7 cases (9.9%) with skull fracture, 6 cases (8.5%) with traumatic subarachnoid hemorrhage, and a case (1.4%) with traumatic intraventricular hemorrhage. The insurance types were national health insurance in 54 cases (76.1%), automobile insurance in 11 cases (15.5%), and industrial accident insurance in 5 cases (7.0%) (Table 2). Of the 71 subjects, no one underwent neurosurgical intervention, however, 22 (31%) underwent non-neurosurgical surgical treatments due to their accompanying traumas.
All 71 patients were divided into high and low-risk group for PTSD according to the sum of PCL. Ten patients (14.1%) were included in high-risk group and others were included in low-risk group. Two female cases among 10 patients in high-risk group showed three PTSD symptoms (recollection, avoidance and hyper-arousal) after they experienced trauma; a 32 years-old female with PCL score 48 after fall-down and a 39 years-old female with PCL score 49 after traffic accident. Both of them underwent further psychiatric treatment for PTSD. In the high-risk group, 6 subjects (60.0%) complained of at least one of the three PTSD symptoms, and 3 (30.0%) subjects take psychiatric medications. During the follow-up 2 patients of high risk group (2.8%) were confirmed as PTSD (Fig. 2). In the statistical analysis, the high and low-risk groups showed statistically significant differences, which confirmed the usefulness of the PCL scores for PTSD screening (p=0.017). No statistical correlation was observed between the PCL scores and the factors such as the injury mechanism, type of insurance.
PTSD is a group of diseases that are observed in patients who experience a serious incident and then feel fear and anguish from repeated recollections of such incident, and waste their energy in escaping from such feelings. Accordingly, PTSD patients' social activities are severely and adversely affected28). PTSD was introduced by Da Costa9) when they described the mental anguish of people who had experienced the American Civil War. In 1980, PTSD was defined as a response to a post-traumatic stress; and since then, it has been used as a diagnostic criterion. It was not widely understood in Korea, however, until the Sampoong Department Collapse in 1995. During the clinical observations of the survivors of the collapse, the severity of PTSD drew attention9,17). Since PTSD reflects the cultural backgrounds of the patient, its severity has often been neglected in Korea. In particular, only a few studies on PTSD after mild TBI have been conducted in Korea despite the high prevalence rate of mild TBI because mild TBI patients usually show favorable clinical courses.
It has been argued that PTSD cannot develop after TBI because of the impaired consciousness that is typically associated with TBI15,18,23). It has been suggested that the loss of consciousness or memory that occurs with TBI precludes encoding of trauma-related memories18). Some authors insist that if the trauma-related experience has not been encoded, one cannot have trauma-related memories that mediate re-experiencing PTSD symptoms18,22,23). In particular, Sbordone22) insisted that TBI patients cannot suffer PTSD because the injury to the brain results in a temporary 'shutting down' of its ability to process and record ongoing events. Many authors suggest that PTSD is more likely to occur in less severely brain-injured individuals, and that it may occur in mild TBI cases21). Inherent in this proposition is the assumption that anxiety that is causally related to the traumatic experience requires conscious recollections of the event.
According to the most recent studies, however, PTSD has also been observed in TBI patients with varying degrees of severity7). One of the possible mechanisms of PTSD is the deterioration of the medial prefrontal cortex that regulates the function of the amygdala8). The damage to the prefrontal networks due to the minor TBI may aggravate the functioning of these networks that are implicated in PTSD24). Second, cognitive models of PTSD propose that the extent to which people catastrophize a traumatic experience and its aftermath is pivotal in fueling PTSD10). This model assumes that trauma patients have adequate cognitive resources to use adaptive cognitive strategies for managing their traumatic experience. Minor TBI can damage the patient's cognitive resources and compromise his or her capacity to engage in the optimal cognitive strategies for managing the aftermath of a psychological trauma16).
The prevalence of PTSD after a mild TBI is known to be 17-33%, similar to that after a non-TBI patients5,6,13). Memory loss after a TBI is believed to seriously affect PTSD development. According to the study of Bryant3) on post-TBI and memory loss, which targeted 1167 trauma patients, PTSD was observed more often in TBI patients than the non-TBI patients, and the longer memory loss period was, the less PTSD developed.
PCL is a method of patient reporting of his or her own PTSD DSM-IV symptoms. It has been used to screen PTSD patients. There are two forms of PCL: PCL for the military and PCL for civilians2). PCL is composed of 17 questions, the answers to which are scored from 1 to 5, and the total score is computed by simply adding all the scores. In this study, we used the civilian version, which is almost identical to the military version, except that it inquires about a "stressful experience from the past," as opposed to military trauma. PCL is widely used as a self-rating PTSD-screening test for trauma patients, which is conveniently used in clinical cases. Cut off value of PCL is still in debate. Conventionally, 50 has been considered cut off value for screening test for PTSD27). Cut off value could be vary depending on the aims of the clinician or investigator, most of the reviewed studies recommended one or more cutting scores that often differ from conventions. Some authors chose cut scores to balance sensitivity and specificity whereas others recommended the cut score that offered the highest efficiency, although for others the rationale was not clear. Proposed cut scores are ranging from about 30 to 6019). We decided 44 as cut off value which somewhat lower than conventional one to increase sensitivity. Our result shows that PCL had a specificity of 88.4% and sensitivity of 100% and it is similar to previous review if we decide 44 as cut off value.
Our study was done on mild TBI patients who were admitted and put under surgical observation for several days. Although the sample size was not large, about 14% (10 of 71) of the mild TBI patients were considered to have had a risk of PTSD development, and 20% of them (2 of 10) were diagnosed with PTSD. Although 60% of patients of high risk patients did not meet the PTSD diagnostic criteria, we come to know that they suffering various psychological problems after mild TBI trauma. In this study, a PCL screening test was conducted for mild TBI patients to prospectively investigate the development of PTSD. In Korea, mild TBI patients have received less clinical attention than moderate to severe TBI patients due to their comparatively favorable clinical courses, but the prevalence rate of PTSD after mild TBI is estimated, through our study, to be about 2.8%, and such a number, although not high, is not one that can be overlooked, and PCL was confirmed to be an helpful tool in screening for high-risk patients.
There are some limitations in our study. PCL method is based on patient self-reports, so the subjective clinical manifestations can be over- or under-evaluated. Also, the diagnoses were not made by a psychiatrist but were based on the DSM-IV diagnostic criteria by neurosurgeon, which may yield a discrepancy from the psychiatric diagnoses. Further studies on this issue may be needed in future studies.
PTSD could be suspected in about 2.8% of mild TBI patients reportedly admitted to a hospital. Although the prevalence of PTSD after mild TBI is not high, PCL is thought to be a good screening test that can predict PTSD development in mild TBI patients. Further studies that can overcome the limitations of this study may be needed in the future.
References
1. Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J. Mild traumatic brain injury in the United States, 1998-2000. Brain Inj. 2005; 19:85–91. PMID: 15841752.

2. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. 1996; 34:669–673. PMID: 8870294.

3. Bryant RA. Disentangling mild traumatic brain injury and stress reactions. N Engl J Med. 2008; 358:525–527. PMID: 18234757.

4. Bryant RA, Creamer M, O'Donnell M, Silove D, Clark CR, McFarlane AC. Post-traumatic amnesia and the nature of post-traumatic stress disorder after mild traumatic brain injury. J Int Neuropsychol Soc. 2009; 15:862–867. PMID: 19703323.

5. Bryant RA, Harvey AG. Avoidant coping style and post-traumatic stress following motor vehicle accidents. Behav Res Ther. 1995; 33:631–635. PMID: 7654155.

6. Bryant RA, Harvey AG. Posttraumatic stress reactions in volunteer firefighters. J Trauma Stress. 1996; 9:51–62. PMID: 8750451.

7. Bryant RA, Harvey AG. Traumatic memories and pseudomemories in posttraumatic stress disorder. Appl Cogn Psychol. 1998; 12:81–88.

8. Charney DS, Deutch AY, Krystal JH, Southwick SM, Davis M. Psychobiologic mechanisms of posttraumatic stress disorder. Arch Gen Psychiatry. 1993; 50:295–305. PMID: 8466391.

9. Da Costa J. Art. I.-On irritable Heart; a clinical study of a form of functional cardiac disorder and its consequences. Am J Med Sci. 1871; 121:2–52.

10. Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. 2000; 38:319–345. PMID: 10761279.

11. Englander J, Hall K, Stimpson T, Chaffin S. Mild traumatic brain injury in an insured population: subjective complaints and return to employment. Brain Inj. 1992; 6:161–166. PMID: 1571720.

12. Foa EB. Post-traumatic Stress Diagnostic Scale (PDS). Minneapolis: National Computer Systems;1995.
13. Harvey AG, Bryant RA. The relationship between acute stress disorder and posttraumatic stress disorder: a 2-year prospective evaluation. J Consult Clin Psychol. 1999; 67:985–988. PMID: 10596520.

14. Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med. 2008; 358:453–463. PMID: 18234750.

15. King NS. PTSD and traumatic brain injury: folklore and fact? Brain Inj. 2008; 22:1–5. PMID: 18183503.

16. Landre N, Poppe CJ, Davis N, Schmaus B, Hobbs SE. Cognitive functioning and postconcussive symptoms in trauma patients with and without mild TBI. Arch Clin Neuropsychol. 2006; 21:255–273. PMID: 16716563.

17. Lee MS, Lee JS, Kwak DI. Severity of psychiatric symptoms in survivors of the sampoong accident. J Korean Med Assoc. 1997; 40:86–96.

18. Mayou R, Bryant B, Duthie R. Psychiatric consequences of road traffic accidents. BMJ. 1993; 307:647–651. PMID: 8401049.

19. McDonald SD, Calhoun PS. The diagnostic accuracy of the PTSD checklist: a critical review. Clin Psychol Rev. 2010; 30:976–987. PMID: 20705376.

20. McMillan TM, Williams WH, Bryant R. Post-traumatic stress disorder and traumatic brain injury: A review of causal mechanisms, assessment, and treatment. Neuropsychol Rehabil. 2003; 13:149–164. PMID: 21854332.

21. Rattok J, Boake C, Bontke CF. Do patients with mild brain injuries have posttraumatic stress disorder, too? J Head Trauma Rehabil. 1996; 11:95–102.

22. Sbordone RJ. Distinguishing traumatic brain injury from posttraumatic stress disorder. The Neurolaw Letter. 1992; 9:3.
23. Sbordone RJ, Liter JC. Mild traumatic brain injury does not produce post-traumatic stress disorder. Brain Inj. 1995; 9:405–412. PMID: 7640686.

24. Schneiderman AI, Braver ER, Kang HK. Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: persistent postconcussive symptoms and posttraumatic stress disorder. Am J Epidemiol. 2008; 167:1446–1452. PMID: 18424429.

25. Shindo T, Matsumoto Y, Wang Q, Kawai N, Tamiya T, Nagao S. Differences in the neuronal stem cells survival, neuronal differentiation and neurological improvement after transplantation of neural stem cells between mild and severe experimental traumatic brain injury. J Med Invest. 2006; 53:42–51. PMID: 16537995.

26. Vaishnavi S, Rao V, Fann JR. Neuropsychiatric problems after traumatic brain injury: unraveling the silent epidemic. Psychosomatics. 2009; 50:198–205. PMID: 19567758.

27. Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. San Antonio: The International Society for Traumatic Stress Studies;1993.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download