Abstract
Despite significant advances in the treatment of all forms of chronic otitis media (COM), complications still can and do occur, with intracranial complications representing the most life-threatening cases, often requiring immediate therapeutic intervention. Herein, we present a rare case of rapidly progressing facial paralysis with concomitant severe headache and ipsilateral hearing loss secondary to an otogenic brain abscess, treated with the transmastoid approach, drainage, and facial nerve decompression.
After meningitis, brain abscesses represent the second most common intracranial complication of chronic otitis media (COM)14), with an associated mortality rate ranging between 7% and 61% in most large series11,14). Roughly 50% of brain abscesses in adults and 25% in children are believed to stem from otogenic infections8,18), though the incidence has decreased due to the early treatment of chronic otitis media, the early diagnosis of associated complications, and the widespread use of antibiotics. Nonetheless, the exact timing of abscess drainage and the optimal method for approach remain controversial. Currently, most neurosurgery literature dictates that drainage via burr holes or complete lesion excision (including the abscess capsule) represent the gold-standard for surgical intervention16,17,18). However, not only are these two procedures associated with significant morbidity, and but neither address the treatment of the origin of infection. Herein, we describe the successful management of an otogenic brain abscess presenting as facial paralysis with concomitant headache and ipsilateral hearing loss using a transmastoid approach and subsequent facial nerve decompression and discuss the details of the technique and its specific advantages.
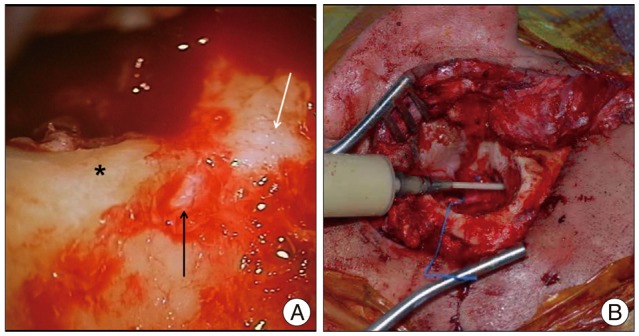
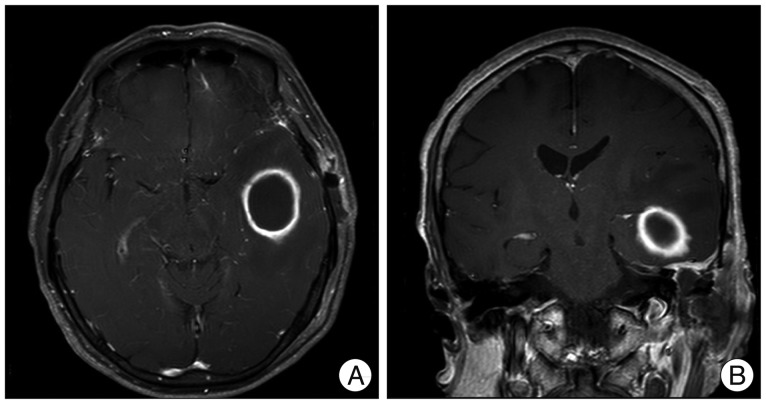
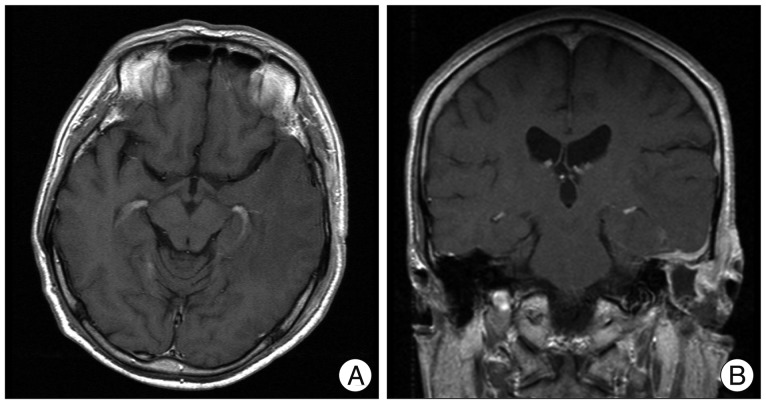
A 50-year-old man presented to our clinic for evaluation of progressive left facial paralysis, otalgia, intermittent otorrhea, mild dizziness, headache and hearing impairment. On physical examination, facial paralysis was rated as Grade III (per the House-Brackmann grading system). A further endoscopic examination revealed total perforation of the tympanic membrane, edema of the middle ear mucosa, and foul-smelling, purulent discharge from the left ear (Fig. 1), with left-sided caloric weakness of 71% found on subsequent electronystagmography. On further questioning, the patient denied any history of diabetes mellitus, hypertension, or pulmonary tuberculosis. Pure-tone audiometry was then performed, demonstrating near total deafness in the left ear. Given these findings, a temporal bone computed tomography (CT) scan was performed, revealing a soft tissue density filling the middle ear cavity and mastoid, possible dehiscence of the mastoid segment of the facial nerve, and pneumocephalus above the tegmen of the left ear. Magnetic resonance imaging (MRI) was also performed, revealing inflammation of the temporal lobe and an epidural abscess. At that time, the decision was made to treat with intravenous antibiotics for 3 weeks to allow the abscess in the temporal lobe to mature. However, as severe headaches and fever developed on day 7 of the IV antibiotic course. Follow-up MRI revealed immature abscess formation in the temporal lobe. Emergent surgical intervention was then scheduled to resolve the ongoing severe headaches, dizziness, and facial nerve paralysis. Specifically, the mastoid was removed via radical mastoidectomy, freeing a significant amount of cholesteatoma from the middle ear. During the operation, the dehiscence of the mastoid segment of the facial nerve was first identified (Fig. 2A) then decompressed, thus resolving any facial nerve paralysis. The tegmen was also found to be eroded, and, after removing many adherent granulations and burring out one portion, the abscess wall was exposed. Next, a needle was advanced into the abscess cavity via a healthy portion of dura, though no pus was able to be aspirated. However, after the 1st operation was undertaken, headache symptom was significantly relieved. Consequently, all further inteventions were deferred until the abscess was matured completely. After another 2-week course of IV antibiotics, a follow-up MRI revealed more mature abscess formation in the temporal lobe (Fig. 3). During the subsequent operation, an 18-gauge needle was advanced into the abscess, obtaining 12 mL of pus (Fig. 2B). The bony defect over the tegmen was closed using tragal and conchal cartilage, so that the free edges of the cartilage were hinged on the intracranial aspect. Temporalis fascia and perichondrium grafts were also transplanted over this area to reinforce the eroded tegmen, and the middle ear and mastoid cavity were repaired via a temporalis muscle rotation flap. Although the post-operative CT revealed a minimal residual abscess cavity, the facial paralysis and severe headache were completely resolved, and after an additional 8-week course of oral antibiotics, all evidence of the brain abscess had entirely disappeared (Fig. 4).
Although intracranial complications of COM are less common now than in years past, the associated incidence is estimated at between 0.13% and 1.97%12,13). Notably, cholesteatoma is an important risk factor for intracranial complications, as it is present in 78% to 100% COM cases that go on to develop complications5,6,12,13). The basic concepts in treating otogenic brain abscesses include immediate decompression of the abscess, prompt eradication of the primary otogenic nidus, and the active prevention of abscess recurrence. Otogenic brain abscesses with intracranial complications are often located adjacent to the temporal lobe and cerebellum, with the middle segment of the temporal lobe and lateral lobe of the cerebellum most highly affected. The infection spreads intracranially through bony defects in the tegmen tympani or Trautmann's triangle or via spread of an infected clot within small emissary veins of the skull to the venous sinuses. Given this location, such abscesses are often amenable to drainage via a transmastoid approach, thus avoiding an additional craniotomy13,14). In the case described here, computed tomography facilitated the diagnosis of a brain abscess associated with underlying ear disease, while a subsequent MRI provided additional information regarding the location of the abscess, the degree of mass effect, the presence of a midline shift, and disease stage18). Typically, treatment of otogenic brain abscesses first involves aspirating the pus or completely excising the abscess, after which parenteral antibiotic therapy is initiated to eradicate the primary nidus of infection1,3,7,9).
Repeated abscess drainage via burr holes and complete excision (including the abscess capsule) are both major operations associated with a higher incidence of neurological deficits.18) Conversely, the evidence shows that small abscesses can be treated with parenteral antibiotic therapy alone, and cases of multiple abscesses similarly respond best to parenteral antibiotic therapy after the largest lesion is aspirated2,9). If aspiration is performed, the abscess size should be monitored using weekly or biweekly CT scans to determine whether repeat interventions are required9,15). In all cases, the recommended course of parenteral antibiotic therapy is 6 to 8 weeks (following aspiration)9). In treating otogenic brain abscesses, the transmastoid approach has the advantage of eradicating the primary source of infection while additionally providing an easily accessible method for abscess aspiration in one or two stages4,10,18).
Although otogenic brain abscesses are relatively rare, both the otologist and neurosurgeon should be vigilant for any concerning clinical signs including persistent fever, headache, or purulent ear discharge as these represent the most common symptoms and signs of intracranial complications of COM. In conclusion, we contend that the transmastoid approach represents a good modality for otogenic brain abscesses with minimal neurologic sequelae.
Herein, the authors report a rare case of otogenic brain abscess with facial paralysis. Compared to the other modalities for therapeutic intervention, the transmastoid approach has the advantage of eradicating the primary source of infection while additionally providing an easily accessible method for abscess aspiration that represents a novel, safe, and effective treatment strategy to decrease mortality and morbidity. As such, we contend that otogenic abscesses can be effectively managed through cooperation between the neurosurgeon and otologist.
References
1. Aebi C, Kaufmann F, Schaad UB. Brain abscess in childhood--long-term experiences. Eur J Pediatr. 1991; 150:282–286. PMID: 2029923.

2. Basit AS, Ravi B, Banerji AK, Tandon PN. Multiple pyogenic brain abscesses : an analysis of 21 patients. J Neurol Neurosurg Psychiatry. 1989; 52:591–594. PMID: 2732727.
3. Bernardini GL. Diagnosis and management of brain abscess and subdural empyema. Curr Neurol Neurosci Rep. 2004; 4:448–456. PMID: 15509445.

4. Hippargekar PM, Shinde AD. Trans-mastoid needle aspiration for otogenic brain abscesses. J Laryngol Otol. 2003; 117:422–423. PMID: 12803800.

5. Kangsanarak J, Fooanant S, Ruckphaopunt K, Navacharoen N, Teotrakul S. Extracranial and intracranial complications of suppurative otitis media. Report of 102 cases. J Laryngol Otol. 1993; 107:999–1004. PMID: 8288994.

6. Kurien M, Job A, Mathew J, Chandy M. Otogenic intracranial abscess : concurrent craniotomy and mastoidectomy--changing trends in a developing country. Arch Otolaryngol Head Neck Surg. 1998; 124:1353–1356. PMID: 9865758.
7. Lu CH, Chang WN, Lui CC. Strategies for the management of bacterial brain abscess. J Clin Neurosci. 2006; 13:979–985. PMID: 17056261.

8. Ludman H. Complications of suppurative otitis media. In : Scott-Brown WG, Kerr AG, Groves J, editors. Scott-Brown's otolaryngology. ed 5. London: Butterworths;1987. p. 264–291.
9. Moorthy RK, Rajshekhar V. Management of brain abscess : an overview. Neurosurg Focus. 2008; 24:e3. PMID: 18518748.
10. Morwani KP, Jayashankar N. Single stage, transmastoid approach for otogenic intracranial abscess. J Laryngol Otol. 2009; 123:1216–1220. PMID: 19607739.

11. Nalbone VP, Kuruvilla A, Gacek RR. Otogenic brain abscess : the Syracuse experience. Ear Nose Throat J. 1992; 71:238–242. PMID: 1505373.
12. Osma U, Cureoglu S, Hosoglu S. The complications of chronic otitis media : report of 93 cases. J Laryngol Otol. 2000; 114:97–100. PMID: 10748823.
13. Penido Nde O, Borin A, Iha LC, Suguri VM, Onishi E, Fukuda Y, et al. Intracranial complications of otitis media : 15 years of experience in 33 patients. Otolaryngol Head Neck Surg. 2005; 132:37–42. PMID: 15632907.

14. Sennaroglu L, Sozeri B. Otogenic brain abscess : review of 41 cases. Otolaryngol Head Neck Surg. 2000; 123:751–755. PMID: 11112974.
15. Sharma BS, Gupta SK, Khosla VK. Current concepts in the management of pyogenic brain abscess. Neurol India. 2000; 48:105–111. PMID: 10878771.
16. Stapleton SR, Bell BA, Uttley D. Stereotactic aspiration of brain abscesses : is this the treatment of choice? Acta Neurochir (Wien). 1993; 121:15–19. PMID: 8475802.

17. Strowitzki M, Schwerdtfeger K, Steudel WI. Ultrasound-guided aspiration of brain abscesses through a single burr hole. Minim Invasive Neurosurg. 2001; 44:135–140. PMID: 11696881.

18. Syal R, Singh H, Duggal KK. Otogenic brain abscess : management by otologist. J Laryngol Otol. 2006; 120:837–841. PMID: 16824235.
Fig. 1
Total perforation of the tympanic membrane, edematous mucosa, and profound discharge documented on endoscopic examination of the left ear.
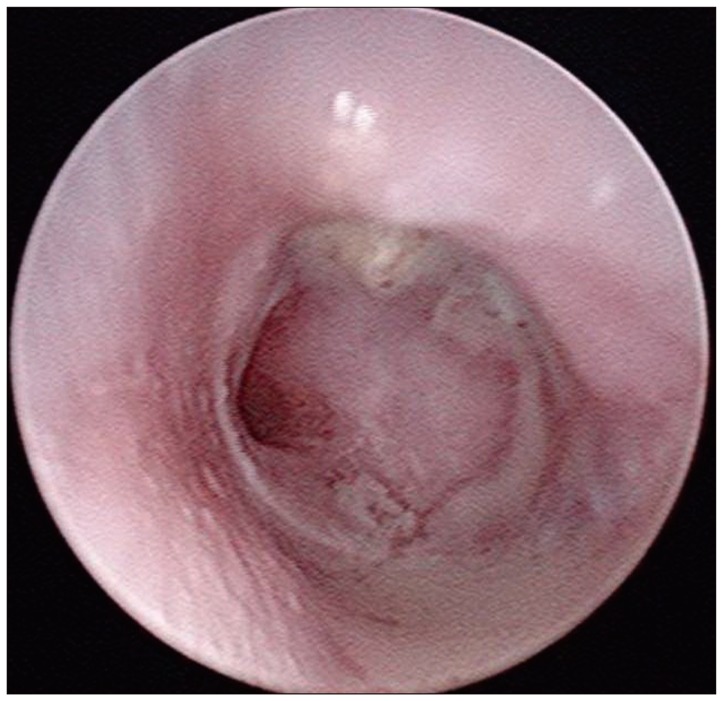
Fig. 2
A : The dehiscence of the mastoid segment of the facial nerve was identified during the 1st operation (black arrow : mastoid segment of the facial nerve, white arrow : lateral semicircular canal, asterisk : lower posterior wall of thee external auditory canal). B : An 18-gauge needle was advanced into the abscess via the transmastoid approach, yielding 12 mL of pus.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download