Abstract
Neurocysticercosis is the commonest parasitic disease of the human central nervous system. The incidence of intra ventricular form of neurocysticercosis (NCC) is less common accounting 10-20% that of total central nerve system cysticercosis. Intra ventricular NCC is complicated due, to its high incidence of acute hydrocephalus caused by ball valve mechanism. The only reliable tool for diagnosis of NCC is by neuroimaging with CT or MRI. MRI preferred over CT because of its high specificity and sensitivity. In emergency situations like acute hydrocephalus one can proceed with emergency endoscopic surgery. Through the endoscopic view, intra ventricular NCC (IVNCC) has distinguished morphological features like the full moon sign. This feature not only helps in identification of IVNCC, but also guides in further endoscopic treatment strategy. Authors report two cases of 3rd ventricular NCC with acute hydrocephalus managed with emergency endoscopy. Authors have discussed the clinical features, intra operative endoscopic findings and role of endoscopy in emergency surgery for NCC with acute hydrocephalus.
Neurocysticercosis (NCC) is one the common parasitic infestation of the central nervous system caused by the larval stage of taenia solium (T. Solium). It is endemic in most developing countries as well as in industrialized nations. Humans are incidental intermediate hosts in the life cycle of the T. solium10,12,14). Among the NCC, intraventricular form accounts for 10-20%14). One of the acute presentations of the intra ventricular NCC is life threatening intermittent hydrocephalus (Bruns Phenomena), which can occur due to cyst induced cerebrospinal fluid (CSF) flow obstruction from a ball valve mechanism19). At times, this can cause brain herniation leading to sudden death1,3,7,8,9,13,17,18,19). These cases require emergency management to avoid any serious complications. Authors reported two cases of third ventricular NCC presented with features suggestive of Bruns syndrome, and discussed their management with emergency endoscopic surgery.
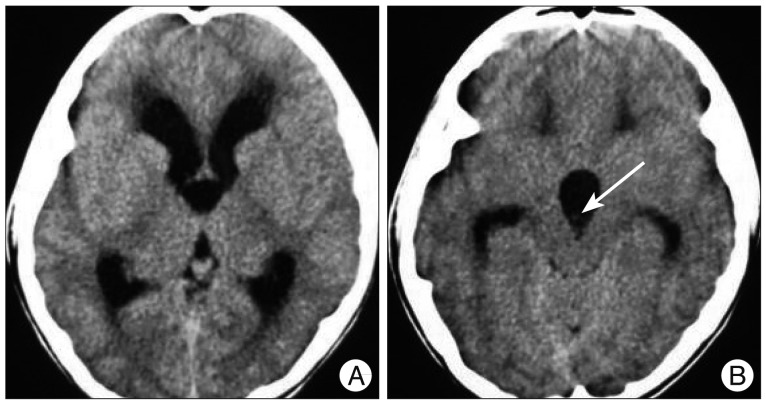
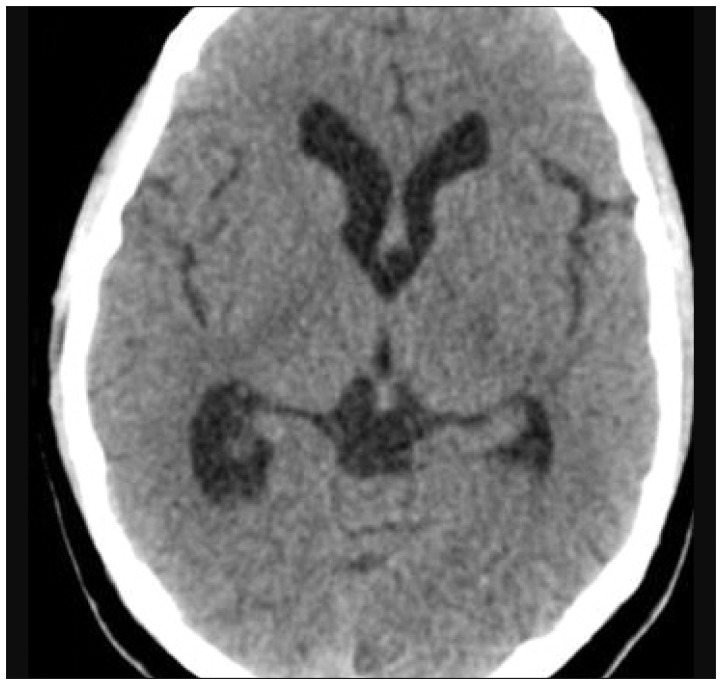
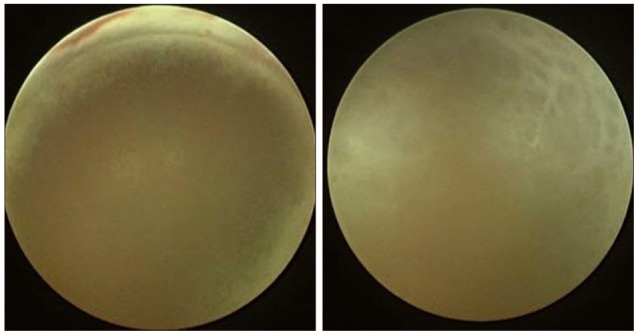
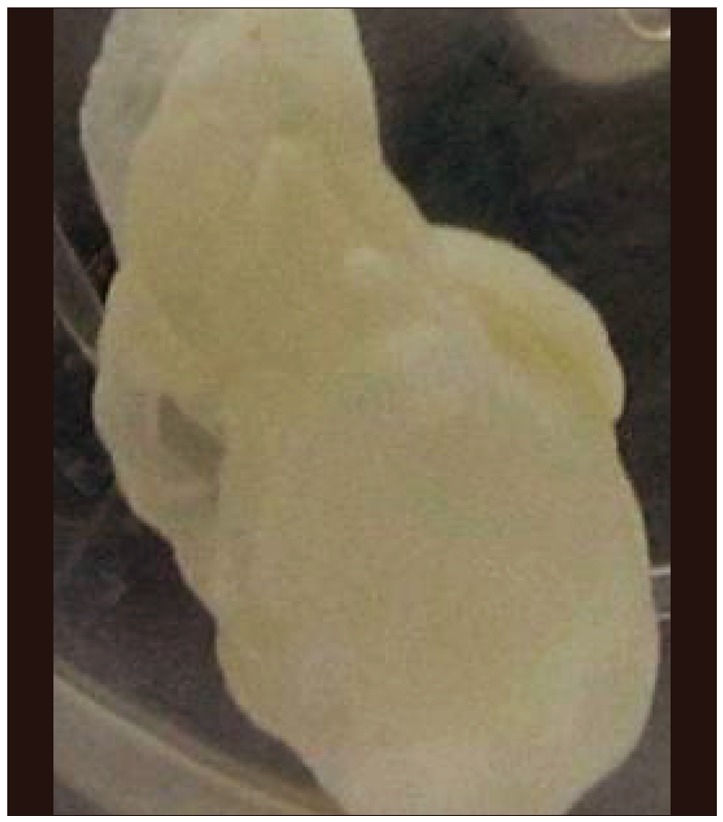
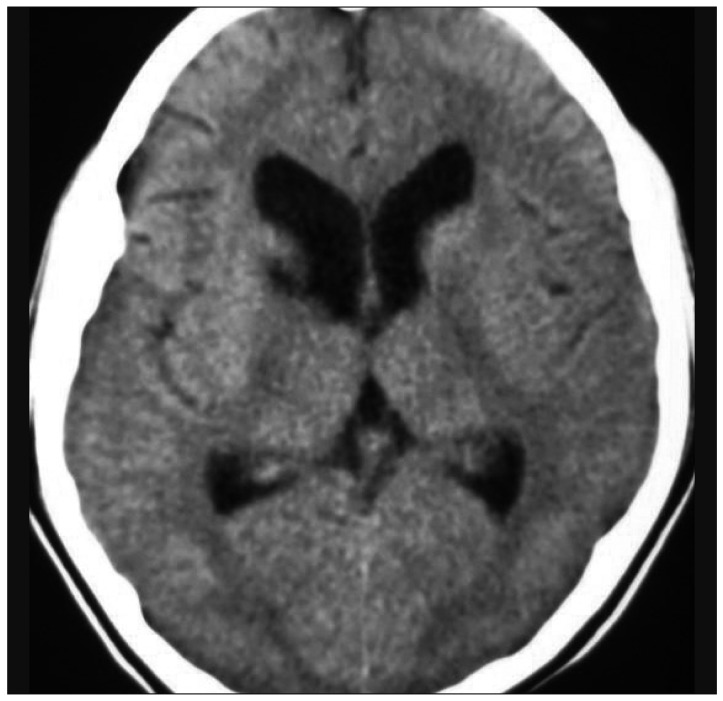
A 17-year-old female presented with history of on and off intense headache for the last two weeks and sudden loss of consciousness on the day of admission. She had two episodes of vomiting. There was no record of fever, neck rigidity. On examination, she was unconscious with Glasgow Coma Scale (GCS) E2V2M5 and semi dilated, sluggishly reacting pupils. She was intubated in the casualty. She was afebrile with stable vitals. Computed tomography (CT) (Fig. 1) of brain revealed gross hydrocephalus with an ill defined cystic lesion in the dilated third ventricle. With a provisional diagnosis of 3rd ventricular neurocysticercosis, an emergency endoscopic surgery was performed. Distinct endoscopic features suggestive of full moon sign reinforced the provisional diagnosis of intra ventricular neurocysticercosis (IVNCC) (Fig. 2). Following the cyst removal (Fig. 3), total ventricular cavity was inspected with angled scopes and found that it was solitary cyst. Left lateral ventricle was inspected through a small septostomy. There was severe ependymitis and thickened ventricular floor. Finally endoscopic third ventriculostomy (ETV) was done to prevent the delayed hydrocephalus. Postoperatively, patient recovered well and regained full consciousness. There were no added post operative deficits. Histopathological examination confirmed the diagnosis of NCC (Fig. 4). Patient was treated with albendazole for one week and continued on antiepileptic medicines for six months. There was no evidence of hydrocephalus in six months follow up CT scan (Fig. 5). At two years follow up, she is doing fine.
A 15-year-old female presented with complaints of headache and vomiting from one month and altered sensorium from one day. There was no history of seizures. CT scan of brain revealed hydrocephalus with dilated lateral and third ventricles (Fig. 6). Cysticercus lesion was seen in the dilated third ventricle. An endoscopic cyst removal was done through right precoronal burr hole. The third ventricle was filled with the cysticercus lesion and completely obstructing the Foramen of Monroe and appeared as a "full moon" (Fig. 7). Cyst was removed completely (Fig. 8) and the ETV was not done as the ventricular cavity was appearing healthy. Postoperatively there were no complications. Postoperative CT scan three months after surgery showed resolved hydrocephalus (Fig. 9). She was kept on cysticidal treatment to complement the surgical treatment. At six months of follow-up, she had no recurrence of symptoms or fresh complaints.
Following general anesthesia, patients were placed in supine position with head turned to left side by 15°. A right frontal burr hole was marked at 3 cm lateral to the midline and 3 anterior to the coronal suture. The scalp was shaved around the right fore head around the burr hole location. After appropriate preparation and draping, adequate sized right frontal precoronal burr hole was made. Dura was incised in a cruciate manner; the pia matter was coagulated and cut. Endoscopic trochar and cannula mounted on the endoscope holder was introduced in to the right lateral ventricle. A 5.5 mm rigid endoscope (Karl Storz, GmbH & Co.KG, Tuttlingen, Germany) was introduced to evaluate the intra ventricular pathology. A cyst which was floating, malleable, uneven surface and having dark discolored patches at places was located in the anterior third ventricle. The rigid scope was replaced with working scope and the cyst was grasped with a grasping forceps. While retrieving the cyst, the grasping forceps holding the cyst was removed along with working endoscope, to avoid the rupture of the cyst in the precise working channel. After cyst removal, the ventricle anatomy was reviewed for the evidence of any additional cysts with 30° and 45° angled scopes. Ventricle was irrigated with copious amounts of ringer lactate solution to remove the white debris.
NCC is the commonest parasitic infestations of the human central nervous system (CNS) and can involve any area of the CNS5,9,16). Intra parenchymal NCC is common and other forms are intraventricular, cisternal and spinal NCC5). Among all these, IVNCC is a potentially life threatening problem. Sometimes, IVNCC can be associated with acute obstructive hydrocephalus leading to brain herniation and sudden death, emphasizing the need for early detection and emergency treatment1,3,5,7,8,9,13,15,16,17,18,19). Large IVNCC with their free movement in the ventricular system can lead to intermittent acute occlusion of foramen of Monroe or aqueduct of sylvius due to ball valve mechanism, which is also known as Bruns syndrome19). Both these cases reported by authors, presented with features of raised intra cranial pressure in emergency.
The diagnosis of NCC is a multimodality approach and includes systematic evaluation of clinical features, neuroimaging and serology5,15). Serological analysis has a limited role in case of emergency due to their limited sensitivity and specificity5,7,13,18). The only reliable tool for diagnosis of IVNCC is imaging by computed tomography (CT) or magnetic resonance imaging trans(MRI)5,12,15,16). CT is less sensitive than MRI, as there is slight variation between CT attenuation values of cyst fluid and CSF. MRI with CSF flow study and Three dimensional Constructive Interference in Study State (3D CISS) sequence for the demonstration of an intraventricular cyst will provide proper diagnosis15). In critical situations one has to plan the emergency treatment based on the regular CT scan than MRI. Both the cases authors reported, did not have the requisite time for careful MRI evaluation due to the poor neurological level and were subjected for emergency endoscopic surgery.
In CT scan, author could demonstrate the cyst outline in the dilated third ventricle. Along with third ventricular dilation, there was gross dilatation of both lateral ventricles. Based on the clinical features and CT imaging, the IVNCC was the first differential diagnosis. Other possibilities could be intraventricular arachnoid cyst or post infective hydrocephalus due to TBM2,11).
The treatment options are medical management, ventriculo peritoneal shunt (VPS), microsurgery and endoscopic surgery alone or in combination7,9,15,18). Medical management alone is out of favor because of the limited effectiveness of albendazole and praziquentel. Though there is no general consensus regarding ideal surgical treatment of intraventricular NCC, neuroendoscopy is preferred over microsurgery and VPS18,19). Microsurgery for NCC removal needs craniotomy, more brain invasion, increases operative time, blood loss, increased hospital stay and expenses1,7). On the other hand, VPS is associated with more post operative complications like shunt malfunction, repeat surgeries2,6,7). Because of its minimal invasive nature, endoscopic surgery has less brain injury, operative time and blood loss. Moreover, endoscopy allows a quick and relatively easy approach to the single or multiple cysts located within the ventricles8,13). By using endoscope, one can remove the cysts, and as well do ETV to prevent the delayed hydrocephalus. Delayed hydrocephalus commonly seen in cases treated by microsurgery or VPS2,6). Even in emergency, endoscopy plays a role in intra operative diagnosis of these lesions with their distinct features like "full moon" sign (Fig. 2, 7)14). Ramos-Zúñiga et al.14) reported the specific features and consistent correlation between macroscopic endoscopic view of the intraventricular vesicular stage NCC and appearance of the full moon. This unique analogy was also seen by authors and allowed the diagnosis of IVNCC. They also opined that, this endoscopic sign is not seen in other intraventricular cysts or tumors. Implications of such findings are not only clinically relevant for the diagnostic clarification but also help in therapeutic planning. Hence, neuroendoscopic removal of the IVNCC with hydrocephalus is the preferred surgery where ever the expertise is available14,18,19).
Both the cases were reported by authors presented with acute hydrocephalus with altered sensorium. Patients reported to the author with a CT scan done already from other peripheral centers. An emergency endoscopic surgery and cyst removal was done. In both the cases, presumptive clinic-radiological diagnosis of the IVNCC was reinforced with endoscopic imaging features of full moon sign. After cyst removal, 30° and 45° angled endoscopes are used for detailed examination of ventricles. Opposite left lateral ventricle was visualized with the use of small septostomy. In first case ETV was done at the end as there were features of diffuse ependymitis to prevent the delayed hydrocephalus due to fibrosis and aqueductal stenosis. In second case as the ventricle was appearing healthy without the evidence of ependymitis, ETV was not done. First case at two years and the second one at six months follow up period did not show hydrocephalus or recurrence of symptoms.
Intraventricular NCC with acute hydrocephalus continues to be a potentially fatal condition if not addressed well in time. Although active and vesicular NCC does not produce host reaction, they can hinder CSF movement with ball valve mechanism, leading to the complex clinicopathological entity of hydrocephalus known as "Bruns syndrome". Emergency neuroendoscopy helps in diagnosing the IV NCC with their distinct features like full moon sign. It also helps in removal of the cyst and establishment of alternative CSF flow channel by ETV to prevent the delayed hydrocephalus. Thus, where ever the facilities are available, neuroendoscopic surgery should be the modality of first choice for treatment of IVNCC with hydrocephalus.
References
1. Anandh B, Mohanty A, Sampath S, Praharaj SS, Kolluri S. Endoscopic approach to intraventricular cysticercal lesions. Minim Invasive Neurosurg. 2001; 44:194–196. PMID: 11830776.

2. Apuzzo ML, Dobkin WR, Zee CS, Chan JC, Giannotta SL, Weiss MH. Surgical considerations in treatment of intraventricular cysticercosis. An analysis of 45 cases. J Neurosurg. 1984; 60:400–407. PMID: 6607328.
3. Bergsneider M, Holly LT, Lee JH, King WA, Frazee JG. Endoscopic management of cysticercal cysts within the lateral and third ventricles. J Neurosurg. 2000; 92:14–23. PMID: 10616077.

4. Buxton N, Punt J. Cerebral infarction after neuroendoscopic third ventriculostomy : case report. Neurosurgery. 2000; 46:999–1001. discussion 1001-1002. PMID: 10764279.

5. Carpio A. Neurocysticercosis : an update. Lancet Infect Dis. 2002; 2:751–762. PMID: 12467692.
6. Colli BO, Martelli N, Assirati JA Jr, Machado HR, de Vergueiro Forjaz S. Results of surgical treatment of neurocysticercosis in 69 cases. J Neurosurg. 1986; 65:309–315. PMID: 3734881.

7. Goel RK, Ahmad FU, Vellimana AK, Suri A, Chandra PS, Kumar R, et al. Endoscopic management of intraventricular neurocysticercosis. J Clin Neurosci. 2008; 15:1096–1101. PMID: 18653345.

8. Husain M, Jha DK, Rastogi M, Husain N, Gupta RK. Neuro-endoscopic management of intraventricular neurocysticercosis (NCC). Acta Neurochir (Wien). 2007; 149:341–346. PMID: 17342378.

9. Husain M, Rastogi M, Jha DK, Husain N, Gupta RK. Endoscopic transaqueductal removal of fourth ventricular neurocysticercosis with an angiographic catheter. Neurosurgery. 2007; 60(4 Suppl 2):249–253. discussion 254. PMID: 17415160.

10. Matushita H, Pinto FC, Cardeal DD, Teixeira MJ. Hydrocephalus in neurocysticercosis. Childs Nerv Syst. 2011; 27:1709–1721. PMID: 21928035.

11. McLaughlin MR, Wahlig JB, Kaufmann AM, Albright AL. Traumatic basilar aneurysm after endoscopic third ventriculostomy : case report. Neurosurgery. 1997; 41:1400–1403. discussion 1403-1404. PMID: 9402593.

12. Medina MT, DeGiorgio C. Introduction to Neurocysticercosis : a worldwide epidemic. Neurosurg Focus. 2002; 12:1–6.
13. Proaño JV, Torres-Corzo J, Rodríguez-DellaVecchia R, Guizar-Sahagun G, Rangel-Castilla L. Intraventricular and subarachnoid basal cisterns neurocysticercosis : a comparative study between traditional treatment versus neuroendoscopic surgery. Childs Nerv Syst. 2009; 25:1467–1475. PMID: 19557421.

14. Ramos-Zúñiga R, de La Cruz-Ramírez J, Casillas-Espinosa PM, Sánchez-Prieto JA, López-Hernández MD. "Full moon" endoscopic sign in intraventricular neurocysticercosis. Minim Invasive Neurosurg. 2011; 54:90–94. PMID: 21656445.

15. Singh S, Gibikote SV, Shyamkumar NK. Isolated fourth ventricular cysticercus cyst : MR imaging in 4 cases with short literature review. Neurol India. 2003; 51:394–396. PMID: 14652451.
16. Sinha S, Sharma BS. Intraventricular neurocysticercosis : a review of current status and management issues. Br J Neurosurg. 2012; 26:305–309. PMID: 22168964.

17. Suri A, Goel RK, Ahmad FU, Vellimana AK, Sharma BS, Mahapatra AK. Endoscopic excision of intraventricular neurocysticercosis in children : a series of six cases and review. Childs Nerv Syst. 2008; 24:281–285. PMID: 17994242.

18. Suri A, Goel RK, Ahmad FU, Vellimana AK, Sharma BS, Mahapatra AK. Transventricular, transaqueductal scope-in-scope endoscopic excision of fourth ventricular neurocysticercosis : a series of 13 cases and a review. J Neurosurg Pediatr. 2008; 1:35–39. PMID: 18352801.

19. Torres-Corzo J, Rodriguez-della Vecchia R, Rangel-Castilla L. Bruns syndrome caused by intraventricular neurocysticercosis treated using flexible endoscopy. J Neurosurg. 2006; 104:746–748. PMID: 16703879.

Fig. 1
CT scan brain images of first case (axial) showing hydrocephalus with dilated lateral and third ventricles.
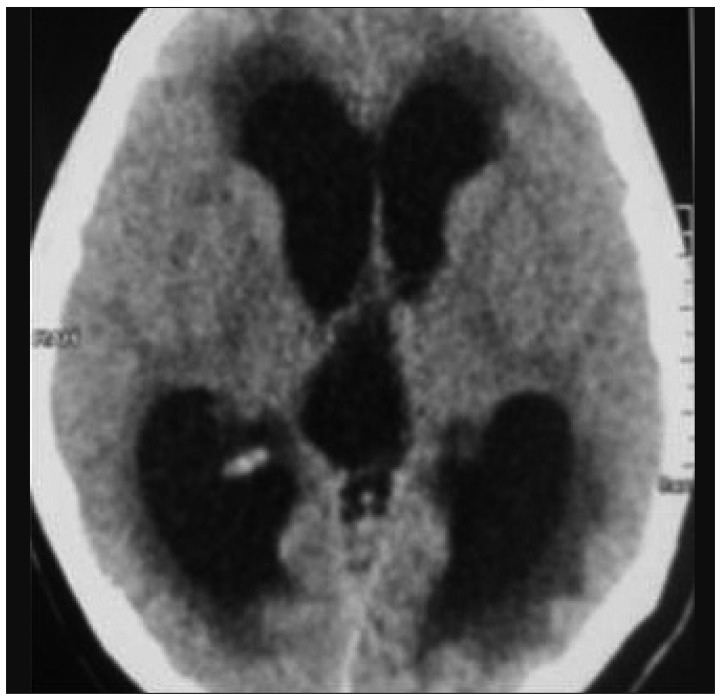
Fig. 2
A : Endoscopic view of cysticercus lesion seen obstructing the foramen of Monroe with surrounding relations. B : Cysticercus lesion appearing as the "Full moon" in the endoscopic view.
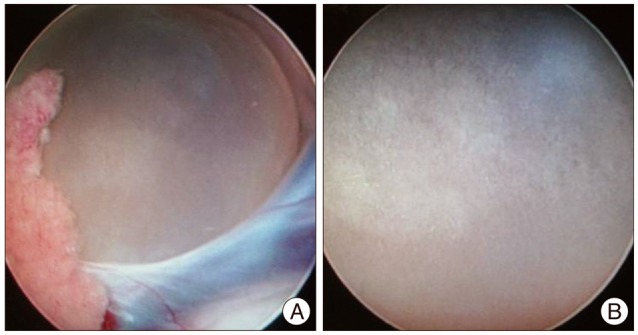
Fig. 3
A : Image showing the endoscopic view of foramen Monroe and third ventricle after the cyst removal. B : Image showing the thin walled cyst containing cysticercus larva in form of a nodule inside.
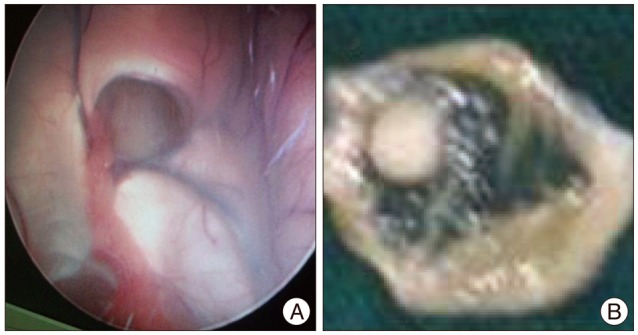
Fig. 4
Haematoxylin and eosin stained low power field image showing cysticercus larva. Cyst cavity is lined by three layers : cuticle, cellular and inner loose layer. Cephalic end of the larva showing an invaginated scolex having a sucker and hooklets is identified. Caudal end of scolex larva showing duct like invaginations surrounding a coelomic cavity.
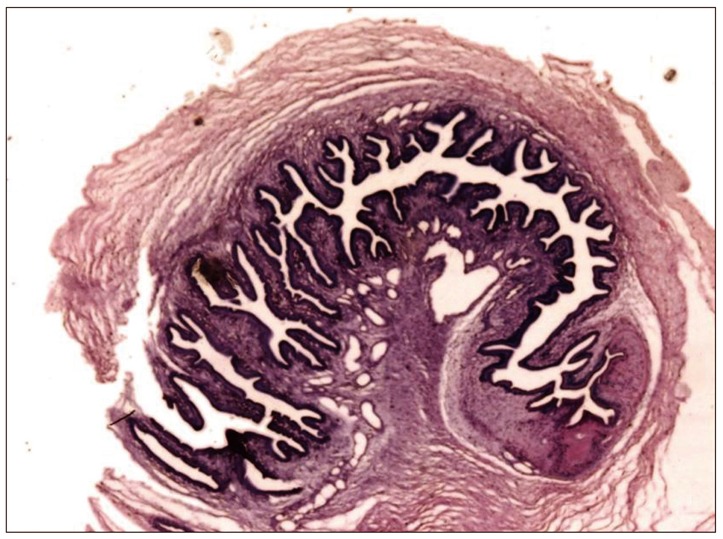
Fig. 6
Serial axial CT scan images (A) of second case showing hydrocephalus and a hyperdense nodular lesion in the third ventricle (B) (arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download