Abstract
Percutaneous epidural neuroplasty (PEN) is a known interventional technique for the management of spinal pain. As with any procedures, PEN is associated with complications ranging from mild to more serious ones. We present a case of intracranial subdural hematoma after PEN requiring surgical evacuation. We review the relevant literature and discuss possible complications of PEN and patholophysiology of intracranial subdural hematoma after PEN.
Go to : 
Percutaneous epidural neuroplasty (PEN) is one of many interventional techniques utilized for nonsurgical management of spinal pain. It is a minimally invasive technique developed nearly a decade ago to treat the pain from spinal radiculopathy8). Its mechanism of action is known as local epidural adhesiolysis, neurolysis of vertebral nerve roots and local lavage of inflammatory mediators by injections of local anesthetics, corticosteroids, hyaluronidase and hypertonic saline5).
However, adverse events of PEN are sometimes underestimated because of its simplicity of procedure. Complications of PEN include unintended dural puncture, administration of the drugs to the subarachnoid or subdural space, catheter shearing, catheter breakage, infection and severe hemodynamic instability. Theses complications may occur not only as a direct result of the procedure itself but also from specific drugs-related side effect11).
There have also been reports of intracranial hypotension and headache after neuroplasty2,3). However, there has been no reports on the case of subdural hematoma (SDH) occurring as a result of PEN, as far as we know. We report a rare case of SDH after PEN and discuss possible pathophysiology.
Go to : 
A 53-year-old right-handed male visited outpatient clinic due to progressive headache for one month. He reported that his headache started after PEN performed at another institution for his back and leg pain one month ago. As the catheter was inserted through the coccyges and came up to the back side, he had immediate anxiety associated with back pain and sweating. He felt palpitation of heart, which had never experienced before. After the procedure, his back pain and leg pain improved but headache started. His headache was aggravated by standing and relieved with lying down, least in the morning and worst at night. He also had intermittent nausea and anxiety. His headache worsened despite analgesics.
On his first outpatient visit three weeks after PEN, his mental status and the rest of his neurological examination were normal. The past medical history was otherwise unremarkable. He did not have a history of chronic alcohol consumption or coagulopathy, nor had he been on a medication that could affect coagulation. Physical examination was also unremarkable except for mild neck stiffness. He could not recall any trauma or injury except for PEN. Due to new-onset progressively worsening headache, brain MRI was recommended but he refused at that time.
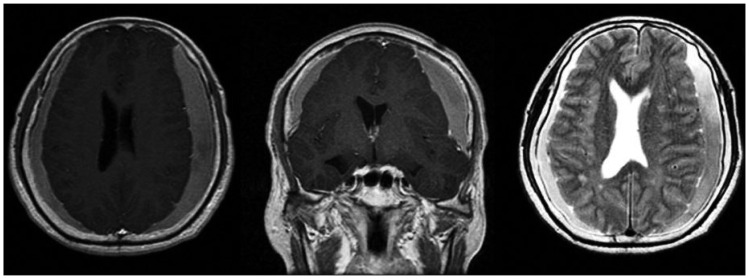
One week later when his headache worsened, even worse he agreed to brain MRI. It showed bilateral chronic subdural fluid collections compressing the brain (Fig. 1). The patient was taken to the operating room for bilateral burr hole evacuation of subdural fluid collection an placement of subdural catheter. Chronic subdural hematoma was confirmed in the operating room. He improved postoperatively with decreased headaches. We planned lumbar MRI to evaluate the site of neurolysis but patient refused because he was getting better.
Headache eventually resolved and brain computed tomography performed one month after burr hole trephination showed resolution of SDH (Fig. 2).
Go to : 
The procedure of PEN was introduced in 1981 as an alternative to epidural catheter for providing anesthesia or analgesia9). PEN is not only utilized in patients suffering from failed spine surgery but also increasingly utilized for non-surgical management of back pain8).
Excluding catheter-related complications, possible known complications of PEN include hypotension, respiratory depression, urinary and/or fecal incontinence, urinary hesitancy, sexual dysfunction, paresthesia, epidural abscess, and meningitis3). Talu and Erdine11) reported the complications from 250 neuroplasty cases; hypotension was seen during and after drug injections in 12 patients; three patients had migration and penetration of the catheter into the dura; 25 patients experienced numbness in dermatomal areas of the upper or lower extremities; there were eight infections at the entry site of the catheter, three epidural abscesses, and two patients with meningitis. In additions, inflammation, edema, fibrosis, venous congestion, pressure on the posterior longitudinal ligaments, annulus fibrosis, spinal nerves, and even central sensitization may occur.
Complications from epidural neuroplasty may occur as a direct result of the procedure or from the drugs administered as a part of neuroplasty. Erdine and Talu1) analyzed the differences between immediate and late complications. Complications relating to the procedure are usually seen immediately, while complications relating to drug administration are typically seen later. Immediate complications are bleeding in the epidural space, bending of the tip of the needle, penetration of the dura, subdural insertion of the catheter, shearing of the catheter, problems during the withdrawal of the catheter, severe pain during injection, blocking of the catheter, hypotension, and late complications are known to be delayed laceration of the dura, numbness in the dermatomal region, temporary paraesthesia, permanent paraesthesia, bowel and bladder dysfunction, sexual dysfunction, headache, infection at the site of penetration, epidural abscess, arachnoiditis1,7,10,12).
Intracranial hypotension can develop after cerebrospinal (CSF) leakage from inadvertent dural puncture and can be accompanied by various symptoms, including headache and neck pain. In recent years, cases of chronic subdural hematoma that develop concomitantly with intracranial hypotension have been reported4). In current case, we suspect that the patient had sudden headache and sweating as the dura was violated leading to CSF leak.
Authors' hypothesis is that during the PEN, CSF leak may occur due to dural tear, which could lead the intracranial hypotension and symptoms of headache and neck pain. Also, continuation of intracranial hypotension might lead the subdural hematoma.
Intracranial hypotension from CSF leak led to waxing and waning orthostatic headache. Sudden intracranial hypotension may stretch and tear of the intracranial bridging veins that eventually led to subdural hematoma. The fact that our patient had postural headache supports our contention that CSF leak lead to intracranial hypotension. Relatively stable neurologic status of the patient is consistent with a slow venous bleed from torn bridging veins.
There is similar case report of a 41-year-old woman with multiple sclerosis and intractable spasticity who developed a bilateral subacute subdural hematoma after the placement of an intrathecal catheter connected to a programmable pump for baclofen infusion4). We assumed that this similar report might support our presumptive pathologic mechanism. Additionally our hypothesis is supported by his negative history of trauma and uncommon age for chronic subdural hematoma.
Lad et al.3), discussed in detail the diagnostic tool of intracranial hypotension. They asserted that brain MRI was better than head CT in diagnosing intracranial hypotension. Brain MRI may demonstrate subdural fluid collection, enhancement of the pachymeninges, engorgement of venous structures, pituitary hyperemia and sagging of the brain. Epidural blood patch is an accepted treatment for headache associated with dura CSF leak when conservative management fails2).
MRI of the spine may help detect the exact location of the CSF leak for targeted epidural blood patch or surgical repair of the dural laceration; it may reveal characteristic findings such as epidural fluid collections, collapse of the dural sac accompanied by engorgement of the epidural venous plexus, and abnormalities of the root sleeves. Radioisotope cisternography could help with the detection of CSF leak either directly by accumulation of radioactivity outside the subarachnoid space or indirectly by a limited ascent of the tracer to the cerebral convexities and its early accumulation in the kidneys, urinary bladder, and soft tissues. CT myelography, however, remains the study of choice for localization of CSF leak. Mokri6) reported that CT myelography localized a CSF leak in 67% of patients overall compared with 50% and 55% for MRI and radioisotope cisternography, respectively. We could not find the objective evidence of CSF leakage, such as radioisotope cisternography and MRI. This might be the weak point of our study. If we had such a study for proofing CSF, that would also help us for treating this patient.
PEN is mostly safe but can lead to serious complications. However, we must aware of the possibility of such complications including intracranial hypotension and subdural hematoma. In order to reduce complications, we recommend that epidural neuroplasty procedures be performed in well-equipped centers by experienced hands.
In this article, we tried to assume not only the possible complication during PEN, but its presumptive pathologic mechanism to prevent and manage the complication.
Go to : 
We report a case of chronic subdural hematoma discovered one month after PEN.
The authors hypothesized that it was due to intracranial hypotension leading to chronic subdural hematoma. Physicians should be alert this potential complication during PEN and patient should know the possibility of such a unintended complication before the procedure.
Go to : 
References
1. Erdine S, Talu GK. Precautions during epidural neuroplasty. Pain Pract. 2002; 2:308–314. PMID: 17156038.

2. Khalid S, Das PG, Mohammad H, Hameed U. Spontaneous intracranial hypotension in a patient with Marfan's syndrome treated with epidural blood patch--a case report. Middle East J Anesthesiol. 2012; 21:635–638. PMID: 23327040.
3. Lad SP, Li G, Lin SC, Henderson JM. Intracranial hypotension from intrathecal baclofen pump insertion. A case report and review of the literature. Stereotact Funct Neurosurg. 2008; 86:75–79. PMID: 18073519.

4. Magro E, Remy-Neris O, Seizeur R, Allano V, Quinio B, Dam-Hieu P, et al. Bilateral subdural hematoma following implantation of intrathecal drug delivery device. Neuromodulation. 2011; 14:179–181. discussion 182. PMID: 21992208.

5. Manchikanti L, Bakhit CE. Percutaneous lysis of epidural adhesions. Pain Physician. 2000; 3:46–64. PMID: 16906207.

6. Mokri B. Cerebrospinal fluid volume depletion and its emerging clinical/imaging syndromes. Neurosurg Focus. 2000; 9:e6. PMID: 16859267.

7. Oh CH, An SD, Choi SH, Ji GY. Contrast mimicking a subarachnoid hemorrhage after lumbar percutaneous epidural neuroplasty : a case report. J Med Case Rep. 2013; 7:88. PMID: 23548107.
8. Park EJ, Park SY, Lee SJ, Kim NS, Koh do Y. Clinical outcomes of epidural neuroplasty for cervical disc herniation. J Korean Med Sci. 2013; 28:461–465. PMID: 23487574.

9. Racz GB, Sabonghy M, Gintautas J, Kline WM. Intractable pain therapy using a new epidural catheter. JAMA. 1982; 248:579–581. PMID: 7097904.

10. Ryu KS, Rathi NK, Kim G, Park CK. Iatrogenic intradural lumbosacral cyst following epiduroscopy. J Korean Neurosurg Soc. 2012; 52:491–494. PMID: 23323173.

11. Talu GK, Erdine S. Complications of epidural neuroplasty : a retrospective evaluation. Neuromodulation. 2003; 6:237–247. PMID: 22151070.
12. Wagner KJ, Sprenger T, Pecho C, Kochs EF, Tölle TR, Berthele A, et al. [Risks and complications of epidural neurolysis -- a review with case report]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2006; 41:213–222. PMID: 16636945.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download