Abstract
A case of an iatrogenic spinal arteriovenous fistula with progressive paraplegia in a young woman is reported. The fistula was eventually created after repetitive lumbar punctures performed in the process of spinal anaesthesia. Her symptoms were progressed to paraplegia over a period of 2 years. The digital subtraction angiography demonstrated a single-hole fistula, involving the anterior spinal artery and vein. The lesion was occluded by embolization with immediate improvement. The potential mechanism is discussed.
Even though the real incidence of neurologic complications arising from spinal anaesthesia is not known, these seem to be very rare2,3,5,7). Usually, these complications include compression of the spinal cord or nerve roots secondary to subdural or epidural haematoma or abscess, direct trauma of the spinal cord or root and neurotoxicity due to the injected anaesthetics1,2,9,11,16,17,21).
Direct arteriovenous fistulas (AVFs) are the simplest type of arteriovenous shunts of the spinal cord1,17). Single shunts are presented either in the context of a genetic hereditary disorder or as sporadic lesions of unknown etiology8,10). There has been no documented case of traumatic aetiology published so far.
We report a case of an iatrogenic traumatic spinal AVF presented with progressive paraplegia in a 20-year-old young woman. The fistula had most probably resulted as a complication of repetitive lumbar punctures performed in the process of spinal anaesthesia. The value of proper technique for spinal anaesthesia is emphasized.
A 20-year-old female was referred to our hospital, with a history of progressive sensory-motor paraplegia and a spinal magnetic resonance imaging (MRI) demonstrating conus medullaris edema as well as dilated vessels on the cord surface. Her history began two years prior to her admission to our hospital, while she was admitted to another hospital with acute abdomen and the suspicion of a ruptured ectopic pregnancy. For some reason, most likely related to the fact that she had eaten shortly before her admission, spinal anaesthesia was decided instead of general anesthesia. Several unsuccessful attempts for access were made. She described that during those attempts she felt a sharp electric current-like sensation in both the lower extremities followed by pins and needles-like sensation. She complained intensely and further attempts were aborted. Thereafter and during her hospitalisation she was complaining of disturbing sensory symptoms involving her legs. Over the following weeks, she started to have a progressive 'numbness' of her lower limbs followed by slowly progressive spastic paraplegia over the next twenty months. During that period and especially soon after her discharge, she visited her family doctor and described her problem, which was not properly evaluated and further investigation was not followed. She was getting worse in spite of physiotherapy, which was suggested. During the last six months she developed clear spasticity and paraparesis and was investigated by MRI, which revealed conus medullaris edema and dilated vessels on the surface of the spinal cord. A vascular lesion was suspected and the patient was referred to us for further investigation and treatment. On admission the general physical and systemic examination was unremarkable except for the neurological findings. No family history or sign of any genetic disease related to a central nervous system vascular lesion was discovered. Her neurological findings included severe spastic paraplegia-she came on a wheelchair-with hypoesthesia below the twelfth thoracic (T12) dermatome. Tone was markedly increased, and knee reflexes were exaggerated. Both the plantar reflexes were elicited with an up-going great toe and both her legs were affected by some atrophic changes. Bladder and intestinal sphincter function were preserved.
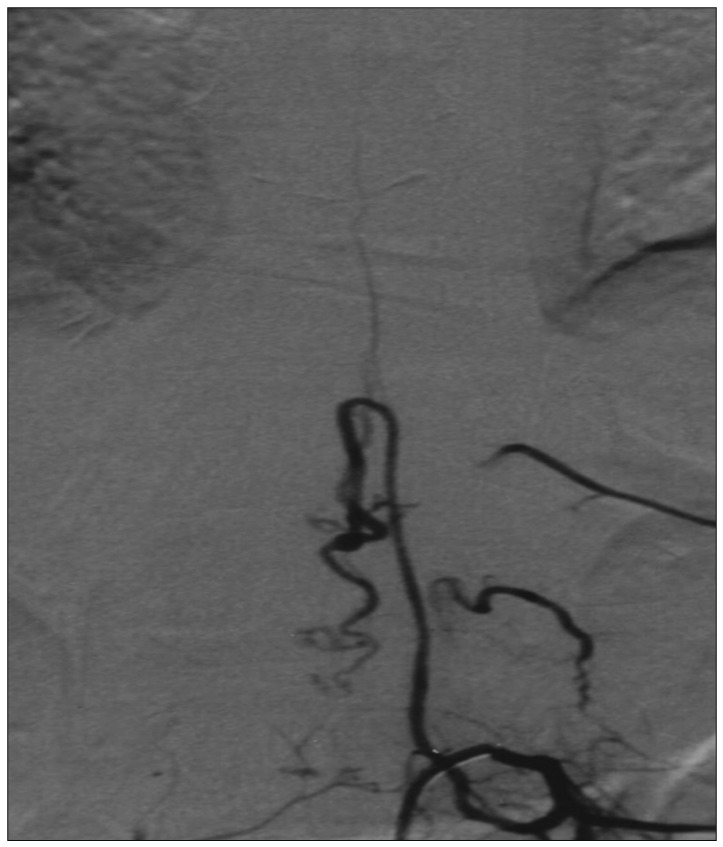
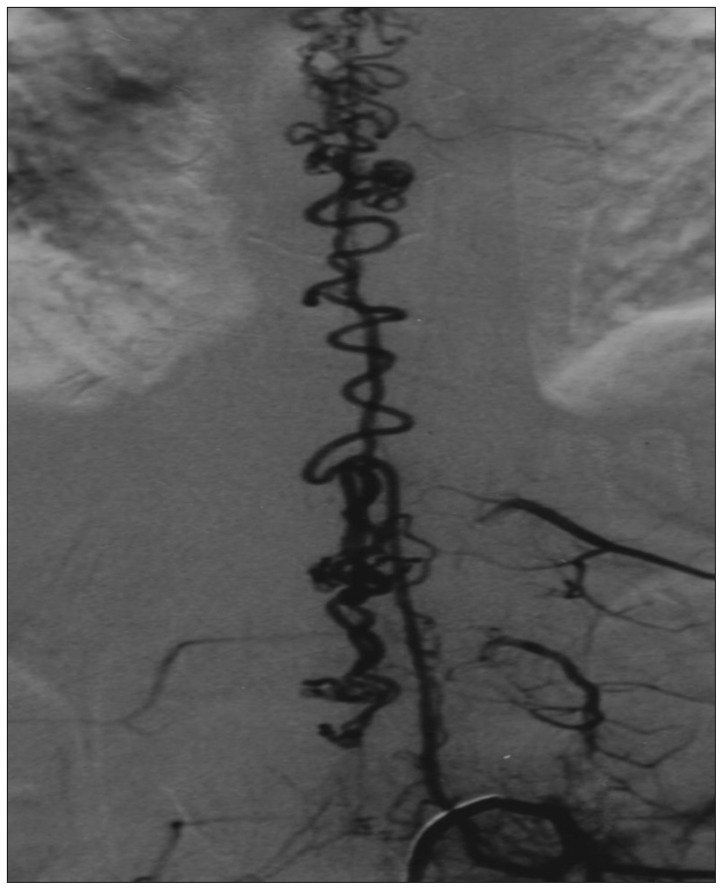
After her admission she underwent a spinal angiogram that revealed a single, direct, moderate flow, single-hole type AVF at the left first lumbar (L1) level supplied by the anterior spinal artery (ASA), which presented a small dilatation just at the shunt site (Fig. 1). The draining vein and the superficial venous network were dilated with slow flow indicating venous congestion (Fig. 2). In the same session and under general anaesthesia we approached the lesion endovascularly using a Magic 1.2 Fr microcatheter (Balt, Montmorency, France) which was advanced over a Mirage 0.008-inch guidewire (ev3, Irvine, CA, USA). A single drop of N-butyl cyanoacrylate glue 50% was delivered just at the shunt site, which resulted to a complete occlusion of the fistula (Fig. 3).
After awakening, she reported some immediate sensory improvement. Six months after the operation she was able to walk again with assistance. No complete motor recovery was achieved after one year despite of intensive rehabilitation.
It has been years since spinal anaesthesia has been well established as a safe method over a series of reported studies. Neurological complications of the lumbar puncture, though rare, represent a constant source of concern for the anaesthesiologist as they can lead to permanent deficits6). The incidence of neurologic injury with a permanent deficit is reported between 0.015 and 0.07% whereas transient deficits are more common (0.01 to 0.8%)2,5,7).
As far as the type and mechanism of the neurological complication is concerned, there are several reports in the literature describing cases of unintended subdural injection, extradural or intradural spinal haematomas causing compression of the spinal cord or the nerve roots, infection with or without abscess, direct trauma of the cord or nerve, neurotoxicity due to the injected anaesthetic1,2,3,5,7,11,12,14,15,16,17,22).
Most of the purely iatrogenic reports have involved either some difficulty during lumbar puncture or multiple attempts to reach the subarachnoid space. Selection of high lumbar or thoracic intervertebral spaces for access to the subarachnoid or epidural spaces may lead to inadvertent puncture of the spinal cord. Concerning our case, the evaluation of the decision making process regarding the type of anaesthesia and execution is beyond the scope of this report.
Rajakulendran et al.17) reported a case of traumatic damage of the cord by the spinal needle. Pradhan et al.16) described three cases of focal myelomalacia and syrinx formation due to accidental injection of lidocaine into the substance of the spinal cord. Halbach et al.8) in their series of ten giant spinal AVFs reported one patient whose fistula cause might have been related to epidural anaesthesia traumatising a low tethered cord. This is the only case to our knowledge in the literature, which refers with uncertainty though, to the possibility of creating such a fistula as a complication of spinal anaesthesia.
Epidural or spinal anaesthesia is quite common in surgical practice. Although it represents a routine action, the procedure is by no means innocuous as it requires knowledge, proper technique and experience. Among the anatomical pitfalls are the inability to access the correct entry site and lack of awareness of structures in relation to the advancing needle4).
In our case, the immediate bilateral symptomatology suggests direct injury of the spinal cord most likely in the midline. The needle sizes used for spinal anaesthesia range from 21G to 27G with the 23G and 25G ones being the most frequent ones. Such a needle coming from the dorsal side of the cord at the T12-L1 level could injure both ASA and vein which runs dorsal to the artery and roughly parallel10). This kind of simultaneous injury after an initial phase of mostly subpial or intraspinal haematoma formation resulting by both injured vessels is possible to lead to a direct shunt later, due to the pressure gradient. A similar mechanism is involved in the fistula formation between femoral artery and vein after femoral punctures.
In our case there was no evidence of any hereditary or metameric disorder present, therefore it should fall into the group of sporadic lesions.
Spinal cord AVFs supplied by the ASA are not often characterized by large venous dilatations since the anterior spinal vein which is often the recipient vein runs subpially18). In Rodeschs' series among all spinal cord arteriovenous shunts, 20% were fistulae (1/4 macro, 3/4 micro) and most of them were single10). In the adult group, none of the micro variety was connected with any hereditary disease21). High-flow lesions tend to bleed whereas slow-flow ones tend to present with progressive ischemic syndromes secondary to venous hypertension20). The lumbar AVFs present with myelopathy, with the vast majority having progressive course with weakness, sensory changes, bowel and bladder dysfunction.
The above-mentioned features regarding location, presentation, flow pattern, rough anatomy and epidemiology fit well with our case. Nevertheless, due to its detailed morphology and particularly the small vascular dilatation just at the shunt site, we think it may correspond to the initial direct needle damage on both vessel walls. The possibility of a coincidental and independently developed, therefore unrelated to the spinal anaesthesia, spinal arteriovenous single-hole fistula seems in our opinion extremely unlike, primarily because of the elucidative and accurately described medical history, associating onset of symptoms during the spinal anaesthesia and a progressive course thereafter.
Although our case report describes an extremely rare complication, we conclude that high suspicion index is essential, especially in cases of spinal anaesthesia with symptoms suggestive of spinal cord injury or following multiple troublesome attempts of spinal anaesthesia. Early and proper investigation and intervention are necessary to prevent severe and irreversible neurologic deficits. Recovery from these kinds of vascular trauma is most likely to be incomplete.
Acknowledgements
The authors would like to thank Dr. E. A. Psatha for the critical reviewing of the manuscript.
References
1. Ahmad FU, Pandey P, Sharma BS, Garg A. Foot drop after spinal anesthesia in a patient with a low-lying cord. Int J Obstet Anesth. 2006; 15:233–236. PMID: 16798451.

2. Auroy Y, Narchi P, Messiah A, Litt L, Rouvier B, Samii K. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthesiology. 1997; 87:479–486. PMID: 9316950.
3. Birnbach DJ, Hernandez M, van Zundert AA. Neurologic complications of neuraxial analgesia for labor. Curr Opin Anaesthesiol. 2005; 18:513–517. PMID: 16534285.

4. Boon JM, Abrahams PH, Meiring JH, Welch T. Lumbar puncture: anatomical review of a clinical skill. Clin Anat. 2004; 17:544–553. PMID: 15376294.

5. Charuluxananan S, Thienthong S, Rungreungvanich M, Chanchayanon T, Chinachoti T, Kyokong O, et al. The Thai Anesthesia Incidents Study (THAI study) of morbidity after spinal anesthesia: a multi-centered registry of 40,271 anesthetics. J Med Assoc Thai. 2007; 90:1150–1160. PMID: 17624210.
6. Domenicucci M, Ramieri A, Ciappetta P, Delfini R. Nontraumatic acute spinal subdural hematoma: report of five cases and review of the literature. J Neurosurg. 1999; 91(1 suppl):65–73. PMID: 10419371.
7. Faccenda KA, Finucane BT. Complications of regional anaesthesia Incidence and prevention. Drug Saf. 2001; 24:413–442. PMID: 11368250.
8. Halbach VV, Higashida RT, Dowd CF, Fraser KW, Edwards MS, Barnwell SL. Treatment of giant intradural (perimedullary) arteriovenous fistulas. Neurosurgery. 1993; 33:972–979. discussion 979-980. PMID: 8134010.

9. LaFerlita BW. Postoperative paraplegia coincident with single shot spinal anaesthesia. Anaesth Intensive Care. 2007; 35:605–607. PMID: 18020083.

10. Lasjaunias P, Berenstein A, ter Brugge K. Surgical Neuroangiography. ed 2. Berlin: Springer-Verlag;2004. p. 767–813.
11. Likar R, Mathiaschitz K, Spendel M, Krumpholz R, Martin E. [Acute spinal subdural hematoma after attempted spinal anesthesia]. Anaesthesist. 1996; 45:66–69. PMID: 8678281.
12. Liu YC, Wu RS, Wong CS. Unexpected complication of attempted epidural anaesthesia: cauda equina syndrome. Anaesth Intensive Care. 2003; 31:461–464. PMID: 12973972.

13. Niimi Y, Berenstein A. Endovascular treatment of spinal vascular malformations. Neurosurg Clin N Am. 1999; 10:47–71. PMID: 9855649.

14. Paech MJ, Godkin R, Webster S. Complications of obstetric epidural analgesia and anaesthesia: a prospective analysis of 10,995 cases. Int J Obstet Anesth. 1998; 7:5–11. PMID: 15321239.

15. Pogatzki-Zahn EM, Wenk M, Wassmann H, Heindel WL, Van Aken H. [Complications of regional anesthesia: diagnostic and management]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2007; 42:42–52. PMID: 17253336.
16. Pradhan S, Yadav R, Maurya PK, Mishra VN. Focal myelomalacia and syrinx formation after accidental intramedullary lidocaine injection during lumbar anesthesia: a report of 3 cases. J Neurol Sci. 2006; 251:70–72. PMID: 17097107.

17. Rajakulendran Y, Rahman S, Venkat N. Long-term neurological complication following traumatic damage to the spinal cord with a 25 gauge whitacre spinal needle. Int J Obstet Anesth. 1999; 8:62–66. PMID: 15321178.

18. Rodesch G, Hurth M, Alvarez H, David P, Tadie M, Lasjaunias P. Embolization of spinal cord arteriovenous shunts: morphological and clinical follow-up and results--review of 69 consecutive cases. Neurosurgery. 2003; 53:40–49. discussion 49-50. PMID: 12823872.

19. Rodesch G, Hurth M, Alvarez H, Lasjaunias P. Embolisation of Spinal Cord Arteriovenous Malformations with Glue through the Anterior Spinal Axis. Review of 20 Cases. Interv Neuroradiol. 1997; 3:131–143. PMID: 20678351.

20. Rodesch G, Hurth M, Alvarez H, Tadié M, Lasjaunias P. Classification of spinal cord arteriovenous shunts: proposal for a reappraisal--the Bicêtre experience with 155 consecutive patients treated between 1981 and 1999. Neurosurgery. 2002; 51:374–379. discussion 379-380. PMID: 12182775.

21. Rodesch G, Hurth M, Alvarez H, Tadie M, Lasjaunias P. Spinal cord intradural arteriovenous fistulae: anatomic, clinical, and therapeutic considerations in a series of 32 consecutive patients seen between 1981 and 2000 with emphasis on endovascular therapy. Neurosurgery. 2005; 57:973–983. discussion 973-983. PMID: 16284566.

22. Sorenson EJ. Neurological injuries associated with regional anesthesia. Reg Anesth Pain Med. 2008; 33:442–448. PMID: 18774513.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download