Abstract
Objective
The aim of this study was to evaluate effect of pulsed radiofrequency (PRF) neuromodulation of suprascpaular nerve (SSN) in patients with chronic shoulder pain due to adhesive capsulitis and/or rotator cuff tear.
Methods
The study included 11 patients suffering from chronic shoulder pain for at least 6 months who were diagnosed with adhesive capsulitis (n=4), rotator cuff tear (n=5), or adhesive capsulitis+rotator cuff tear (n=2) using shoulder magnetic resonance imaging or extremity ultrasonography. After a favorable response to a diagnostic suprascapular nerve block twice a week (pain improvement >50%), PRF neuromodulation was performed. Shoulder pain and quality of life were assessed using a Visual Analogue Scale (VAS) and the Oxford Shoulder Score (OSS) before the diagnostic block and every month after PRF neuromodulation over a 9-month period.
Results
The mean VAS score of 11 patients before PRF was 6.4±1.49, and the scores at 6-month and 9 month follow-up were 1.0±0.73 and 1.5±1.23, respectively. A significant pain reduction (p<0.001) was observed. The mean OSS score of 11 patients before PRF was 22.7±8.1, and the scores at 6-month and 9 month follow-up were 41.5±6.65 and 41.0±6.67, respectively. A significant OSS improvement (p<0.001) was observed.
Shoulder pain is the second most common musculoskeletal disorder in adults over their lifetime15). Shoulder disorders are often accompanied by acute, sub-acute, or chronic pain, and limited range of motion (ROM)14,16). Limited ROM of the shoulder joint affects upper extremity joint function and quality of life. Effective management of shoulder pain demands a multidirectional approach including medication, physical therapy, rehabilitation, surgical procedures, and selective nerve block for local pain control7,8). Reduction of painful protective muscle spasms and modulation of afferent input and motor control may be facilitated by suprascapular nerve blockade (SSNB)21). If the short-term effect of peripheral nerve block using local anesthetics is not sufficient, other techniques may be used for long-term pain relief. Several case studies have reported a favorable outcome for pulsed radiofrequency (PRF) neuromodulation to the suprascapular nerve (SSN)10,18,20). In this study, we present the clinical outcomes of 11 patients with chronic shoulder pain treated using PRF neuromodulation.
From September 2010 to April 2011, 18 patients who had significant chronic shoulder pain for at least 6 months who were unresponsive to medication and intra-articular injections and were not considered surgical candidates were included in this study. All diagnoses were confirmed using ultrasonography or magnetic resonance imaging (MRI). All patients received diagnostic SSNB using 1.0% lidocaine and dexamethasone twice a week. Temporary pain relief of >50% or improvement in ROM was considered a positive response to the diagnostic nerve block. Of the 18 patients, 11 showed a positive response. These patients underwent PRF neuromodulation of the SSN for chronic shoulder pain. Clinical data were obtained from a review of the patients' medical records.
The PRF procedure was performed in the operating room under fluoroscopy using a NeuroTherm NT1000 (NeuroTherm Inc., Middleton, MA, USA) radiofrequency generator. The C-arm was oblique about 10-20° and angled cephalo-caudad about 10-20°. The suprascapular notch was easily identified superior to the scapular spine, medial to the coracoids process, and lateral to the rib margins.
The scapula area was aseptically draped with sterile towels. The skin was anesthetized with 5% lidocaine gel. The spine of the scapula was located, and a line was drawn along it from the tip of the acromion to the medial scapular border. The midpoint of the line was determined and a vertical line parallel to the spine of the vertebral column was drawn through it. The angle of the upper outer quadrant was bisected with a line, and an X was marked on the line 1 cm from the apex of this angle (Fig. 1). A disposable 22-gauge, 15-cm radiofrequency cannula (Model S-1505, NeuroTherm Inc.) with a 5-mm active tip was inserted at this point perpendicular to the skin in all planes. The author confirmed the correct needle tip relative to the suprascapular notch by fluoroscopic images. The introducer needle was withdrawn and the disposable RF electrode (Model RFDE-15, NeuroTherm Inc.) was advanced. Sensory stimulation (50 Hz) was performed after the needle tip penetrated the suprascapular notch. Sensory stimulation at 50 Hz was performed and reproducible paresthesias in the shoulder joint occurred at a voltage ≤0.3 V. Motor stimulation at 2 Hz was performed and contractions of the infraspinatus and supraspinatus muscles occurred at 0.4 V. After positive stimulation, PRF neuromodulation was performed for a total of 240 pulses at 50 V during which the temperature at the needle tip was not permitted to exceed 42℃.
In all patients, pain was assessed prior to the diagnostic block and once per month following the PRF neuromodulation procedure by the same physician who performed the initial pain and shoulder function assessments. A Visual Analogue Scale (VAS) (0 cm-no pain; 10 cm-worst possible pain imaginable) and the Oxford Shoulder Score (OSS) test13) were administered following the pre-diagnostic block and once a month following PRF neuromodulation. The OSS is a condition-specific questionnaire with pain and function questions that assesses the impact of shoulder pain on daily life during the past four weeks.
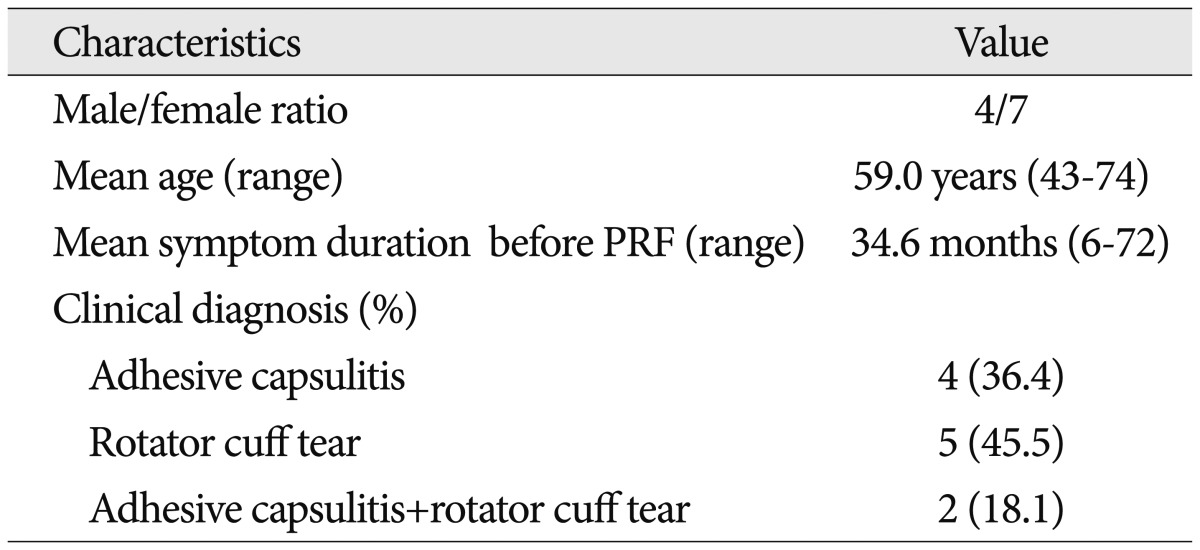
The study included 11 patients [four males (36.4%) and seven females (63.6%)] aged 43 to 74 years (mean, 59 years). All patients were diagnosed using shoulder MRI scans or ultrasonography. The diagnoses were rotator cuff tear in five patients (45.5%), adhesive capsulitis in four (36.4%), and rotator cuff tear with adhesive capsulitis in two patients (18.1%). The mean symptom duration was 34.6 months (range, 6-72 months). Clinical follow ups were conducted at 6 and 9 months post-PRF neuromodulation (Table 1).
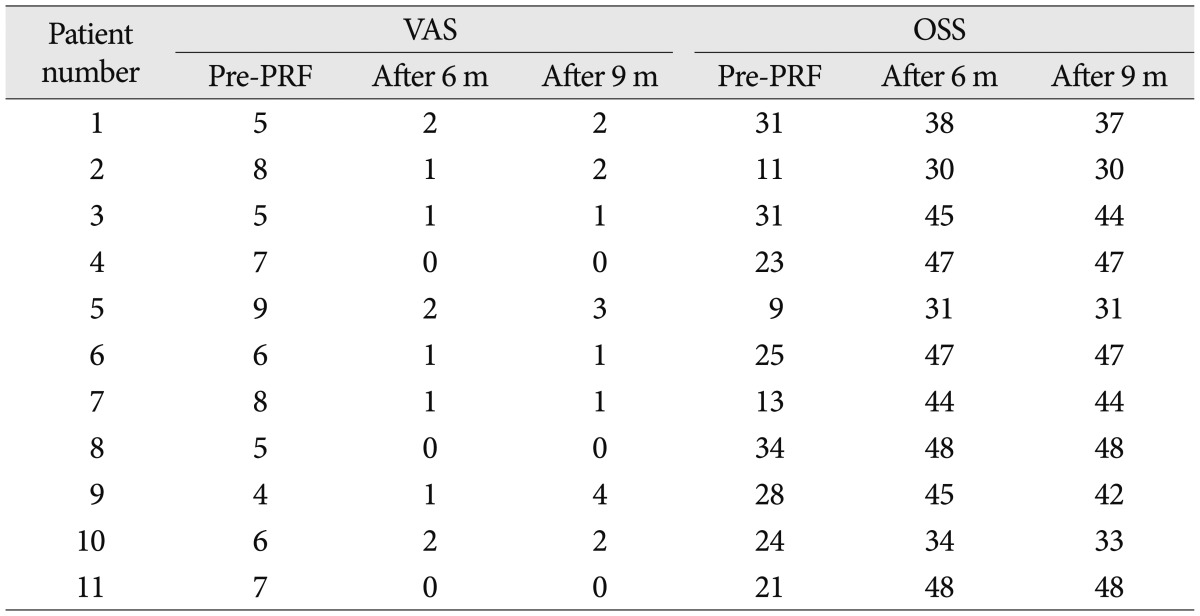
Treatment outcomes following PRF neuromodulation are shown in Table 2. At the 6-month follow up, all patients reported significant pain relief (VAS, ≥50% reduction in pain), and at the 9-month follow up, 10 patients (90.9%) reported significant pain relief (p<0.001). At the 6- and 9-month follow ups, seven patients (63.6%) reported a significant improvement in shoulder function (OSS score ≥40). No complications were reported.
Mean VAS and OSS scores are shown in Table 3. The VAS and OSS scores at the 6- and 9-month follow up assessments showed significant improvements in pain and function compared with the pre-diagnostic block scores (p<0.001) (Table 3). The mean pre-diagnostic block VAS score of 6.4±1.49 decreased to 1.0±0.73 and 1.5±1.23 at 6 and 9 months following the PRF procedure, respectively (both p<0.001). The mean pre-diagnostic block OSS score was 22.7±8.1 and increased to 41.5±6.65 and 41.0±6.67 at the 6- and 9-month follow-up assessments, respectively (both p<0.001).
The SSN has become a target for intervention because of its extensive sensory nerve supply to the shoulder structures, including the posterior glenohumeral joint capsule, acromioclavicular joint, subacromial bursa, and coracoclavicular ligament1). SSNB has been investigated in various types of chronic shoulder pain disorders3). Moreover, SSNB has a long history of reducing pain and improving ROM in patients with shoulder pain including rotator cuff lesions and frozen shoulder2,4,17,21,23). Several studies have reported that SSNB provides significant and sustained pain relief and improvement in disability scores and ROM in degenerative disease and conditions that are inflammatory in origin21). However, the effects of SSNB are short term, and although pain relief may be prolonged by steroids, long-lasting pain reduction exceeding 12 weeks has not been reported6,21,23).
Our results indicate that PRF neuromodulation of the suprascapular nerve improved pain and function in patients with intractable chronic shoulder pain. Of the 11 patients who underwent the procedure, 10 reported significant pain relief lasting 9 months. These findings have important clinical implications because chronic shoulder pain is debilitating and difficult to treat. At present, the evidence is not sufficient to support or refute the efficacy of traditional shoulder pain treatments9). Medical treatments such as simple analgesia, non-steroidal anti-inflammatory drugs, and physical therapy, rehabilitation, intra-articular steroid injection, and surgery have limitations21).
RF treatment of SSN may be an alternative method of providing prolonged relief for chronic shoulder pain12). Conventional RF treatment destroys nerve tissue, thus preventing the propagation of pain signals and providing sustained pain relief19). However, irreversible neural tissue damage may occur at temperatures above 45℃22).
Unlike conventional RF treatment, PRF neuromodulation makes rapid changes in strong electric fields and can lead to alteration of pain signal and pain relief. Moreover, temperatures do not exceed 42℃ during the procedure, and the target nerves and surrounding tissue are not damaged. Thus, the risk of neural damage and neuritis is reduced in the PRF neuromodulation procedure compared with conventional RF treatment5,11,19).
Few studies have investigated the effect of PFR neuromodulation for shoulder pain12). Shah and Racz20) described the case of a patient with severe post-traumatic pain who received repeated PRF neuromodulation on the suprascapular nerve. The patient reported pain relief lasting up to 4 weeks. Gurbet et al.10) found that PRF neuromodulation on the SSN of eight patients with chronic shoulder pain caused by rotator cuff tear had a beneficial effect for up to 3 months. In the present study, patients with adhesive capsulitis and/or rotator cuff tear reported a significant reduction in pain (VAS score) and improvement in shoulder function increasing the life of quality (OSS score)13) lasting more than 9 months following PRF neuromodulation. The results of our study suggest that PRF neuromodulation of the SSN may improve chronic shoulder pain of various origins for a relatively long period. Furthermore, PRF neuromodulation is minimally invasive and has no serious adverse effects.
Our study has some limitations. First, although the VAS and OSS are proven tools for the quantification of pain, they are subjective outcome measures because they may vary according to individual interpretations. Second, the small sample size limits the strength and generalizability of our observations.
Acknowledgements
This study was supported by Hallym University Research Fund 2013 (HURF-2013-07) and BioGreen21 Program (PJ009051) of Rural Development Administration
References
1. Aszmann OC, Dellon AL, Birely BT, McFarland EG. Innervation of the human shoulder joint and its implications for surgery. Clin Orthop Relat Res. 1996; (330):202–207. PMID: 8804294.

2. Carron H. Relieving pain with nerve blocks. Geriatrics. 1978; 33:49–57. PMID: 147196.
3. Chan CW, Peng PW. Suprascapular nerve block : a narrative review. Reg Anesth Pain Med. 2011; 36:358–373. PMID: 21654552.
4. Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G. A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block : an evaluation of the first results. Arthroscopy. 2008; 24:689–696. PMID: 18514113.

5. Choi HJ, Choi SK, Kim TS, Lim YJ. Pulsed radiofrequency neuromodulation treatment on the lateral femoral cutaneous nerve for the treatment of meralgia paresthetica. J Korean Neurosurg Soc. 2011; 50:151–153. PMID: 22053239.

6. Dahan TH, Fortin L, Pelletier M, Petit M, Vadeboncoeur R, Suissa S. Double blind randomized clinical trial examining the efficacy of bupivacaine suprascapular nerve blocks in frozen shoulder. J Rheumatol. 2000; 27:1464–1469. PMID: 10852272.
7. Emery P, Bowman S, Wedderburn L, Grahame R. Suprascapular nerve block for chronic shoulder pain in rheumatoid arthritis. BMJ. 1989; 299:1079–1080. PMID: 2511970.

8. Gado K, Emery P. Modified suprascapular nerve block with bupivacaine alone effectively controls chronic shoulder pain in patients with rheumatoid arthritis. Ann Rheum Dis. 1993; 52:215–218. PMID: 8484675.

9. Green S, Buchbinder R, Glazier R, Forbes A. Systematic review of randomised controlled trials of interventions for painful shoulder : selection criteria, outcome assessment, and efficacy. BMJ. 1998; 316:354–360. PMID: 9487172.

10. Gurbet A, Türker G, Bozkurt M, Keskin E, Uçkunkaya N, Sahin S. [Efficacy of pulsed mode radiofrequency lesioning of the suprascapular nerve in chronic shoulder pain secondary to rotator cuff rupture]. Agri. 2005; 17:48–52. PMID: 16158343.
11. Hagiwara S, Iwasaka H, Takeshima N, Noguchi T. Mechanisms of analgesic action of pulsed radiofrequency on adjuvant-induced pain in the rat : roles of descending adrenergic and serotonergic systems. Eur J Pain. 2009; 13:249–252. PMID: 18539061.

12. Luleci N, Ozdemir U, Dere K, Toman H, Luleci E, Irban A. Evaluation of patients' response to pulsed radiofrequency treatment applied to the suprascapular nerve in patients with chronic shoulder pain. J Back Musculoskelet Rehabil. 2011; 24:189–194. PMID: 21849733.

13. Olley LM, Carr AJ. The use of a patient-based questionnaire (the Oxford Shoulder Score) to assess outcome after rotator cuff repair. Ann R Coll Surg Engl. 2008; 90:326–331. PMID: 18492399.

14. Parsons S, Breen A, Foster NE, Letley L, Pincus T, Vogel S, et al. Prevalence and comparative troublesomeness by age of musculoskeletal pain in different body locations. Fam Pract. 2007; 24:308–316. PMID: 17602173.

15. Picavet HS, Schouten JS. Musculoskeletal pain in the Netherlands : prevalences, consequences and risk groups, the DMC(3)-study. Pain. 2003; 102:167–178. PMID: 12620608.

16. Rechardt M, Shiri R, Karppinen J, Jula A, Heliövaara M, Viikari-Juntura E. Lifestyle and metabolic factors in relation to shoulder pain and rotator cuff tendinitis : a population-based study. BMC Musculoskelet Disord. 2010; 11:165. PMID: 20646281.
17. Ritchie ED, Tong D, Chung F, Norris AM, Miniaci A, Vairavanathan SD. Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery : a new modality? Anesth Analg. 1997; 84:1306–1312. PMID: 9174311.

18. Rohof OJ. Radiofrequency treatment of peripheral nerves. Pain Pract. 2002; 2:257–260. PMID: 17147740.

19. Rozen D, Parvez U. Pulsed radiofrequency of lumbar nerve roots for treatment of chronic inguinal herniorraphy pain. Pain Physician. 2006; 9:153–156. PMID: 16703977.
20. Shah RV, Racz GB. Pulsed mode radiofrequency lesioning of the suprascapular nerve for the treatment of chronic shoulder pain. Pain Physician. 2003; 6:503–506. PMID: 16871304.
21. Shanahan EM, Ahern M, Smith M, Wetherall M, Bresnihan B, FitzGerald O. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Ann Rheum Dis. 2003; 62:400–406. PMID: 12695149.

22. Van Zundert J, de Louw AJ, Joosten EA, Kessels AG, Honig W, Dederen PJ, et al. Pulsed and continuous radiofrequency current adjacent to the cervical dorsal root ganglion of the rat induces late cellular activity in the dorsal horn. Anesthesiology. 2005; 102:125–131. PMID: 15618796.

23. Vecchio PC, Adebajo AO, Hazleman BL. Suprascapular nerve block for persistent rotator cuff lesions. J Rheumatol. 1993; 20(3):453–455. PMID: 8478851.
Fig. 1
C-arm fluoroscopy image of pulsed radiofrequency neuromodulation showing fluoroscopy landmarks for the suprascapular nerve (asterix), which is located in the suprascapular notch (white curved line) at the midpoint of the scapular spine (white straight line).

Table 1
Characteristics of patients who underwent pulsed radiofrequency neuromodulation for chronic shoulder pain




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download