Abstract
Lymphomatosis cerebri is considered a diffuse form of primary central nervous system lymphoma and very rare. It is not well recognized and may be misdiagnosed with infiltrating tumors, degenerative disorders, ischemic diseases, and infectious diseases developed in the brain. Awareness of the possibility of this rare disease and early biopsy are required for differential diagnosis and preventing poor clinical outcomes. We report a case with lymphomatosis cerebri who presented with rapid neurological deteriorations and review the relevant literatures.
Primary central nervous system lymphoma (PCNSL) is hematopoetic tumors that is usually restricted to the central nervous system5,7). It is well known that PCNSL presents as one or more discrete, well-enhancing lesions on magnetic resonance image (MRI). Meanwhile, lymphmatosis cerebri refers to the extensive, diffuse infiltrations of both cerebral hemispheres by lymphoma cells without discernible lesions9,11). It has been reported less than 20 cases up to now8). It is poorly recognized as a very rare variant of PCNSL and misdiagnosis resulting in delayed treatment may occur. We present a case with biopsy-proven lymphomatosis cerebri who had experienced rapid deteriorations of higher brain functions and review the relevant literatures.
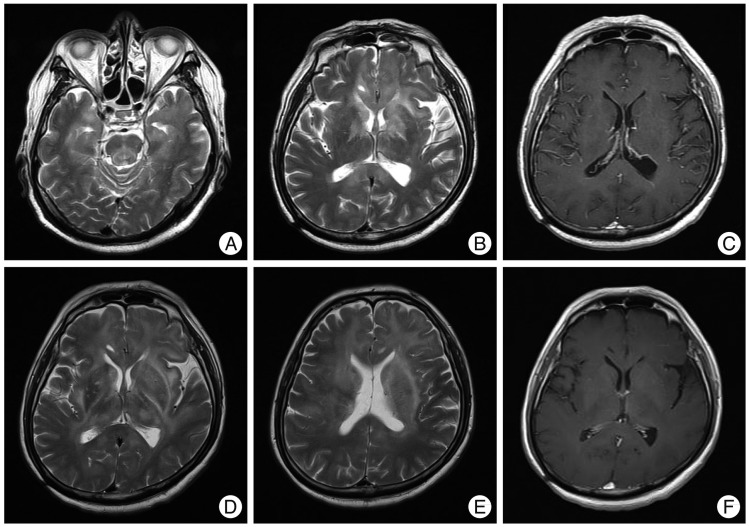
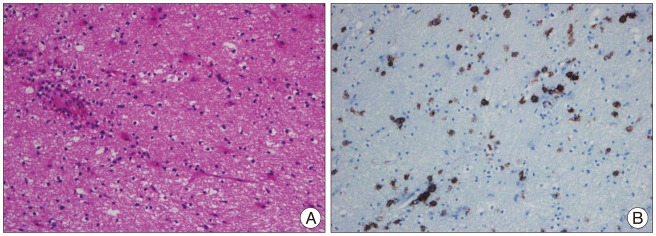
A 64-year-old male patient presented with gait disturbance and slowness of behavior. At another hospital, cerebrospinal fluid (CSF) analysis and cytology were performed to differentiate several diseases such as ischemic diseases, infectious diseases, infiltrative tumors, and neurodegenerative disorders. But, there were no positive results among the tested. Conservative treatments including antiplatelet drug without steroids under the impression of ischemic diseases were applied for about 2 months. However, his neurological symptoms were aggravated gradually and cognitive functions declined too. He was transferred to our hospital for further evaluation. On neurological examinations, he was drowsy deeply and obeyed only simple commands. He could not stand by himself, even sitting. Kanofsky performance status (KPS) score was 30. He was severely disabled and needed special cares for daily living activities. We had reviewed the clinical data including several images taken from outside meticulously. Brain computed tomography (CT) revealed no specific findings. Brain MRIs showed extensive, diffuse hyper-intense lesions without enhancement involving bilateral cerebral hemispheres and brainstem on both T2 and fluid attenuated inversion recovery (FLAIR)-weighted MRIs (Fig. 1A-C). MR angiograms were normal. Follow-up brain MRIs taken from our hospital revealed further progression of T2 and FLAIR hyper-intense lesions involving the gray and white matters together extending into both thalamus and periventricular deep white matters (Fig. 1D, E). Definite focal enhancement lesions were not seen on enhanced T1-weighted MRI (Fig. 1F). Initially, infiltrative tumors such as gliomatosis cerebri were suspected. Since it was difficult to confirm diagnosis with those clinical studies only, a stereotactic biopsy was performed for pathological diagnosis. Two separated targets to avoid false-negative results were selected. One was the lesion within the deep white matter of left frontal lobe and the other was the lesion close to the left frontal horn which showed brighter T2 signal intensity than first one. Both separated targets for biopsy were targeted on the T2 and FLAIR images. Scattered atypical lymphocytes and perivascular lymphoid cells were found in the two specimens. These tumor cells were strongly immunoreactive with CD20 which was consistent with diffuse large B lymphoma (Fig. 2). Despite subsequent high dose corticosteroids for 1 week, there were no further neurological improvements up to 3 months.
Lymphomatosis cerebri is considered as a rare variant of PCNSL. It has been reported to be less than 20 cases in the literatures and their clinical outcome is very poor. Most reported cases died within 6-12 months after the onset4,6-8). The patient with lymphomatosis cerebri may have variable clinical symptoms such as gait disturbance, focal weakness, decline of cognitive functions, memory disturbance, personality changes, dementia, anorexia, orthostatic hypotension, paraparesis and weight loss7,8). Our case presented with gait disturbance and behavioral changes initially. And then, gradual declines of verbal communication and cognitive functions were developed. In the neurosurgical field, clinical symptoms such as weight loss, personality changes, dementia are unusual and may lead to diagnostic confusion. The tumors infiltrating to the diencephalon have been reported to cause the diencephalic syndrome which is characterized by profound emaciation despite normal caloric intake2). Our case did not present with diencephalic syndrome although bilateral diencephalic involvements were seen on T2 and FLAIR-weighted MRIs. Typical MR findings of the lymphomatosis cerebri are extensive, diffuse T2 and FLAIR-weighted hyper-intense lesions without contrast enhancement in both cerebral hemispheres and brainstem7). However, subtle or patchy enhancements may be seen in some cases8,10). These radiological findings may be similar with those of the gliomatosis cerebri which has to be differentiated in this case. In the gliomatosis cerebri, T1-weighted hypo-intense lesions on MRIs, low-density lesions on CT, and focal enhancements are typical radiological findings3). Our case showed extensive, diffuse T2 and FLAIR-weighted hyper-intense lesions in both periventricular deep white matters, basal ganglia, diencephalon, and brainstem on MRIs. And, the abnormal lesion was centrally located and symmetrical in gray and white matters of both cerebral hemispheres. It was not useful to differentiate the abnormal lesions from normal regions on brain CT and T1-weighted MRIs.
PCNSL achieves a response rate of 90% and median survival of 60 months with high dose methotrexate-based chemotherapy1). However, the prognosis of lymphomatosis cerebri is worse than that of PCNSL despite corticosteroids, chemotherapy, and radiotherapy although there was a report with successful result6,8). In the literatures, there were little cases who underwent the established treatments for PCNSL fully and most of them had already suffered from prolonged neuropsychological symptoms over several months before accurate diagnosis and proper treatment7,8). Lymphomatosis cerebri has been considered a diagnostic challenge. It is thought that vague clinico-radiological findings and lack of awareness about lymphomatosis cerebri may delay the early diagnosis. Optimal treatment for lymphomatosis cerebri remains unclear. However, better outcomes may be expected than previously reported ones because lymphomatosis cerebri is identical to PCNSL pathologically. In our case, his medical condition was not enough to tolerate chemo-radiotherapy and we could carry out only steroid trial. Therefore, the possibility of being lymphomatosis cerebri should be kept in mind not to defer the early biopsy for accurate diagnosis and proper treatment if diffuse white matter lesions are seen on MRIs. As suspected of lymphomatosis cerebri, corticosteroids with cytotoxic effect about lymphoma cells should be delayed and multiple, separated biopsies should be performed to avoid false-negative biopsy results.
References
1. Abrey LE, Yahalom J, DeAngelis LM. Treatment for primary CNS lymphoma : the next step. J Clin Oncol. 2000; 18:3144–3150. PMID: 10963643.
2. Ashworth B. Cerebral histiocytic lymphoma presenting with loss of weight. Neurology. 1982; 32:894–896. PMID: 7048129.

3. Chen S, Tanaka S, Giannini C, Morris J, Yan ES, Buckner J, et al. Gliomatosis cerebri : clinical characteristics, management, and outcomes. J Neurooncol. 2013; 112:267–275. PMID: 23341100.

4. Courtois F, Gille M, Haven F, Hantson P. Lymphomatosis cerebri presenting as a recurrent leukoencephalopathy. Case Rep Neurol. 2012; 4:181–186. PMID: 23185172.

6. Kanai R, Shibuya M, Hata T, Hori M, Hirabayashi K, Terada T, et al. A case of 'lymphomatosis cerebri' diagnosed in an early phase and treated by whole brain radiation : case report and literature review. J Neurooncol. 2008; 86:83–88. PMID: 17611716.

7. Keswani A, Bigio E, Grimm S. Lymphomatosis cerebri presenting with orthostatic hypotension, anorexia, and paraparesis. J Neurooncol. 2012; 109:581–586. PMID: 22806340.

8. Kitai R, Hashimoto N, Yamate K, Ikawa M, Yoneda M, Nakajima T, et al. Lymphomatosis cerebri : clinical characteristics, neuroimaging, and pathological findings. Brain Tumor Pathol. 2012; 29:47–53. PMID: 21927864.

9. Lewerenz J, Ding X, Matschke J, Schnabel C, Emami P, von Borczyskowski D, et al. Dementia and leukoencephalopathy due to lymphomatosis cerebri. J Neurol Neurosurg Psychiatry. 2007; 78:777–778. PMID: 17210623.

10. Raz E, Tinelli E, Antonelli M, Canevelli M, Fiorelli M, Bozzao L, et al. MRI findings in lymphomatosis cerebri : description of a case and revision of the literature. J Neuroimaging. 2011; 21:e183–e186. PMID: 20345746.
11. Rollins KE, Kleinschmidt-DeMasters BK, Corboy JR, Damek DM, Filley CM. Lymphomatosis cerebri as a cause of white matter dementia. Hum Pathol. 2005; 36:282–290. PMID: 15791573.

Fig. 1
MRI shows diffuse, poorly-circumscribed T2 hyper-intense lesions which involve the brainstem and deep regions in both cerebral hemispheres at presentation (A and B). These lesions are not enhanced with Gadolinium (C). Two months later, these lesions extend into both thalamus and periventricular deep white matters (D and E). Definite enhancement is still not noted (F).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download