Abstract
Objective
Despite several limitations, the Trauma Injury Severity Score (TRISS) is normally used to evaluate trauma systems. The aim of this study was to evaluate the preventable trauma death rate using the TRISS method in severe trauma patients with traumatic brain injury using our emergency department data.
Methods
The use of the TRISS formula has been suggested to consider definitively preventable death (DP); the deaths occurred with a probability of survival (Ps) higher than 0.50 and possible preventable death (PP); the deaths occurred with a Ps between 0.50 and 0.25. Deaths in patients with a calculated Ps of less than 0.25 is considered as no-preventable death (NP). A retrospective case review of deaths attributed to mechanical trauma occurring between January 1, 2011 and December 31, 2011 was conducted.
Results
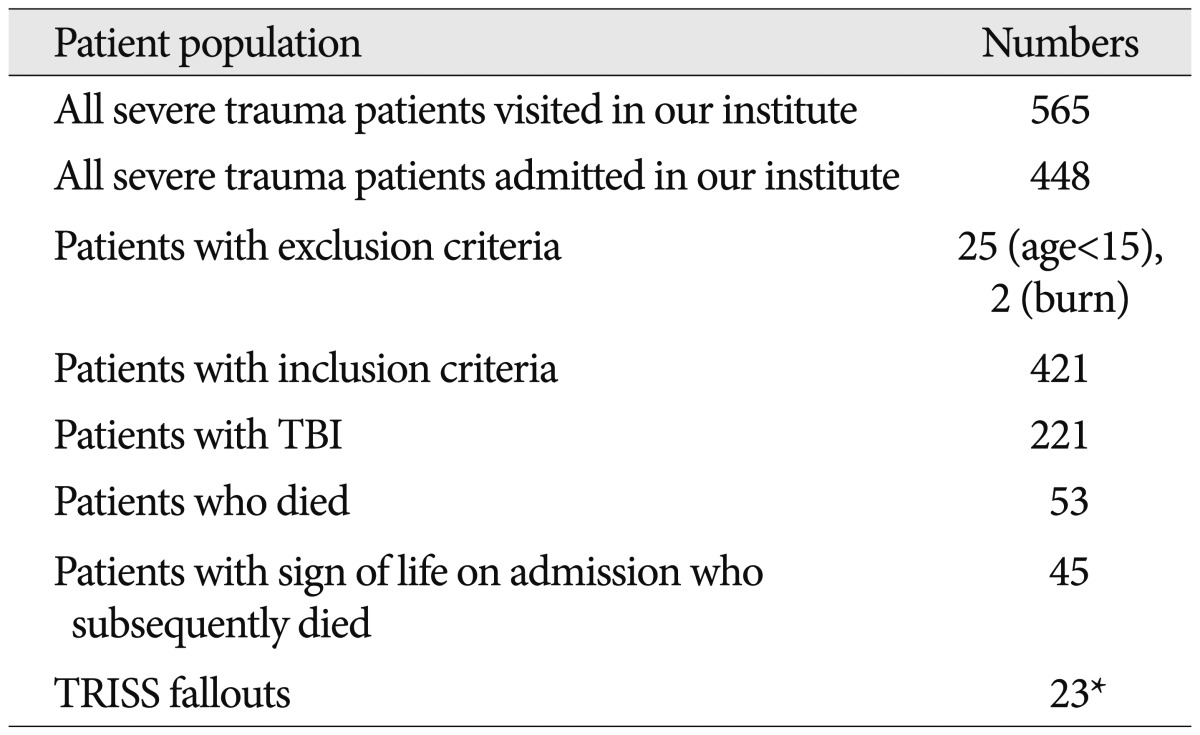
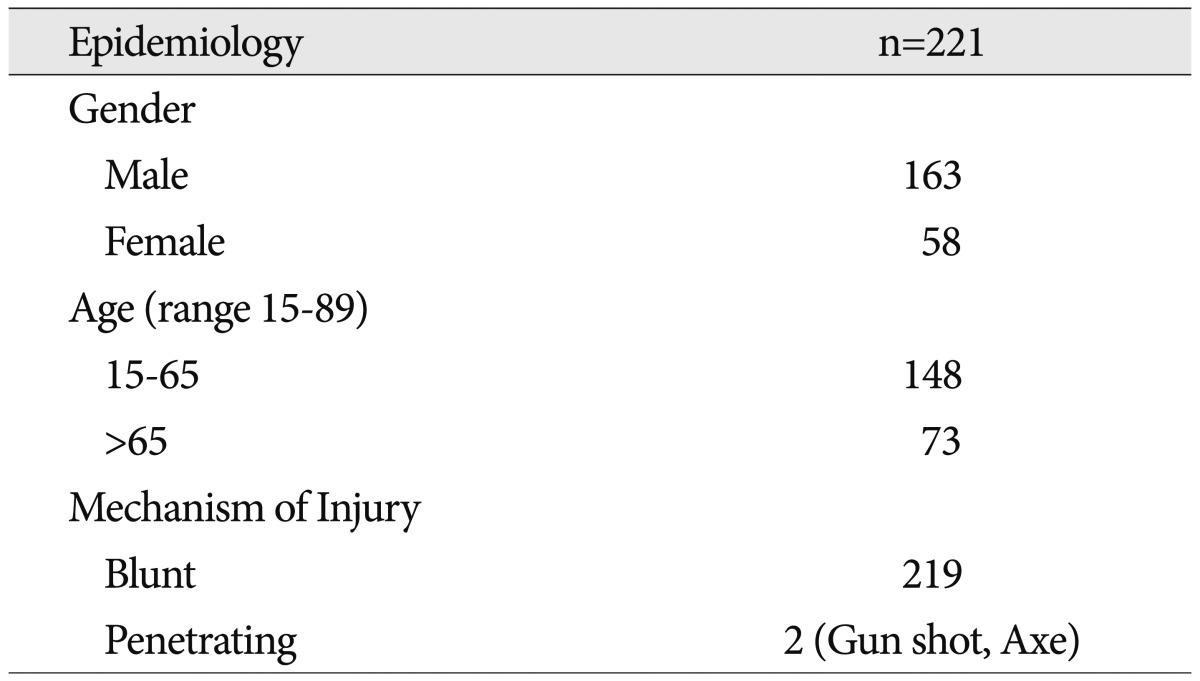
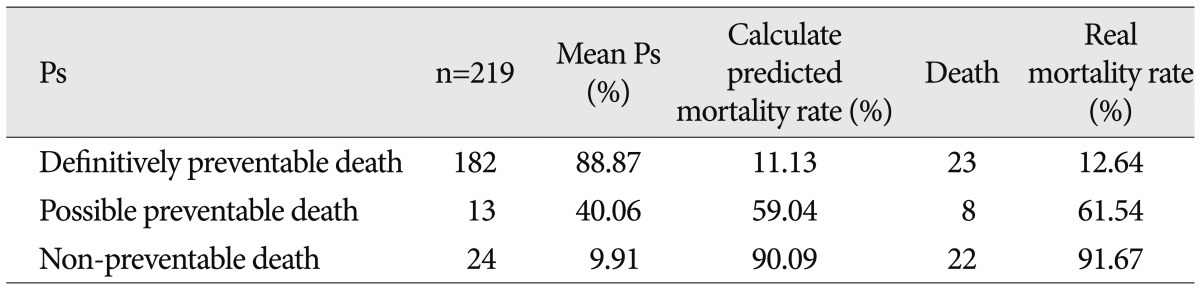
A total of 565 consecutive severe trauma patients with ISS>15 or Revised Trauma Score<7 were admitted in our institute. We excluded a total of 24 patients from our analysis : 22 patients younger than 15 years, and 2 patients with burned injury. Of these, 221 patients with head injury were analyzed in the final study. One hundred eighty-two patients were in DP, 13 in PP and 24 in NP. The calculated predicted mortality rates were 11.13%, 59.04%, and 90.09%. The actual mortality rates were 12.64%, 61.547%, and 91.67%, respectively.
Trauma is one of the most important health problems worldwide. It is a disease of the young and the leading cause of death up to the age of 4518). According to the chronological occurrence of death, trauma deaths are assorted in a tri-modal distribution. "Immediate deaths" which happen immediately after trauma are due to non-salvageable injuries. "Early deaths" occur in the first six hours and are due to conditions like continuous blood loss. "Late deaths" occur days or weeks after in the hospital and are due to sepsis or multiple organ failure5). To improve the probability of survival of immediate deaths, the pre-hospital patient transfer system is very important but, it is very difficult to establish its foundations. In order to achieve reduction of early deaths, in-hospital care as well as pre-hospital care is very important. In traumatology, improvement of survival rate focuses on reducing the number of of "early deaths", because they are deemed preventable.
Trauma scoring systems are routinely used to evaluate and monitor traumatic injury outcomes over time with a focus on reducing preventable deaths. To the best of our knowledge, no study has investigated the preventable trauma death rate using the Trauma Injury Severity Score (TRISS) method in severe trauma patients with traumatic brain injury (TBI). This study was aimed to analyze TRISS predictability among patients suffered traumatic brain injury and to compare the discrepancy between the predictive values of the TRISS model and the actual value of mortality of head trauma victims.
Trauma scoring systems are routinely used to evaluate and monitor traumatic injury outcomes over time with a focus on reducing preventable deaths. While various scoring systems exist, the TRISS is the standard method for estimating survival and assessing trauma centers7), despite its extensively documented limitations8,12). The TRISS uses a combination of patient age (AGE), Injury Severity Score (ISS) as the anatomic index and Revised Trauma Score (RTS) as the physiologic index to anticipate a patient's probability of survival following traumatic injury. The formula for the probability of survival using TRISS is :
Ps=1/(1+e-b)
Where
b=αi+βAGE,i×AGE+βRTS,i×RTS+βISS,i×ISS
with i=1 (blunt injury) or 2 (penetrating injury), αi is the constant for mechanism i, βAGE,i, βRTS,i, and βISS,i are the coefficients associated with AGE, RTS, and ISS and mechanism i, respectively. RTS is given by :
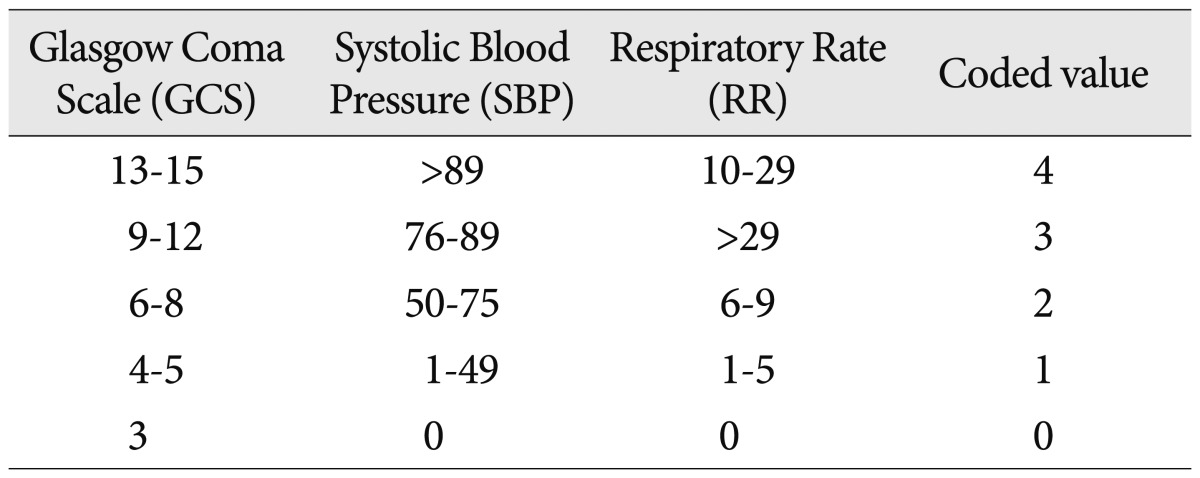
RTS=βRR×RR+βSBP×SBP+βGCS×GCS
Where βRR, βSBP, and βGCS are the coefficients associated with RR, SBP, and GCS. Substituting the formula for RTS into the equation for b gives :
b=ai+βAGE,i×AGE+βRR,i×RR+βSBP,i×SBP+βGCS,i×GCS+βISS,i×ISS
Where βRR,i, βSBP,i and βGCS,i are the coefficients associated with RR, SBP, and GCS with mechanism I, and βAGE,i and βISS,i are defined as above. The TRISS variable classifications assigned the values and coefficients derived from the MTOS in 1995 and the NTDB in 2010 (Table 1).
The ISS was calculated using the Abbreviated Injury Scores (AIS) for body regions 1-6 for individual injuries. These body regions were the head or neck, face, chest, abdomen or pelvic contents, extremities or pelvic girdle, and external. To calculate an ISS, the highest AIS severity code in each of the three most severely injured ISS body regions was needed.
ISS=(1st AIS score)2+(2nd AIS score)2+(3rd AIS score)2
The range of the ISS score is from 1 to 75; unsurvivable patients are given 75. The ISS greater than 15 is defined as major trauma4).
We conducted a retrospective case review of probability of survival (Ps) prediction models involving head trauma victims at the emergency medical center, Chonnam National University Hospital. From January 2011 to December 2011, patients who had severe traumatic injuries were registered in our database. The trauma registry maintains a database including demographics, anatomic and physiologic indices of injury severity, mechanism of injury, mode of arrival at the emergency department, timeliness of activation and response of the trauma team, timeliness of operative intervention when indicated, length to stay, survival, cause of death, etc.
The popular TRISS method calculates the Ps of a trauma patient. "TRISS fallouts", or unexpected nonsurvivors, are patients who met death despite the probability of survival on admission of >0.5. Preventable death can be divided into three categories : 1) definitively preventable death (DP) : deaths occurred with Ps>0.50, 2) possible preventable death (PP) : deaths occurred with 0.25<Ps<0.50, 3) non-preventable death (NP) : deaths occurred with 0.25<Ps. The including criteria of patients were ISS>15 and RTS≤7, restricted to adults (≥15 years old), and penetrating trauma was excluded as it happens rarely. The burn injured patients and transferred patients (do not want further treatment) were also excluded.
During the study period, a total of 565 patients with injuries due to severe trauma visited our institute. Of these, 221 patients had traumatic brain injury (39%). Fifty-three patients died at the emergency department. Eight patients were dead on arrival (no pulse, no blood pressure, no respiration; GCS=3). Of the remaining 45 patients who showed signs of life upon admission and subsequently died, 23 (51%) were TRISS fallouts (Ps>50%) (Table 2).
The average age of the brain injury group was 53.5 years (range 15-89). There were 163 men (73%) and 58 women. The most common trauma etiology was blunt injury in 219. Above mentioned, 2 patients underwent penetrating head trauma was excluded (Table 3).
The patients in DP group were 182, and the mean Ps was 88.87%. Eventually, the calculated predicted mortality rate was 11.13%. In fact, twenty-three patients died, the real mortality rate was 12.64%. The PP group had 13 patients, and the mean Ps was 40.06%. The calculated predicted mortality rate was 59.04%. Eight patients died, and the real mortality rate was 61.54%. The NP group included 24 patients, and the mean Ps was 9.91%. The calculated predicted mortality rate was 90.09%. Twenty-two patients died, and the real mortality rate was 91.67% (Table 4).
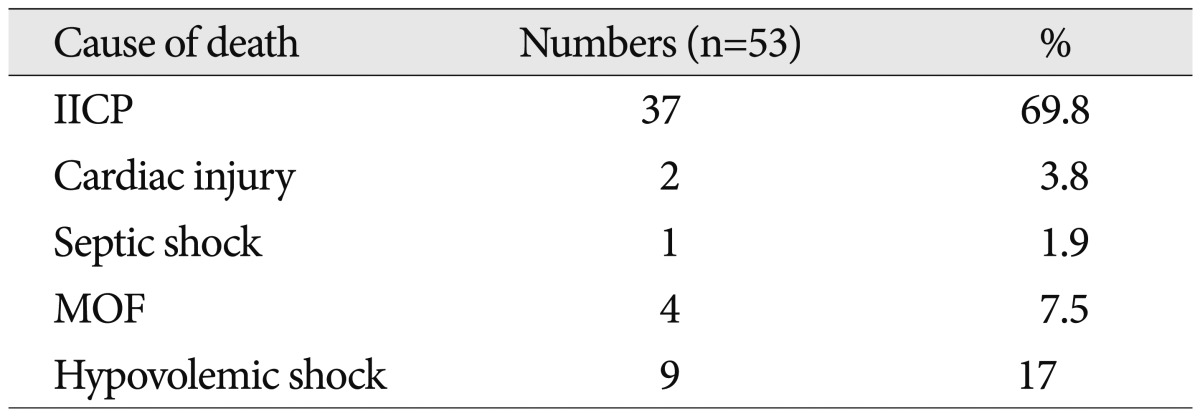
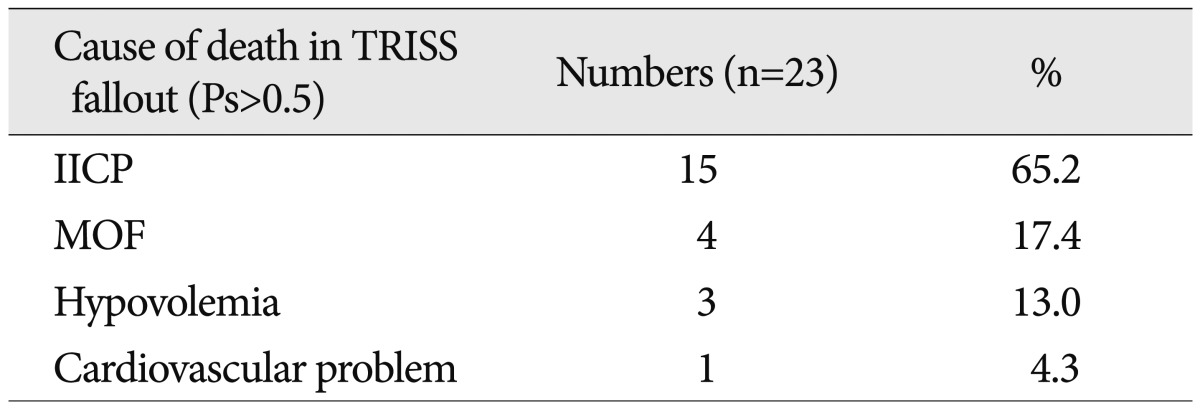
Thirty-seven patients died due to increased intracranial pressure (IICP), 9 patients due to hypovolemic shock, 4 patients due to multiple organ failure (MOF), 2 patients died due to cardiac injury and 1 patient due to septic shock (Table 5). The causes of death in TRISS fallouts (Ps>0.5) were IICP, MOF, and septic shock (Table 6).
In spite of these conformities in real and calculated mortality rates, there were discrepancies in several cases. The following two case illustrations were classified in the DP group in the current TRISS method, but the authors thought these cases were the non-DP group in the chart review.
A 67-year-old man was brought directly to our trauma center after a cultivator accident. Upon arrival at the emergency medicine department, the patient was found to have a systolic blood pressure of 150 mm Hg and a respiratory rate of 24 breaths/min and GCS of 3 (eye=1, verbal=1, motor=1). His pupils were 4/4 mm in size and did not respond to light. Also, his corneal reflex disappeared. Brain computed tomography (CT) represented a large amount of subdural hemorrhage and midline shifting from right to left (Fig. 1). His blood pressure (RTS coded value=4), respiratory rate (RTS coded value=4), and GCS (RTS coded value= 0) gave him an RTS of 4.09 (RTS=0.9368×0+0.7326×4+0.2908×4=4.09). His head and neck injuries, acute subdural hemorrhage (AIS=5) and his ISS was 25 (ISS=1st AIS2=52=25). Therefore, his calculated probability of survival by the TRISS methodology was 60.18%. During his hospital course, Brain swelling progressed and compressed the brain stem. He eventually died and was considered an unexpected nonsurvivor. If his AIS of the head and neck was given 6, his calculated probability of survival by the TRISS methodology would have decreased to 2.76%.
Another example is seen in the case of a 51-year-old man sustaining traumatic brain injury combined multiple trauma in a pedestrian accident. Upon arrival at the emergency medicine department, the patient presented a systolic blood pressure of 140 mm Hg and a respiratory rate of 0. Because his eyes were closed and he was intubated, and showed no movement to pain, he was assigned a GCS of 3. His pupils were 6/6 mm in size and not responsive to light. Also, his corneal reflex disappeared. On brain CT, severe brain swelling and global hypoxic damaged brain parenchyme (the so-called, 'whole brain infarct') was revealed (Fig. 2). His blood pressure (RTS coded value=4), respiratory rate (RTS coded value=0), and GCS (RTS coded value=0) gave him an RTS of 2.93 (RTS=0.9368×0+0.7326×4+0.2908×0=2.93). His head and neck injuries, severe brain swelling and acute subdural hemorrhage (AIS=5) and liver injury of the abdomen (AIS=2) and clavicular fracture of extremity (AIS=2) were combined to give him an ISS of 33(ISS=1st AIS2+2nd AIS2+3rd AIS2=52+22+22=33). Thus, his calculated probability of survival by the TRISS methodology was 67.48%. If his AIS of the head and neck was given 6, his calculated probability of survival by the TRISS methodology would have decreased to 6.86%.
Quality improvement is an essential component of any trauma scoring system, and outcomes have been under constant monitoring by health professionals and health organizations. Although it is difficult to imagine predicting life or death using a mathematical formula, a common consensus was that an objective and comparable method was needed to measure the outcomes and results from different trauma centers. In the initial phase, studies on preventable trauma deaths involved panel reviews of prehospital courses and hospital charts. However, reliability and validity of agreements were under debate. After the initial phase, multidisciplinary peer-review outcome analysis was conducted. The TRISS methodology was developed by Champion and Sacco in the 1980s6). After serial trials and revisions, computer-generated TRISS probability of survival date has been in wide use. TRISS has become a standard component of the quality control process in most trauma centers.
Subsequent studies reported several limitations of TRISS. In 1991, Cayten et al.2) identified some limitations. They revealed 1) the inability of TRISS to account for multiple severe injuries to a single body part, 2) the inability to predict survival in low falls, 3) the lack of distinction between gunshot and knife injuries19), and the inability to take into account pre-existing conditions and underestimation of the effects of age and head injuries. Since then, physicians have attempted to improve TRISS, and revised the coefficients as well as introduced new or modified variables in 1995 and 20106,12,17).
In our study, the mean TRISS probability of survival was 72.9%, and thus, the predicted death rate was 27.1%. The actual mortality rate of TBI was 23.4%. These two results relatively coincided. Therefore, the predicted value of TRISS can be considered as a simple and time-saving evaluation tool at trauma centers.
However, this discrepancy was not negligible; it was probably developed under the expectation of unexpected nonsurvivors. Possible explanations are inappropriate emergency transporting systems, inappropriate emergency care at the trauma center, and inaccurate prediction of the TRISS method. The first two factors can be improved by supplementation of the infrastructure. Regarding the prediction of survival rate, as aforementioned, the TRISS method was based on RTS and ISS. Physiologic responses to injury are measured by the RTS14,15), and anatomic injury severity is represented by the ISS in the TRISS model16). The RTS and ISS were documented the limits9,10,19). In particular, the ISS, anatomic injury indicator has some problems. The ISS does not account for multiple injuries to the same body region or fatal damage to internal organs, such as severe TBI. In fact, two severe injuries to the same body region may have lowered the calculated score than two moderate injuries to different body regions. However, fatal injury to the brain is the major cause of morbidity and mortality. More than 35% of traumatic deaths are attributed to TBI1).
With the above mentioned examples, we presented the cases with overestimation of probability of survival in TBI patients. To improve the prediction, pupil dilatation or loss of pupil response to light can be included in RTS. In case of effacement of ventricle or brainstem cistern due to severe brain swelling, beside both pupil dilated, but was calculated as 5 in ISS, it could be changed to 6. Actually, if patients' AIS of the head and neck was 6, not 5, the discrepancies between the actual and predicted survival of TRISS were closed a gap. As described earlier, Champion et al.3) found it superior to TRISS in predicting survival when they included the scores of all anatomic injuries and reflected the severity of trauma.
From an emergency neurosurgeon's standpoint, in order to evaluate TBI in the acute setting, noncontrast CT is the modality of choice due to its convenience and accuracy. CT readily identifies intracranial hemorrhage and brain swelling. On imaging, significant midline shift, cerebral herniation sign, evidence of cerebral swelling (loss of sulcus or sulcal effacement, compression of the basilar cisterns, flattening of the ventricular margins), cerebral ischemia and infarction due to mechanical compression represent a very poor prognosis of the patient11).
This study had several limitations. First, there were missed records of pre-existing medical conditions as well as patient comorbidities. A number of co-morbid factors were associated with survival after trauma, especially in blunt injuries. However, according to a previous study, further improvement of accuracy was not seen with models that included information about comorbidities. Because trauma victims were relatively young, most comorbidities took place in less than 1% of trauma victims13). However, in our database, the average age of patients was 57.3 years, we thought that is why geographical position of our trauma center. Our model was comprised of a large proportion of elderly patients, so comorbidities might have contributed more to the results. Second, the duration of the study was only 1 year, and comparison and integration of registered data were not conducted with other trauma centers. A period of 1 year of data collection may not be sufficient and small sample sizes can result in a lack of power. The accuracy of the predicted survival rate will be improved with cumulative patient data.
Nowadays, trauma care is a significant, expensive problem for our society. Although the TRISS methodology offers a standard approach for tasking and evaluating the outcomes of trauma care, no study has analyzed the predictability of outcomes in traumatic brain injury. Despite the previously reported limitations, the overall performance of TRISS seemed acceptable. Moreover, TRISS is relatively exact and acceptable compared with actual data, therefore, it can be considered as a simple and time-saving method. To improve the prediction in severe TBI patients, we propose that severe brain swelling with absent ventricle or brainstem cistern and dilated both pupils, but calculated 5 in ISS, should be changed to 6.
References
1. Barmparas G, Singer M, Ley E, Chung R, Malinoski D, Margulies D, et al. Decreased intracranial pressure monitor use at level II trauma centers is associated with increased mortality. Am Surg. 2012; 78:1166–1171. PMID: 23025964.

2. Cayten CG, Stahl WM, Murphy JG, Agarwal N, Byrne DW. Limitations of the TRISS method for interhospital comparisons : a multihospital study. J Trauma. 1991; 31:471–481. discussion 481-482. PMID: 2020032.
3. Champion HR, Copes WS, Sacco WJ, Frey CF, Holcroft JW, Hoyt DB, et al. Improved predictions from a severity characterization of trauma (ASCOT) over Trauma and Injury Severity Score (TRISS): results of an independent evaluation. J Trauma. 1996; 40:42–48. discussion 48-49. PMID: 8576997.
4. Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW Jr, et al. The Major Trauma Outcome Study : establishing national norms for trauma care. J Trauma. 1990; 30:1356–1365. PMID: 2231804.
5. Chiara O, Cimbanassi S, Pitidis A, Vesconi S. Preventable trauma deaths : from panel review to population based-studies. World J Emerg Surg. 2006; 1:12. PMID: 16759417.
6. Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The Injury Severity Score revisited. J Trauma. 1988; 28:69–77. PMID: 3123707.

7. Gabbe BJ, Cameron PA, Wolfe R. TRISS : does it get better than this? Acad Emerg Med. 2004; 11:181–186. PMID: 14759963.
8. Hannan EL, Mendeloff J, Farrell LS, Cayten CG, Murphy JG. Validation of TRISS and ASCOT using a non-MTOS trauma registry. J Trauma. 1995; 38:83–88. PMID: 7745667.

9. Kilgo PD, Meredith JW, Hensberry R, Osler TM. A note on the disjointed nature of the injury severity score. J Trauma. 2004; 57:479–485. discussion 486-487. PMID: 15454791.

10. Kilgo PD, Meredith JW, Osler TM. Incorporating recent advances to make the TRISS approach universally available. J Trauma. 2006; 60:1002–1008. discussion 1008-1009. PMID: 16688062.

11. Kim JJ, Gean AD. Imaging for the diagnosis and management of traumatic brain injury. Neurotherapeutics. 2011; 8:39–53. PMID: 21274684.

12. Kirkham JJ. A comparison of hospital performance with non-ignorable missing covariates : an application to trauma care data. Stat Med. 2008; 27:5725–5744. PMID: 18646254.

13. Millham FH, LaMorte WW. Factors associated with mortality in trauma : re-evaluation of the TRISS method using the National Trauma Data Bank. J Trauma. 2004; 56:1090–1096. PMID: 15179251.

14. Moore L, Lavoie A, Camden S, Le Sage N, Sampalis JS, Bergeron E, et al. Statistical validation of the Glasgow Coma Score. J Trauma. 2006; 60:1238–1243. discussion 1243-1244. PMID: 16766966.

15. Moore L, Lavoie A, LeSage N, Abdous B, Bergeron E, Liberman M, et al. Statistical validation of the Revised Trauma Score. J Trauma. 2006; 60:305–311. PMID: 16508487.

16. Moore L, Lavoie A, Turgeon AF, Abdous B, Le Sage N, Emond M, et al. Improving trauma mortality prediction modeling for blunt trauma. J Trauma. 2010; 68:698–705. PMID: 20220424.

17. Schluter PJ, Nathens A, Neal ML, Goble S, Cameron CM, Davey TM, et al. Trauma and Injury Severity Score (TRISS) coefficients 2009 revision. J Trauma. 2010; 68:761–770. PMID: 20386271.

18. Trunkey DD. Trauma. Accidental and intentional injuries account for more years of life lost in the U.S. than cancer and heart disease. Among the prescribed remedies are improved preventive efforts, speedier surgery and further research. Sci Am. 1983; 249:28–35. PMID: 6623052.
19. West TA, Rivara FP, Cummings P, Jurkovich GJ, Maier RV. Harborview assessment for risk of mortality : an improved measure of injury severity on the basis of ICD-9-CM. J Trauma. 2000; 49:530–540. discussion 540-541. PMID: 11003333.
Fig. 1
A large amount of acute subdural hemorrhage along the right cerebral hemisphere; brain CT shows the mass effect with right subfalcine herniation (arrow).
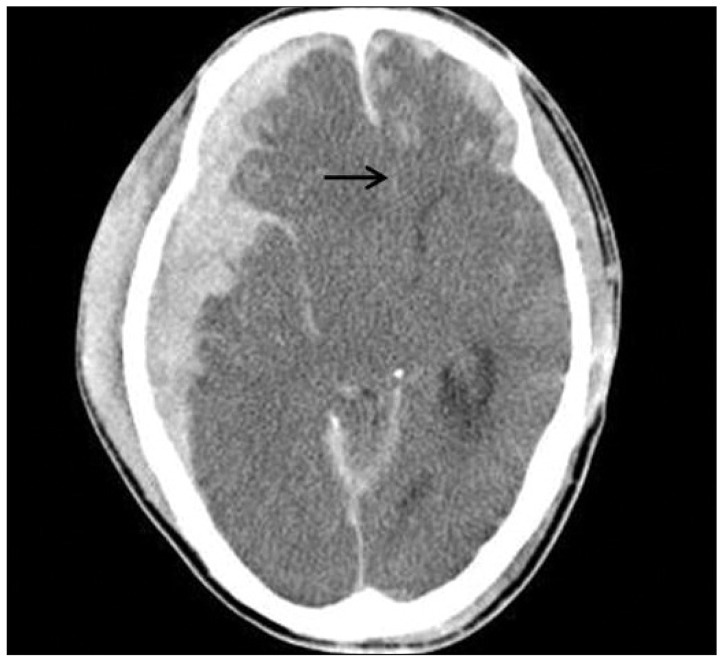
Fig. 2
Acute diffuse subdural hemorrhage along the right cerebral hemisphere, brain CT shows severe brain swelling with effacement of CSF spaces, decreased gray-white matter demarcations (arrowhead), and midline shifting to the left (arrow, about 13 mm midline shift to left).
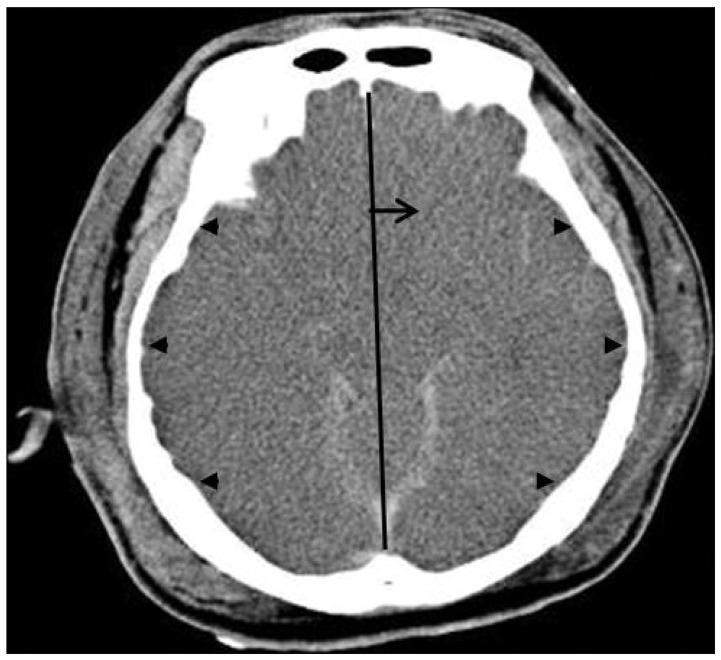
Table 1
Physiologic score system with high inter-rater reliability and demonstrated accuracy in predicting death




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download