Abstract
Lumbar microdiscectomy (MD) is the gold standard for treatment of lumbar disc herniation. Generally, the surgeon attempts to protect the facet joint in hopes of avoiding postoperative pain/instability and secondary degenerative arthropathy. We believe that preserving the facet joint is especially important in young patients, owing to their life expectancy and activity. However, preserving the facet joint is not easy during lumbar MD. We propose several technical tips (superolateral extension of conventional laminotomy, oblique drilling for laminotomy, and additional foraminotomy) for facet joint preservation during lumbar MD.
Lumbar microdiscectomy (MD) is the gold standard for treatment of lumbar disc herniation. MD is associated in general with good surgical outcomes, but there is considerable morbidity seen by long-term follow-up6,12,13,15,16). An experienced spine surgeon can shorten the operation time and minimize normal tissue injury and patient discomfort7,19).
If significant facet hypertrophy is present with foraminal stenosis or lateral recesses syndrome, surgeons often perform a partial facetectomy3,9). However, the surgeon generally attempts to protect facet joint in the hopes of avoiding postoperative pain/instability and secondary degenerative arthropathy8). We believe that preserving the facet joint is especially important in young patients, owing to their life expectancy and activity. However, facet joint preservation is not easy during lumbar MD. Celik et al.2) reported a facet joint preservation rate of 57.7% (97/168) in a lumbar MD case series. We propose several technical tips that offer facet joint preservation for lumbar MD.
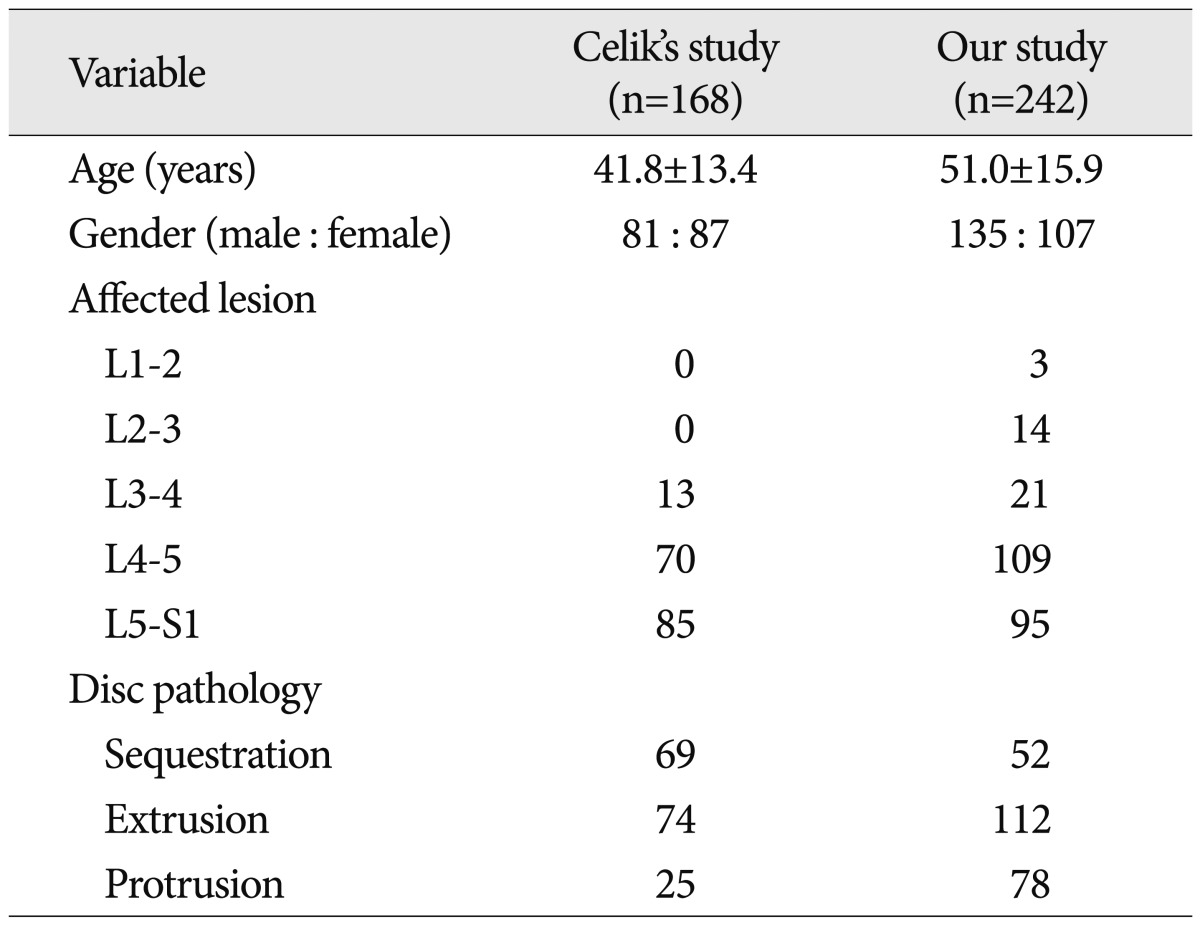
A total of 242 patients with lumbar disc herniation between L1 and S1 were enrolled in the study from January 2007 to April 2011. The basic characteristics of enrolled patients are summarized in Table 1.
Preoperative MRI and postoperative computerized tomography (CT) were done. Before surgery and at the time of follow-up, the degrees of leg and back pain were evaluate using the Visual Analog Scale (VAS, 0=no pain; 10=maximum pain imaginable). We routinely performed postoperative CT at 3 days after surgery. Facet violation was either confirmed intraoperatively by joint-fluid leakage or postoperatively by CT.
Conventional hemilaminotomy is performed by removing the inferior edge of the superior lamina overlying the disc space. Removal of the ligament flavum exposes the fat covering the thecal sac and the nerve root located inferolateral to the thecal sac. To expose the disc space or disc fragment, the shoulder portion of the nerve root should be secured. In numerous cases, disc fragments may be located beneath the traversing nerve root and the affected nerve root may be displaced laterally in relation to the normal position. Therefore, it is not easy to secure the shoulder portion of the nerve root in conventional hemilaminotomy. A superolateral extension of conventional laminotomy help in securing the shoulder portion of nerve root (Fig. 1). The added exposure allows for better visualization of the disc space or herniated disc material and usually results in safe discectomy.
The facet joint is angled to the coronal plane, and the mean joint angles of each lumbar level are 39-61°1). Therefore, conventional laminectomy can violate the medial portion of the facet joint (Fig. 2). We propose oblique drilling for laminotomy, which it should permit a proper surgical view without facet joint violation. Additionally, we completely remove the ligament flavum near the inferior surface of the facet joint. This procedure can help to decompress the affected root without joint injury.
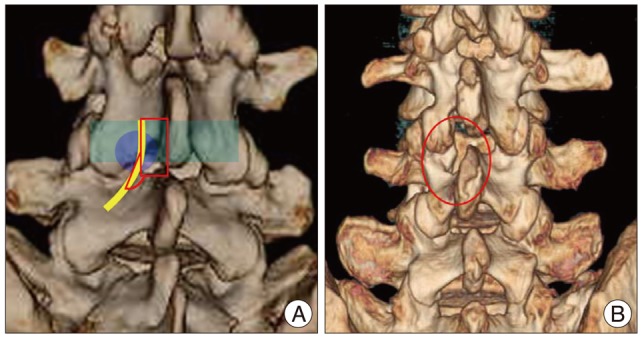
Facet-joint-preserving MD can require more retraction of the nerve root to expose the disc space during discectomy. Therefore, enough decompression of the affected nerve root is required to avoid nerve injury. Additional foraminotomy is helpful to achieve root decompression (Fig. 3). It can increase the movability of nerve root, and consequently, it should decrease the possibility of retraction injury during discectomy.
The demographic data of the cases, including mean±standard deviation and frequencies, are shown in Table 1. The ages of patients ranged from 15 to 72 years (51.0±15.9 years) and follow-ups ranged from 2 to 5 years (3.2±1.2). There were some complications after surgery, such as hematoma (1 case), deep infection (1 case), instability (2 cases), postoperative fibrosis (2 cases), and transient root injury (1 case). Recurrent lumbar disc herniation was observed in 7 cases (2.9%) at final follow-up.
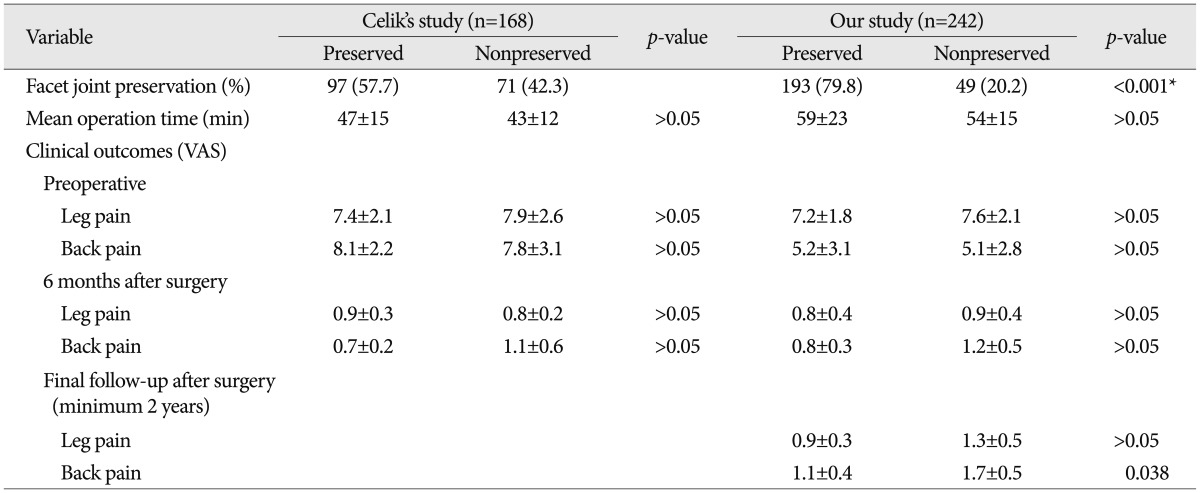
We categorized the preoperative VAS and the postoperative VAS according to facet joint preservation (Table 2). Generally, there were no significant differences between Celik's study and our study, and between the facet joint preservation group and nonpreservation group. However, we found significant difference in final follow-up data in our study. The final follow-up VAS of back pain was 1.1±0.4 in preservation group and 1.7±0.5 in nonpreservation group, respectively (p=0.038).
We used two methods for analyzing the facet joint preservation rate. One is based on the intraoperative findings and the other is based on postoperative CT. If we saw a joint fluid leakage or a tear in the joint capsule intraoperatively, we classified the case in the nonpreserved group. Also, we included cases in the nonpreserved group if postoperative CT showed the articular surface of the facet joint was injured. As a result, our case series showed a 79.8% facet joint preservation rate (193/242) for MD. In contrast, Celik et al. reported a preservation rate of 57.7% (97/168). This difference is statistically significant (p<0.001).
Lumbar MD is the standard treatment for lumbar disc herniation. Although MD is the most popular surgical technique, it is not easy to achieve excellent outcomes. Considerable complications can arise related to surgery6,12,13,15,16). Actually, postoperative back pain, instability, and degenerative arthropathy can result from facet joint violation, so the surgeon generally attempts to protect the facet joint8). Especially, we believe that facet joint preservation is important in young patients, owing to their life expectancy and activity.
We proposed three surgical tips for facet joint preservation during MD. First, superolateral extension of conventional laminotomy makes it easier to secure the shoulder portion of the nerve root (Fig. 1). The added exposure allows for better visualization of the disc space or herniated disc material and usually results in safe discectomy. However, excessive superolateral extension of the laminotomy can induce iatrogenic fracture of inferior articular process, so we have to check the lateral margin of the inferior articular process. Traditional laminectomy can violate the medial portion of the facet joint, because the facet joint is angled to the coronal plane and the mean joint angles of each lumbar level are 39-61° (Fig. 2)1). Therefore, the second surgical tip is oblique drilling for laminotomy, which should permit a proper surgical view without facet joint violation (Fig. 2). If the spinous process is hypertrophic, drilling of the spinous process is needed for a satisfactory surgical view. Of course, this procedure may not provide enough decompression the affected nerve root (traversing nerve root). Therefore, we completely remove the ligament flavum under the inferior surface of the facet joint. We could find an enough decompression to nerve root after discectomy or fragmentectomy, because the nerve root returns to former position after the elimination of mass effect. However, the facet-joint-preserving technique can sometimes require greater retraction of nerve root during discectomy or fragmentectomy compared to the partial facetectomy technique, so it require an enough nerve root decompression before nerve root retraction. The third surgical tip, therefore is additional foraminotomy. We always perform an additional foraminotomy for this reason (Fig. 3). This procedue could increase the mobility of nerve root, so it allows sufficient retraction of the nerve root without retraction injury and sufficient decompression to the nerve root. Also, the additional foraminotomy may decrease the symptomatic recurrence of lumbar disc herniation. Lebow et al. reported a recurrence rate for lumbar disc herniation based on radiologic findings of 23.1% (25/108 patients) in two year follow-up after MD. Interestingly, asymptomatic and symptomatic recurrence rates were 13.0% (14/108 patients) and 10.2% (11/108 patients), respectively. This study shows the importance of enough neural decompression. In our study, the mean final follow-up period was 3.2±1.2 years and the recurrence rate was 2.9%. Generally, the recurrence rates in previous studies were 5 to 15%4,5,11,14,17,18), so the 2.9% rate (7/242) in our study is relatively low. However, this result needs a controlled prospective study with a long-term follow-up for detailed analysis.
Compared with those of lower levels, lengths of the lamina are shorter and facet joint angle is greater in upper lumbar (L1-2, L2-3, L3-4)10). Therfore facet joint preservation is difficult on upper lumbar disc herniation. In our study, facet joint preservation rate of upper lumbar (L1-2, L2-3, L3-4, 23/38 patients, 60.5%) is less than it of lower lumbar (L4-5, L5-S1, 170/204 patients, 83.3%).
Finally, we would insist that these surgical tips are not best for all cases of MD. There are several disadvantage for these surgical tips during MD. First, the facet-joint-preserving MD technique can possibly result in nerve retraction injury if significant facet hypertrophy is present with foraminal stenosis or lateral recesses syndrome. In this situation, partial facetectomy would be needed to prevent nerve injury. Even in experienced hands, nerve root retraction is difficult during facet-joint-preserving MD. Actually, our operation time is longer than in Celik's study (Table 2), because we spend considerable time on nerve root retraction. Second, as mentioned above, excessive superolateral extension of the laminotomy can induce iatrogenic fracture of inferior articular process, so we have to check the lateral margin of the inferior articular process.
Therefore, these surgical tips cannot sufficiently guarantee the preservation of the facet joint in all cases, but it should help in general to preserve the facet joint during MD.
We propose that these surgical tips (superolateral extension of conventional laminotomy, oblique drilling for laminotomy, and additional foraminotomy) should be helpful towards preserving the facet joint during MD. Also, the techniques might result in a decreased incidence of symptomatic recurrent disc herniation and postoperative back pain.
References
1. Boden SD, Riew KD, Yamaguchi K, Branch TP, Schellinger D, Wiesel SW. Orientation of the lumbar facet joints : association with degenerative disc disease. J Bone Joint Surg Am. 1996; 78:403–411. PMID: 8613448.
2. Celik SE, Celik S, Kara A, Ince I, Goksu K. Lumbar facet joint angle and its importance on joint violation in lumbar microdiscectomy. Neurosurgery. 2008; 62:168–172. discussion 172-173. PMID: 18300904.

3. Ciric I, Mikhael MA, Tarkington JA, Vick NA. The lateral recess syndrome. A variant of spinal stenosis. J Neurosurg. 1980; 53:433–443. PMID: 7420163.
4. Connolly ES. Surgery for recurrent lumbar disc herniation. Clin Neurosurg. 1992; 39:211–216. PMID: 1458740.
5. Fandino J, Botana C, Viladrich A, Gomez-Bueno J. Reoperation after lumbar disc surgery : results in 130 cases. Acta Neurochir. 1993; 122:102–104. PMID: 8333299.
6. Findlay GF, Hall BI, Musa BS, Oliveira MD, Fear SC. A 10-year follow-up of the outcome of lumbar microdiscectomy. Spine. 1998; 23:1168–1171. PMID: 9615370.

7. Javedan S, Sonntag VK. Lumbar disc herniation : microsurgical approach. Neurosurgery. 2003; 52:160–162. discussion 162-164. PMID: 12493114.
8. Kambin P, Cohen LF, Brooks M, Schaffer JL. Development of degenerative spondylosis of the lumbar spine after partial discectomy. Comparison of laminotomy, discectomy, and posterolateral discectomy. Spine. 1995; 20:599–607. PMID: 7604330.

9. Kanamiya T, Kida H, Seki M, Aizawa T, Tabata S. Effect of lumbar disc herniation on clinical symptoms in lateral recess syndrome. Clin Orthop Relat Res. 2002; 131–135. PMID: 11964642.

10. Kim DS, Lee JK, Jang JW, Ko BS, Lee JH, Kim SH. Clinical features and treatments of upper lumbar disc herniations. J Korean Neurosurg Soc. 2010; 48:119–124. PMID: 20856659.

11. Kim KT, Park SW, Kim YB. Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine. 2009; 34:2674–2678. PMID: 19910771.

12. Kotilainen E. Long-term outcome of patients suffering from clinical instability after microsurgical treatment of lumbar disc herniation. Acta Neurochir. 1998; 140:120–125. PMID: 10398990.

13. Kotilainen E, Valtonen S. Clinical instability of the lumbar spine after microdiscectomy. Acta Neurochir. 1993; 125:120–126. PMID: 8122535.

14. Mobbs RJ, Newcombe RL, Chandran KN. Lumbar discectomy and the diabetic patient: incidence and outcome. J Clin Neurosci. 2001; 8:10–13. PMID: 11320971.

15. Postacchini F. Results of surgery compared with conservative management for lumbar disc herniations. Spine. 1996; 21:1383–1387. PMID: 8725934.

16. Rahme R, Moussa R, Bou-Nassif R, Maarrawi J, Rizk T, Nohra G, et al. Lumbar microdiscectomy : a clinicoradiological analysis of outcome. Can J Neurol Sci. 2011; 38:439–445. PMID: 21515503.
17. Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation: results of operative management. Spine. 2001; 26:672–676. PMID: 11246384.
18. Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosurg Focus. 2003; 15:E10. PMID: 15347228.

19. Wenger M, Mariani L, Kalbarczyk A, Groger U. Long-term outcome of 104 patients after lumbar sequestrectomy according to Williams. Neurosurgery. 2001; 49:329–334. discussion 334-335. PMID: 11504108.

Fig. 1
A : Superolateral extension of conventional laminotomy can help in securing the shoulder portion of the traversing nerve root. The added exposure allows for better visualization of the disc space or herniated disc material and usually results in safe discectomy (red fan-shape : superolateral extension of conventional laminotomy, red square : conventional laminotomy, yellow line : traversing nerve root). B : Superolateral extension of conventional laminotomy of postoperative finding (red circle : postoperative finding).
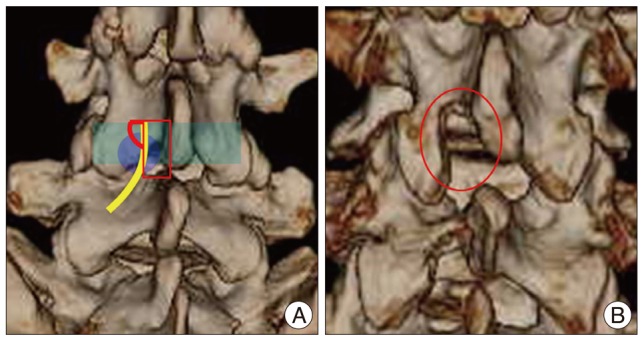
Fig. 2
Demonstrating how the facet joint angles were measured relative to the coronal plane, the faect joint angles of this lumbar level are 42°. Oblique drilling for laminotomy should permit proper surgical view without facet joint violation (red square : conventional laminectomy, yellow square : our laminotomy).
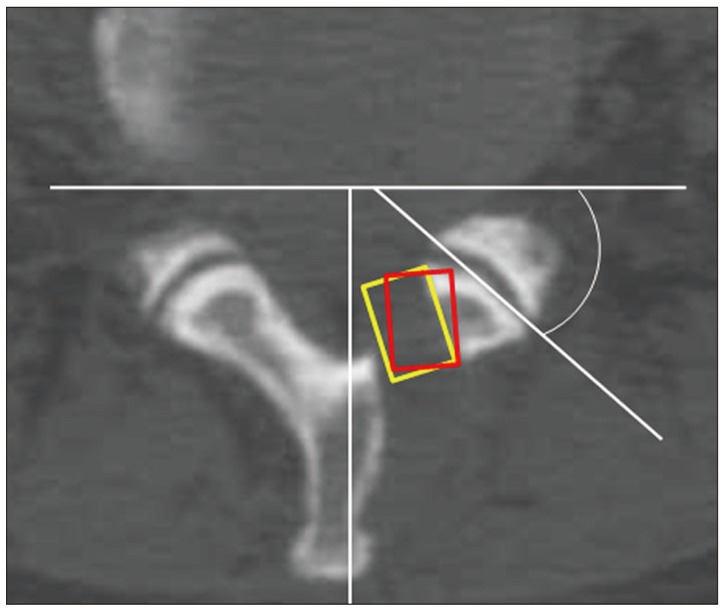
Fig. 3
A : Additional foraminotomy is helpful to achieve root decompression. It can increase the movability of the affected nerve root; consequently, it should decrease the possibility of retraction injury during discectomy (red fan-shape : additional foraminotomy, red square : laminotomy, yellow line : affected nerve root), B : Additional foraminotomy (red circle : postoperative finding).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download