Abstract
Objective
We present our experience of conventional posterior approach without fat lateral approach for ventral foramen magnum (FM) meningioma (FM meningioma) and tried to evaluate the approach is applicable to ventral FM meningioma.
Methods
From January 1999 to March 2011, 11 patients with a ventral FM meningioma underwent a conventional posterior approach without further extension of lateral bony window. The tumor was removed through a working space between the dura and arachnoid membrane at the cervicomedullary junction with minimal retraction of medulla, spinal cord or cerebellum. Care should be taken not to violate arachnoid membrane.
Results
Preoperatively, six patients were of Nurick grade 1, three were of grade 2, and two were of grade 3. Median follow-up period was 55 months (range, 20-163 months). The extent of resection was Simpson grade I in one case and Simpson grade II in remaining 10 cases. Clinical symptoms improved in eight patients and stable in three patients. There were no recurrences during the follow-up period. Postoperative morbidities included one pseudomeningocele and one transient dysphagia with dysarthria.
Foramen magnum (FM) meningiomas are challenging lesions because of the vicinity of the medulla oblongata, the lower cranial nerves, and the vertebral artery7). When diagnosed, these tumors are often large. However, due to their slow-growing rate and indolent course, partly attributable to the wide subarachnoid space at this level, clinical diagnosis is difficult, leading to a long interval since the onset of the first symptom5).
Dorsally situated FM meningiomas are clearly approached through a posterior approach, while ventrally located tumors have been considered to require other complex approaches to ensure surgical corridor such as the postero-lateral approach, called the far-lateral approach7), or the antero-lateral approach, also named the extreme-lateral approach6).
Since Goel et al.8) introduced the posterior approach for FM meningiomas, there have been only a few reports of the posterior approach in ventral FM meningiomas9,28,29). However, these were not conventional posterior surgery. In several studies, the bony exposure extended laterally8,10,28). The far lateral and extreme lateral approaches are difficult and unfamiliar to many surgeons. Lateral bony exposure also may pose risk to the vertebral artery and low cranial nerve injury. The occipital condyle drilling may sometimes be necessary in the far lateral approach. Therefore, conventional posterior approach without lateral bony extension may be good to address these problems.
In this report, we aimed to present our experience of conventional posterior approach without far lateral approach for ventral FM meningioma and tried to evaluate the approach is applicable to ventral FM meningioma.
From November 1999 to March 2011, we operated on 14 patients with FM meningioma in our clinic. We defined a ventral tumor as its dural origin was anterior to the dentate ligament that displaced the brain stem and spinal cord dorsally or dorsolaterally. And 11 of these patients had ventral FM meningioma. All of these 11 patients were operated on by a conventional posterior approach.
Magnetic resonance imaging (MRI) or computed tomography (CT) were taken pre- and postoperatively. The greatest axial tumor size was measured on axial cross-sections using gadolinium-enhanced T1-weighted MRI using Picture Archiving Communication System (Marosis, version 5438; Infinitt, Seoul, Korea).
Each patient's pre- and postoperative clinical status was evaluated with Nurick myelopathy grading system, which ranges from 0 to 5, with 0 denoting normal walking and 5 denoting complete paraplegia19).
The extent of tumor removal was evaluated by operative findings (Simpson grade) and that was confirmed by postoperative MRI. Gross total removal was defined as no visible enhancing/non-enhancing tumor on postoperative imaging, with the surgeon recording no remnant tumor on microscopic operative views. Recurrence was defined as a new onset or worsening of symptoms and/or radiological confirmation of tumor growth4). This retrospective study was approved by the institutional review board of Seoul National University Hospital (H-0910-014-296).
All operations were performed using a posterior approach consisting of suboccipital craniotomy without far lateral approach and C1 laminotomy. Further lateral extension of bony window was not performed in all cases (Fig. 1). After the dura was opened, care was taken not to violate the arachnoid membrane. We usually were able to find the tumor lateral to the medulla and cervical spinal cord. Thereafter, the dentate ligament was severed and C1 posterior root was cut, if needed. A working space was made between dura and arachnoid membrane at the cervicomedullary junction. As most tumors were a little eccentric, we could expose the tumor from one side (Fig. 2A). The tumor was removed little by little, using an ultrasonic aspirator. With this gradual removal of the tumor, we could make a working space large by large. The tumor was progressively delivered into the space made by decompression, with little displacing or handling the medulla, spinal cord or lower cranial nerves (Fig. 2B). The tumor was removed from one side in all cases. The key point is that ventral arachnoid membrane is not violated. Eventually, the tumor capsule could be pulled into the working space and excised. The dural origin of FM meningiomas was either excised or coagulated (Fig. 3).
The number of male and female patients was 5 and 6, respectively. Mean age was 59.1±12.4 years (range, 41-78 years). Paresthesia was the most common symptom and all patients were able to ambulate at the time of surgery. Median follow-up period was 55 months (range, 20-163 months). Preoperatively, six patients were of Nurick grade 1, three were of grade 2, and two were of grade 3. Pathological subtypes were 8 meningothelial, 2 transitional, and 1 angiomatous. Mean duration of symptom was 14.5±17.2 months (range 2-60 months). The mean size of maximal tumor diameter was 24.5±6.3 mm (range, 15-36.4 mm). Details are given in Table 1.
In the 11 ventral FM meningiomas, tumors were located intradurally in all patients. Preoperative T2 MRI did not show the absence of clear separating plane in all patients.
Tumors were gross totally removed in all patients (Fig. 4, Table 1). Mean operative time was 300±84 minutes (range, 210-420 minutes). The extent of resection was Simpson grade I in one case and Simpson grade II in remaining 10 cases (Table 1). There were no recurrences during the follow-up period. Pathological subtypes were 8 meningothelial, 2 transitional and 1 angiomatous. There were no cases of pial invasion in this series. Vertebral artery was saved in all cases except one. In this case, one vertebral artery was encased with the tumor. This encased vertebral artery was trapped through preoperative endovascular intervention in order to decrease the tumor vascularity, because the tumor was hypervascular.
Two patients with Nurick grade 3 improved to grade 2. Three patients with Nurick grade 2 improved to grade 1. In six patients with Nurick grade 1, three patients were in the same grade 1 and the other three patients improved to grade 0 (Table 1).
Two complications occurred. In Patient 2, postoperative pseudomeningocele was found. However, additional treatment was unnecessary. He had no further neurological deficits. In Patient 6, there was transient dysphagia with dysarthria. Postoperative dysphagia with dysarthria resolved progressively for 3 weeks following surgery (Table 1).
In this series, posterior surgery was a safe and effective method for FM meningiomas as neither operative morbidity nor permanent neurological deficit occurred in all patients. Gross total removal was achieved in all patients with minimal morbidity and in terms of Simpson grade, we could achieve grade 2 in all but one patient who got Simpson grade 1. Nurick grade improved in 8 patients and stable in 3 patients.
The posterior approach has several advantages. First, posterior approach is more familiar to surgeons, as well as being easier than the far lateral or extreme lateral approach. Second, there is no need for drilling the condyles or lateral mass. Although the working space is narrow at first, the posterior approach can provide enough working space after a tumor has started to be decompressed. Even though occipitocervical fusion is rarely necessary, occipital condyle resection was needed in between 0% and 66% in the far-lateral approach14,18,20,21,23,26). Third, postoperative recovery is fast. Fourth, in our experience, postoperative morbidity may be minimal with the conventional posterior approach. In our series, there was only one occurrence of transient neurological deficit (9%) and one incidence of pseudomeningocele. Various neurological complications have been reported in the studies using the far lateral or extreme lateral approaches as transient and permanent neurological morbidity occurred in 6-61% and 2-25%, respectively2,10,11,15,22,29). Although direct comparison of figures from each approach is inappropriate, we could assume that the complication after conventional posterior approach is not inferior to the far lateral approach. In addition, CSF fistula has been mentioned in the various series1-3,10,15,29).
Meningiomas are basically intradural and extra-arachnoid24). Both cranial and spinal meningiomas originate from dural attachments and stretch the arachnoid membrane, which can then be exploited as an anatomical dissection plane24).
Even though FM meningiomas were located closely with low cranial nerves and vertebral artery, the tumor mostly did not adhere to adjacent neurovascular structures because of arachnoid membrane. After internal debulking of the mass, tumor could be delivered into the working space made by decompression. Vertebral artery was located in the superior side of ventral FM meningiomas, except in one case. This tendency was similar to that presented in previous literature8,10,28). If the vertebral artery is encased by the tumor, preoperative endovascular intervention is recommended. Preoperative embolization or trapping if possible can be helpful when preoperative angiography revealed hypervascular tumor such as in Patient 7.
The mean size of tumor in our series was 24.5 mm. This is relatively smaller than in previous studies27,29). It has been reported that small FM meningiomas are more difficult to approach than large ones7,9). Based on our study results, relatively small ventral FM meningiomas can be removed by using a posterior approach. However, further studies may be necessary to indicate an applicable cut-off minimum size for posterior approach.
Most tumors were removed with Simpson grade II in our series even though the working space to remove the original dura can be large (Fig. 1B). Our previous studies with those of other investigators have demonstrated that for spinal meningiomas, gross total removal of a tumor and coagulation of its dural origin (Simpson grade II) appears to be sufficient2,30). On the other hand, Nakamura et al.17) recently reported that 6 out of 13 Simpson grade II resected spinal meningiomas underwent reoperation. The average follow-up period for reoperation was 12.2 years. In our study, average follow-up period was 78.3 months. There has been no reoperation for recurrence during this period. However, further follow-up may be necessary for recurrence in our series.
FM was derived embryologically from the fourth occipital "proatlas". The anterior landmarks for FM have been the lower third of the clivus and upper edge of the body of C26). The anterior tubercle of the clivus is derived from the hypocentrum of the proatlas, while the apex of the odontoid process of the axis is derived from the centrum of the proatlas16). We can infer that FM is an extension of the spinal canal. Hence, FM meningiomas are more similar to spinal cord meningiomas than to skull base meningiomas. Through our experience, ventral intradural extramedullary spinal cord tumors including meningiomas could be removed gross totally through conventional posterior approach12). Therefore, it is quite natural to use a conventional posterior approach for removing FM meningiomas like ventral intradural extramedullary spinal cord tumors.
The posterior approach for ventral FM meningioma should be used with caution. Since craniotomy is not extended laterally, exposure is limited at first. Therefore, the dural origin site can be manipulated only after the tumor was removed. If tumor vascularity is very high, a far lateral approach may be more suitable in terms of controlling the dural origin site first.
Additionally, the tendency of psammomatous meningioma toward pial invasion is well known13,24). When this type of tumor adheres to the spinal cord or brain stem, it is impossible to remove it completely using posterior approach. This type of tumor might be anticipated because preoperative MRI and/or CT show a very intimate connection to the spinal cord and the absence of the typical clear separating plane24). Preoperative T2 MRI did not show the absence of clear separating plane even in patient 1 and 9 whose preoperative Nurick grade were 3.
Also13), en plaque or recurrent meningiomas can be difficult to remove. Although we have not experienced these cases, we agree that the posterior approach would be risky in these cases because the normal dissection plane along the arachnoid membrane is absent2,13,25). Other approaches such as far lateral approach or anterior approach should be considered, even though gross total removal is probably impossible even with these approaches.
In the present study, we have described the feasibility of a posterior approach for ventral FM meningiomas. The present study has several limitations. First, this is a retrospective study without any control group. Although all these operations were consecutive series, such a study may lead to inevitable selection bias. Second, the number of patients was small. Case number may be not enough for posterior approach to be generalized. Nonetheless, this study confirmed the feasibility of the conventional posterior approach for ventral FM meningiomas.
Ventral FM meningiomas can be removed gross totally using a conventional posterior surgery without far lateral approach. The arachnoid membrane can then be exploited as an anatomical barrier. However, this approach should be applied with a thorough understanding of its anatomical limitation.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (No. 2010-0028631).
References
1. Arnautović KI, Al-Mefty O, Husain M. Ventral foramen magnum meninigiomas. J Neurosurg. 2000; 92(1 Suppl):71–80. PMID: 10616061.
2. Bassiouni H, Ntoukas V, Asgari S, Sandalcioglu EI, Stolke D, Seifert V. Foramen magnum meningiomas : clinical outcome after microsurgical resection via a posterolateral suboccipital retrocondylar approach. Neurosurgery. 2006; 59:1177–1185. discussion 1185-1187. PMID: 17277680.
3. Borba LA, de Oliveira JG, Giudicissi-Filho M, Colli BO. Surgical management of foramen magnum meningiomas. Neurosurg Rev. 2009; 32:49–58. discussion 59-60. PMID: 18815821.

4. Boström A, Bürgel U, Reinacher P, Krings T, Rohde V, Gilsbach JM, et al. A less invasive surgical concept for the resection of spinal meningiomas. Acta Neurochir (Wien). 2008; 150:551–556. discussion 556. PMID: 18421413.

5. Boulton MR, Cusimano MD. Foramen magnum meningiomas : concepts, classifications, and nuances. Neurosurg Focus. 2003; 14:e10. PMID: 15669785.
6. Bruneau M, George B. Classification system of foramen magnum meningiomas. J Craniovertebr Junction Spine. 2010; 1:10–17. PMID: 20890409.

7. Bruneau M, George B. Foramen magnum meningiomas : detailed surgical approaches and technical aspects at Lariboisière Hospital and review of the literature. Neurosurg Rev. 2008; 31:19–32. discussion 32-33. PMID: 17882459.

8. Goel A, Desai K, Muzumdar D. Surgery on anterior foramen magnum meningiomas using a conventional posterior suboccipital approach : a report on an experience with 17 cases. Neurosurgery. 2001; 49:102–106. discussion 106-107. PMID: 11440430.

9. Gupta SK, Khosla VK, Chhabra R, Mukherjee KK. Posterior midline approach for large anterior/anterolateral foramen magnum tumours. Br J Neurosurg. 2004; 18:164–167. PMID: 15176558.

10. Kandenwein JA, Richter HP, Antoniadis G. Foramen magnum meningiomas--experience with the posterior suboccipital approach. Br J Neurosurg. 2009; 23:33–39. PMID: 19234907.

11. Kano T, Kawase T, Horiguchi T, Yoshida K. Meningiomas of the ventral foramen magnum and lower clivus : factors influencing surgical morbidity, the extent of tumour resection, and tumour recurrence. Acta Neurochir (Wien). 2010; 152:79–86. discussion 86. PMID: 19779669.

12. Kim CH, Chung CK. Surgical outcome of a posterior approach for large ventral intradural extramedullary spinal cord tumors. Spine (Phila Pa 1976). 2011; 36:E531–E537. PMID: 21178841.

13. Klekamp J, Samii M. Surgical results for spinal meningiomas. Surg Neurol. 1999; 52:552–562. PMID: 10660020.

14. Kratimenos GP, Crockard HA. The far lateral approach for ventrally placed foramen magnum and upper cervical spine tumours. Br J Neurosurg. 1993; 7:129–140. PMID: 8494614.

15. Margalit NS, Lesser JB, Singer M, Sen C. Lateral approach to anterolateral tumors at the foramen magnum : factors determining surgical procedure. Neurosurgery. 2005; 56(2 Suppl):324–336. discussion 324-336. PMID: 15794829.
16. Muhleman M, Charran O, Matusz P, Shoja MM, Tubbs RS, Loukas M. The proatlas : a comprehensive review with clinical implications. Childs Nerv Syst. 2012; 28:349–356. PMID: 22282080.

17. Nakamura M, Tsuji O, Fujiyoshi K, Hosogane N, Watanabe K, Tsuji T, et al. Long-term surgical outcomes of spinal meningiomas. Spine (Phila Pa 1976). 2012; 37:E617–E623. PMID: 22146282.

18. Nanda A, Vincent DA, Vannemreddy PS, Baskaya MK, Chanda A. Far-lateral approach to intradural lesions of the foramen magnum without resection of the occipital condyle. J Neurosurg. 2002; 96:302–309. PMID: 11841072.

19. Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972; 95:87–100. PMID: 5023093.

20. Pamir MN, Kiliç T, Ozduman K, Türe U. Experience of a single institution treating foramen magnum meningiomas. J Clin Neurosci. 2004; 11:863–867. PMID: 15519864.

21. Pirotte B, David P, Noterman J, Brotchi J. Lower clivus and foramen magnum anterolateral meningiomas : surgical strategy. Neurol Res. 1998; 20:577–584. PMID: 9785584.

22. Pirotte BJ, Brotchi J, DeWitte O. Management of anterolateral foramen magnum meningiomas : surgical vs conservative decision making. Neurosurgery. 2010; 67(3 Suppl Operative):ons58–ons70. discussion ons70. PMID: 20679947.
23. Samii M, Klekamp J, Carvalho G. Surgical results for meningiomas of the craniocervical junction. Neurosurgery. 1996; 39:1086–1094. discussion 1094-1095. PMID: 8938761.

24. Schaller B. Spinal meningioma : relationship between histological subtypes and surgical outcome? J Neurooncol. 2005; 75:157–161. PMID: 16132511.

25. Setzer M, Vatter H, Marquardt G, Seifert V, Vrionis FD. Management of spinal meningiomas : surgical results and a review of the literature. Neurosurg Focus. 2007; 23:E14. PMID: 17961038.
26. Shin H, Barrenechea IJ, Lesser J, Sen C, Perin NI. Occipitocervical fusion after resection of craniovertebral junction tumors. J Neurosurg Spine. 2006; 4:137–144. PMID: 16506481.

27. Talacchi A, Biroli A, Soda C, Masotto B, Bricolo A. Surgical management of ventral and ventrolateral foramen magnum meningiomas : report on a 64-case series and review of the literature. Neurosurg Rev. 2012; 35:359–367. discussion 367-368. PMID: 22430127.

28. Wang ZY, Xie JC, Ma CC, Liu B, Chen XD, Li ZD, et al. Microsurgery on foramen magnum meningioma with suboccipital. Beijing Da Xue Xue Bao. 2004; 36:634–636. PMID: 15605099.
29. Wu Z, Hao S, Zhang J, Zhang L, Jia G, Tang J, et al. Foramen magnum meningiomas : experiences in 114 patients at a single institute over 15 years. Surg Neurol. 2009; 72:376–382. discussion 382. PMID: 19608233.

30. Yoon SH, Chung CK, Jahng TA. Surgical outcome of spinal canal meningiomas. J Korean Neurosurg Soc. 2007; 42:300–304. PMID: 19096560.

Fig. 1
Illustrative case of postoperative CT (case 5). A : Preoperative T1 weighted sagittal MR image with gadolinium enhancement. B : Preoperative T1 weighted axial MR image with enhancement. C : Postoperative CT image in foramen magnum shows the extent of suboccipital craniotomy. Arrows indicate the extent of craniotomy. D : Postoperative CT image in C1 posterior arch area. Arrows indicate the extent of C1 laminotomy. E : Three dimension reconstructed postoperative CT image. Arrows indicate the extent of craniotomy and C1 laminotomy.
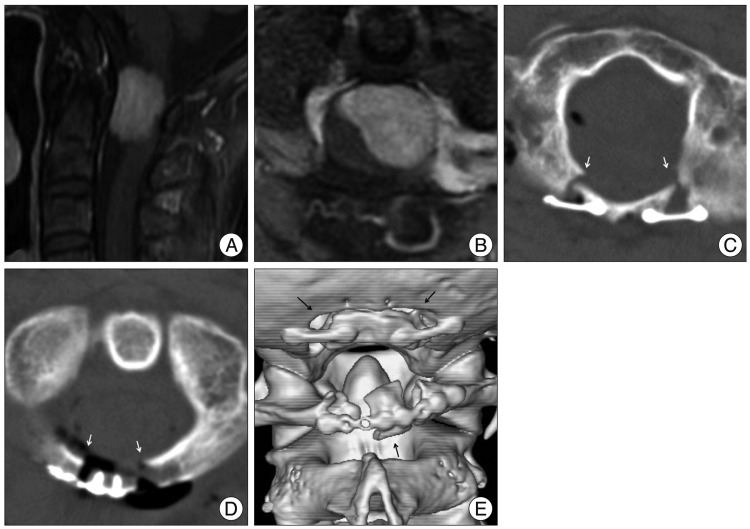
Fig. 2
Illustrative case 1 (case 9). A : An operative photo shows a working space between dura and arachnoid membrane at cervicomedullary junction where internal decompression is initiated. Arrow is the working space. B : An operative photo shows no mass after gross total removal. D : dura, SC : spinal cord, CB : cerebellum, T : tumor.
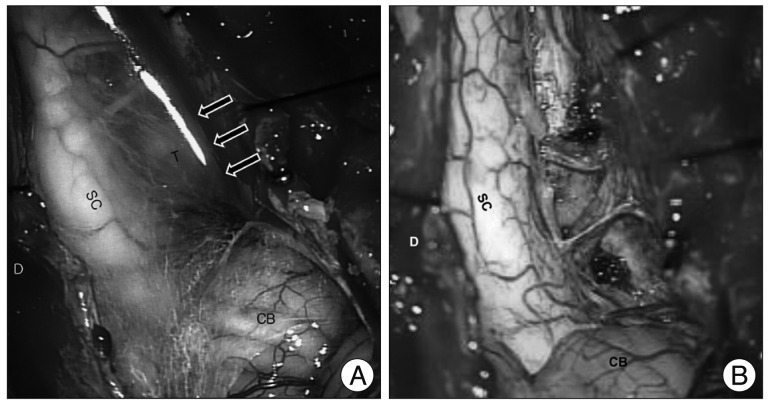
Fig. 3
Schematic drawing shows a working space which is between dura and arachnoid membrane at cervicomedullary junction. Dark area is the working space. A : arachnoid membrane, C1 : C1 posterior root, D : dura, DL : dentate ligament, T : tumor, SC : spinal cord.
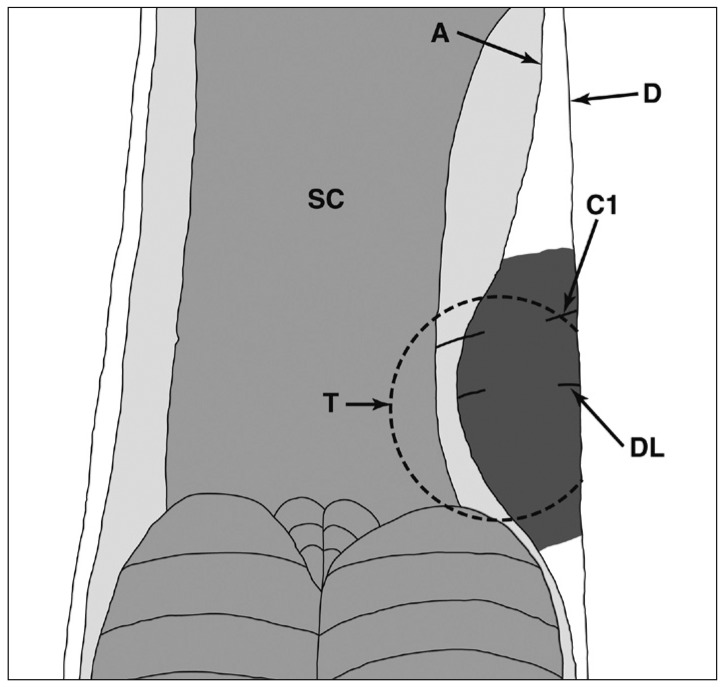
Fig. 4
Illustrative case of gross total removal (case 7). A : Preoperative T1 weighted sagittal MR image with gadolinium enhancement. B : Preoperative T1 weighted axial MR image with enhancement. C : Postoperative T1 weighted sagittal MR image with enhancement showing no residual mass. D : Postoperative T1 weighted axial MR image with enhancement showing no residual mass.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download