Abstract
Objective
There are differences in the clinical characteristics and surgical results between upper (L1-2 and L2-3) and lower (L3-4, L4-5, and L5-S1) lumbar disc herniations. We conducted this study to compare the clinical features and surgical outcomes between the two types of lumbar disc herniations.
Methods
We retrospectively reviewed the clinical features of patients who underwent microdiscectomies from 2008 to 2012. We evaluated the clinical characteristics such as age, preoperative autonomic dysfunction, the presence or absence of previous lumbar surgery and fusion required during surgery. Visual Analogue Scale (VAS) scores about back pain and leg pain were evaluated preoperatively and at the final follow-up.
Results
Upper lumbar group (n=15) was significantly older than lower lumbar group (n=148). The incidence of autonomic dysfunction was significantly higher in upper lumbar group. The number of patients with a previous lumbar surgery was significantly greater in upper lumbar group. There was no statistical significance for fusion required during surgery between two groups. Both groups showed a significant decrease in the VAS scores of leg pain. VAS scores of back pain were significantly decreased in lower lumbar group. But this was not seen in upper lumbar group. Both groups showed significant improvement of Oswestry Disability Index score.
Conclusion
Upper lumbar group had different clinical characteristics from those of lower lumbar group and these include older age, a higher incidence of autonomic dysfunctions and a higher incidence of patients with previous lumbar surgery. There were no significant differences in surgical outcomes, except for back pain, between two groups.
There is no clear definition of "the upper" lumbar disc herniations. It includes T12-L1, L1-2, and L2-3 or L1-2 and L2-3. Most of the reports define it as the lumbar disc herniations affecting the spinal level of L1-2, L2-3, and L3-4, accounting for approximately frequency of 5% of total cases of lumbar disc herniations1,3,8,9,12). The herniations of L3-4 accounted for 70-83% of all upper lumbar disc herniations in above mentioned reports1,9,12). According for Sanderson et al.11), however, there are no significant differences in the anatomical characteristics and surgical outcomes between the L3-4 disc herniation and the lower one. It has therefore been suggested that the L3-4 level should be excluded from the upper lumbar disc.
Given the above background, we retrospectively reviewed the clinical features of our patients and compared the clinical features and surgical outcomes between the upper (L1-2 and L2-3) and the lower (L3-4, L4-5, and L5-S1) lumbar disc herniations.
We retrospectively reviewed the medical records and radiological data of all patients who underwent microdiscectomies for the treatment of lumbar disc herniations at our medical institution from May 2008 to December 2012. Exclusion criteria for the current study were the lumbar disc herniations with abnormal bony involvement, ossification of the ligamentum flavum, and severe spondylosis. Among surgical methods, cases of paramedian approach for far-lateral disc were excluded. In the current study, we evaluated the clinical characteristics such as age, preoperative autonomic dysfunction (bladder and bowl), the presence or absence of previous lumbar surgery and fusion required during surgery. Preoperative magnetic resonance (MR) imaging or computed tomography, plain radiographs (including dynamic flexion/extension view) was performed. During the follow-up periods, dynamic flexion/extension images were evaluated. All the patients underwent a posterior conventional microdiscectomy, which included partial hemilaminectomy, medial facetectomy, and discectomy. When spinal instability was expected intraoperatively, fusion was performed. The Visual Analogue Scale (VAS) score about back pain and leg pain were evaluated preoperatively and last follow-up. In addition, the Oswestry Disability Index (ODI) was evaluated. Statistical analysis of the data was performed by SPSS statistical software (version 18.0, Chicago, IL, USA). Because the small size of this study, Mann-Whitney U-test and repeated measures analysis of variance were used for the statistical analysis. The statistical significance was set at p<0.05.
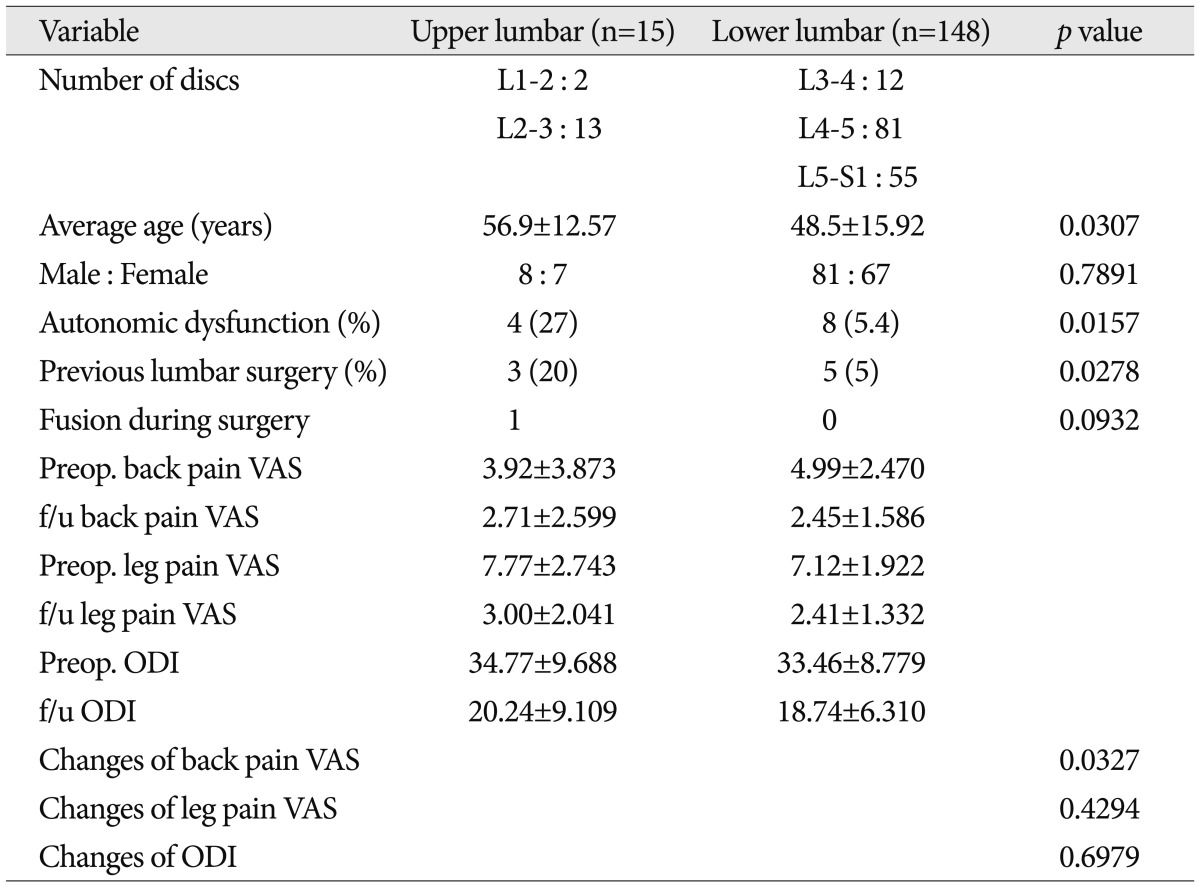
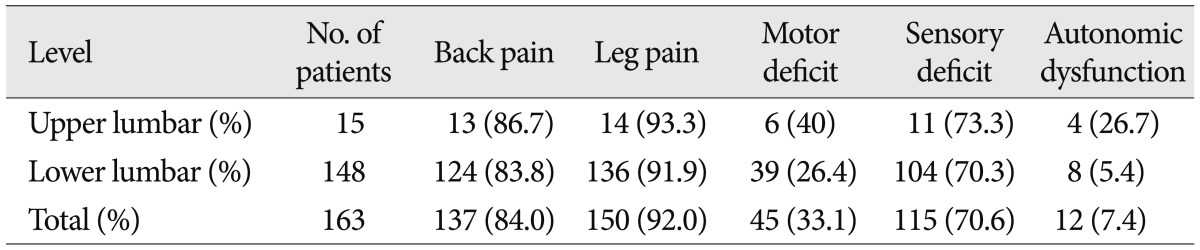
As shown in Table 1, our clinical series of patients were divided into two groups : the upper lumbar group (n=15) and the lower lumbar group (n=148). The mean follow-up period was 27.3 months and 29.8 months in the corresponding order. The mean age was 56.9±12.57 years and 48.5±15.92 years in the corresponding order. This indicates that there was a significant difference in the mean age between the two groups (p=0.0307). In the upper lumbar group, There were eight men (54%) and seven women (46%). In the lower lumbar group, there were 81 men (55%) and 67 women (45%). This indicates that there was no significant difference in the male-to-female ratio between the two groups (p=0.7891).
Clinical features are revealed in Table 2. It shows no significant differences in back and leg pain, motor and sensory deficits between two groups, except autonomic dysfunction. Distribution of pain or sensory change of upper lumbar group is presented in Fig. 1. The patients of the upper lumbar group complained of pain or sensory deficit on buttock (n=13), posterolateral thigh (n=7), anterior thigh (n=5), anterolateral lower leg (n=4), anterolateral thigh (n=3), calf (n=3), inguinal (n=1), perianal (n=1), and foot dorsum (n=1).
The incidence of autonomic dysfunction was significantly higher in the upper lumbar group (four patients, 27%) as compared with the lower lumbar group (eight patients, 5.4%) (p=0.0157).
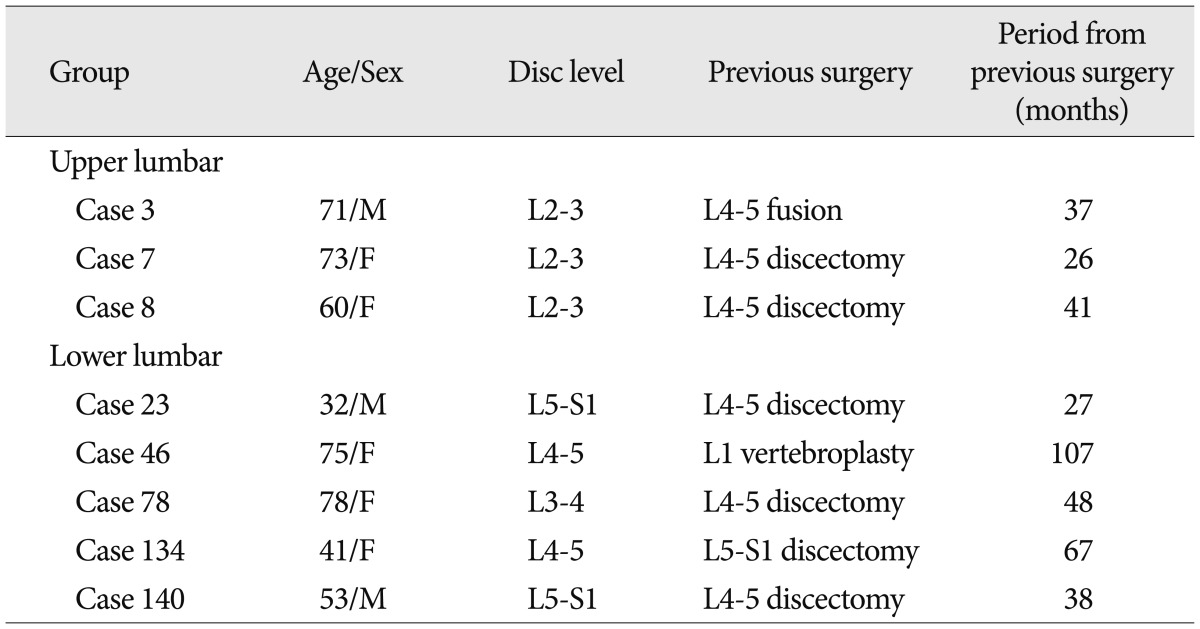
Characteristics of patients with past history of lumbar surgery are presented in Table 3. Three patients of upper lumbar group had previous lumbar surgery in L4-5. The periods from previous surgery to present surgery were variable. Five patients of lower lumbar group had previous lumbar surgery in various levels. The periods from previous surgery to present surgery were variable too. The number of patients with a past history of taking lumbar surgery was significantly greater in the upper lumbar group as compared with the lower lumbar group (20% vs. 5%) (p=0.0278). In both groups, only one patient underwent the fusion surgery due to instability during surgery. This was in the upper lumbar group. But this was not of clinical significance (p=0.0932).
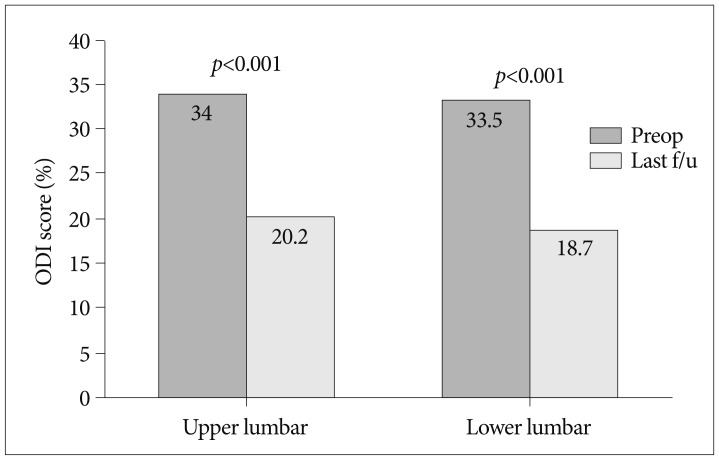
The VAS scores for back pain and leg pain, and ODI scores which were checked before surgery and 24 months after surgery were analyzed. There were significant differences in the postoperative outcomes between the two groups (Fig. 2). In all the parameters, the VAS scores ranged between 0 and 10 points. In the upper lumbar group, the mean VAS scores of back pain and leg pain were 3.92 and 7.77 points preoperatively and 2.71 and 3.00 at the 24 months postoperatively. In the lower lumbar group, these values were 4.99 and 7.12 points preoperatively and 2.45 and 2.41 points at the 24 months postoperatively. Both groups showed a significant decrease in the VAS scores of leg pain (p<0.001). The VAS scores of back pain were significantly decreased in the lower lumbar group (p<0.001). But this was not seen in the upper lumbar group (p=0.1796) (Fig. 2A). In ODI score (Fig. 3), both groups showed a statistically significant decrease (p<0.001). There was statistically significant difference in the degree of the reduction of the back pain VAS score between the two groups (p=0.0327) (Table 1). There were no statistically significant difference in the degree of the reduction of the leg pain VAS score and ODI score between the two groups (p=0.4294 and p=0.6979, respectively).
The upper lumbar vertebrae have a different anatomical aspect such as a narrower spinal canal and smaller range of motion as compared with the lower lumbar vertebrae. Its narrow spinal canal facilitates the compression of the conus medullaris or cauda equina, resulting in polyneuropathy which is not localized by exact nerve root. Moreover, the upper lumbar vertebrae have a smaller range of motion than the lower one. Fontanesi et al.4) suggested that this renders the upper lumbar vertebrae less vulnerable to lesser spondylosis, disc degeneration, and disc herniations. It has been reported that there are age-related changes in the mobility of facet joint in the lower lumbar vertebrae and this transfers the mechanical stress to the upper one6). According to Hsu et al.5), radiologic data indicate that the disc herniations or degenerations of the upper lumbar vertebrae without abnormalities of the lower lumbar level are associated with concurrent spinal abnormalities on MR image scans. We therefore presume that if there are any factors, including the stress, affecting the dynamics of the upper lumbar vertebrae, this would lead to the herniations of the upper lumbar vertebrae.
Our results showed that the mean age was significantly higher in the upper lumbar group compared with the lower lumbar group. It has been reported that the age is one of the factors involved in the pathogenesis of the upper lumbar disc herniation6,11). By contrast, Saberi and Isfahani10) reported that there was no statistically significant difference in the age between the upper and lower lumbar groups. Of note, however, these authors defined the upper lumbar as the spinal level of L1-2, L2-3, and L3-4. Moreover, the spinal level of L3-4 accounted for more than half of total patients of the upper lumbar group. We have therefore speculated that the age is one of the risk factors that are involved in the pathogenesis of the disc herniation at the spinal level of L1-2 and L2-3.
To date, many studies have reported that the upper lumbar disc herniations have more variable clinical symptoms due to ill-defined polyneuropathies1,2,7,9,11). Also, the present study showed the same result. Our results showed that the incidence of autonomic dysfunction was significantly higher in the upper lumbar group as compared with the lower one. Many studies have reported that there is a significant correlation between the autonomic dysfunction and the upper lumbar disc herniation1,2,6). It is well established that such correlation may arise from the anatomical proximity between the conus medullaris and the upper lumbar discs.
The number of patients with a past history of taking lumbar surgery was significantly greater in the upper lumbar group as compared with the lower one. In association with this, Sanderson et al.11) reported the same results. Some authors have reported, however, that there is no significant difference in the number of patients with a past history of taking lumbar surgery between the upper and lower lumbar group6,10). According to these authors, the upper lumbar vertebrae also included the L3-4 level that accounted for more than half of patients of the upper lumbar group. It can therefore, be inferred that A past history of lumbar surgery, affecting the dynamics of the spine, would be related to the pathogenesis of the L1-2, L2-3 disc herniation.
In most of the studies about the upper lumbar disc herniations, the surgical outcomes have been evaluated for the spinal level of L1-2, L2-3, and L3-4. They are compared with those for that of L4-5 and L5-S1. Albert et al.1) reported that 80% of patients with upper lumbar disc herniation had excellent or good outcomes during a mean follow-up period of 2.6 years. Pásztor and Szarvas9) also reported that 93% of total patients with upper lumbar disc herniation achieved excellent or good early outcomes, and 82% did excellent or good late ones. Sanderson et al.11) proposed that there is a similarity in the clinical characteristics between the L3-4 disc herniation and the lower lumbar disc herniation. In addition, as mentioned above, good results have been achieved because the good results at the spinal level of L3-4 may obscure less satisfactory outcomes at the spinal level of L1-2 and L2-3. Theses authors compared the surgical results at the spinal level of L1-2 and L2-3 with those at the spinal level of L3-4, thus reporting that the degree of the symptoms of the leg and back pain was improved in 58% and 53% of patients of lumbar disc herniation at the spinal level of L1-2 and L2-3, respectively. In the L3-4 herniation group, however these values were 94% and 87% in the corresponding order. On the other hand, Kim et al.7) reported that 81% of patients with the upper disc herniation at the spinal level of L1-2 and L2-3 achieved excellent or good outcomes. Iwasaki et al.6) reported a significant improvement in surgical results irrespective of the operative level in a series of 409 patients with lumbar disc herniations. Unlike these reports, we evaluated the surgical outcomes based on the degree of the reduction in the VAS scores of the back and leg pain as well as of the ODI. This showed that the degree of the reduction in the VAS cores of leg pain showed no significant difference between the two groups. Moreover, the VAS scores of back pain were significantly improved in the lower lumbar group. But this was not seen in the upper lumbar group. It means that the back pain of the upper lumbar group was lesser improved than that of the upper lumbar group. There was no significant difference in the ODI scores between the two groups. Based on these results, it can be inferred that we achieved good surgical results regardless of the lumbar disc level. But we could not clarify the reasons the back pain of the upper lumbar group was lesser improved as compared with the lower lumbar group. Presumably, the upper lumbar group may have a propensity of larger laminectomy and larger medial facetectomy due to smaller laminar width than the lower lumbar group. This may cause facet joint injury that read to the change of the spinal biomechanics despite a lack of radiological instability in the dynamic flexion/extension. Besides, the upper lumbar group had a more incidence of previous lumbar surgery. It may explain a lesser improved postoperative back pain of the upper lumbar group than that of the lower one. In general, the patients with lumbar surgery have a propensity of back pain after surgery. However, the preoperative VAS score of back pain of the upper lumbar group was larger than that of the lower one although the upper one had a more incidence of the previous lumbar surgery. It might be due to small series of patients in this study.
The series of the upper lumbar group was smaller than that of the lower one. So, the statistic comparison between the upper and lower lumbar groups was not clear. If the series of patients with the upper lumbar group were large, the results, especially changes of back pain, might be changed. To clarify these problems, the larger series of patients should be analyzed and biomechanical factors, various anatomical factors such as the degree of the facetectomy, characteristics of disc herniation should be included in the future study.
Although we enrolled a small series of patients with upper lumbar herniation in the current study, we suggest that the upper lumbar disc (L1-2 and L2-3) have different clinical characteristics from those of the lower lumbar disc and these include older age, a higher incidence of autonomic dysfunctions, and a greater number of patients with a past history of taking lumbar surgery. There were no significant differences in surgical outcomes for leg pain between the upper lumbar group and the lower one. The back pain of the upper lumbar group was lesser improved comparing with that of the lower one.
References
1. Albert TJ, Balderston RA, Heller JG, Herkowitz HN, Garfin SR, Tomany K, et al. Upper lumbar disc herniations. J Spinal Disord. 1993; 6:351–359. PMID: 8219549.

2. Bartolomei L, Carbonin C, Cagnin G, Toso V. Unilateral swelling of the lower abdominal wall. Unusual clinical manifestation of an upper lumbar disc herniation. Acta Neurochir (Wien). 1992; 117:78–79. PMID: 1387504.
3. Bosacco SJ, Berman AT, Raisis LW, Zamarin RI. High lumbar disk herniations. Case reports. Orthopedics. 1989; 12:275–278. PMID: 2922363.

4. Fontanesi G, Tartaglia I, Cavazzuti A, Giancecchi F. Prolapsed intervertebral disc at the upper lumbar level. Diagnostic difficulties. A report on 12 cases. Ital J Orthop Traumatol. 1987; 13:501–507. PMID: 3503877.
5. Hsu K, Zucherman J, Shea W, Kaiser J, White A, Schofferman J, et al. High lumbar disc degeneration. Incidence and etiology. Spine (Phila Pa 1976). 1990; 15:679–682. PMID: 2218715.

6. Iwasaki M, Akino M, Hida K, Yano S, Aoyama T, Saito H, et al. Clinical and radiographic characteristics of upper lumbar disc herniation : ten-year microsurgical experience. Neurol Med Chir (Tokyo). 2011; 51:423–426. PMID: 21701105.

7. Kim DS, Lee JK, Jang JW, Ko BS, Lee JH, Kim SH. Clinical features and treatments of upper lumbar disc herniations. J Korean Neurosurg Soc. 2010; 48:119–124. PMID: 20856659.

8. Kortelainen P, Puranen J, Koivisto E, Lähde S. Symptoms and signs of sciatica and their relation to the localization of the lumbar disc herniation. Spine (Phila Pa 1976). 1985; 10:88–92. PMID: 3983706.

9. Pásztor E, Szarvas I. Herniation of the upper lumbar discs. Neurosurg Rev. 1981; 4:151–157. PMID: 7301145.

10. Saberi H, Isfahani AV. Higher preoperative Oswestry Disability Index is associated with better surgical outcome in upper lumbar disc herniations. Eur Spine J. 2008; 17:117–121. PMID: 17972115.

11. Sanderson SP, Houten J, Errico T, Forshaw D, Bauman J, Cooper PR. The unique characteristics of "upper" lumbar disc herniations. Neurosurgery. 2004; 55:385–389. discussion 389. PMID: 15271245.

12. Wei CP, Cheng WC, Chang CN, Lee ST, Lui TN, Wang AD. Upper lumbar disc herniation. Changgeng Yi Xue Za Zhi. 1989; 12:193–199. PMID: 2637057.
Fig. 1
Schematic drawings showing distribution of pain or sensory change in 15 patients of upper lumbar group. 1) anterior thigh (n=5), 2) anterolateral thigh (n=3), 3) inguinal (n=1), 4) anterolateral lower leg (n=4), 5) foot dorsum (n=1), 6) buttock (n=13), 7) perianal (n=1), 8) posterolateral thigh (n=7), 9) calf (n=3).
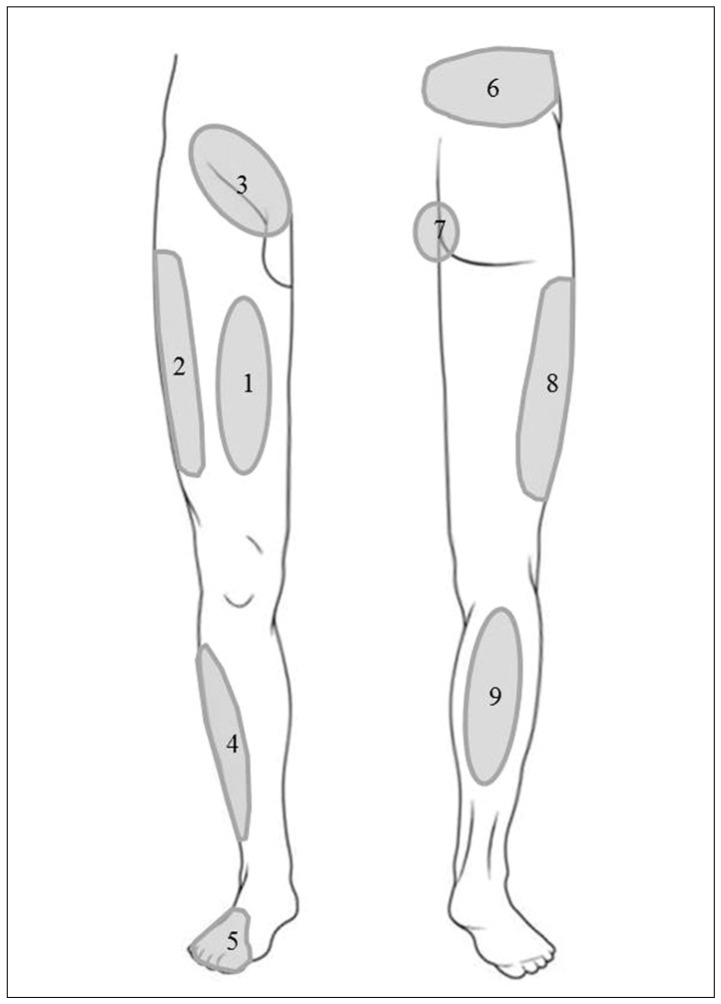
Fig. 2
Comparison of the degree of the reduction in the severity of back pain and leg pain between preoperatively and at 24 month after surgery in upper lumbar (A) and lower lumbar (B) groups. VAS : Visual Analogue Scale, preop : preoperative, f/u : follow-up at 24 months after surgery.
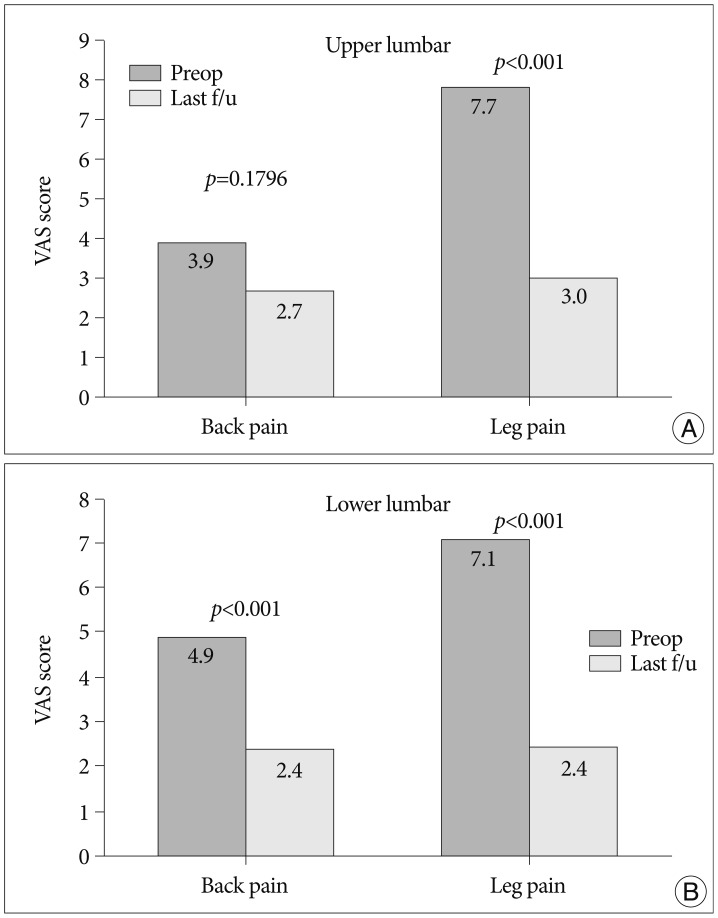
Fig. 3
Comparison of the degree of the reduction in the Oswestry Disability Index between preoperatively and at 24 months after surgery in both groups. preop : preoperative, f/u : follow-up at 24 months after surgery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download