Abstract
Objective
To suggest a new useful diagnostic technique, principles of the selective excitation technique-magnetic resonance images (Proset-MRI), and to know the precise radiologic findings that can prove symptomatic foraminal and extraforaminal stenosis at L5-S1.
Methods
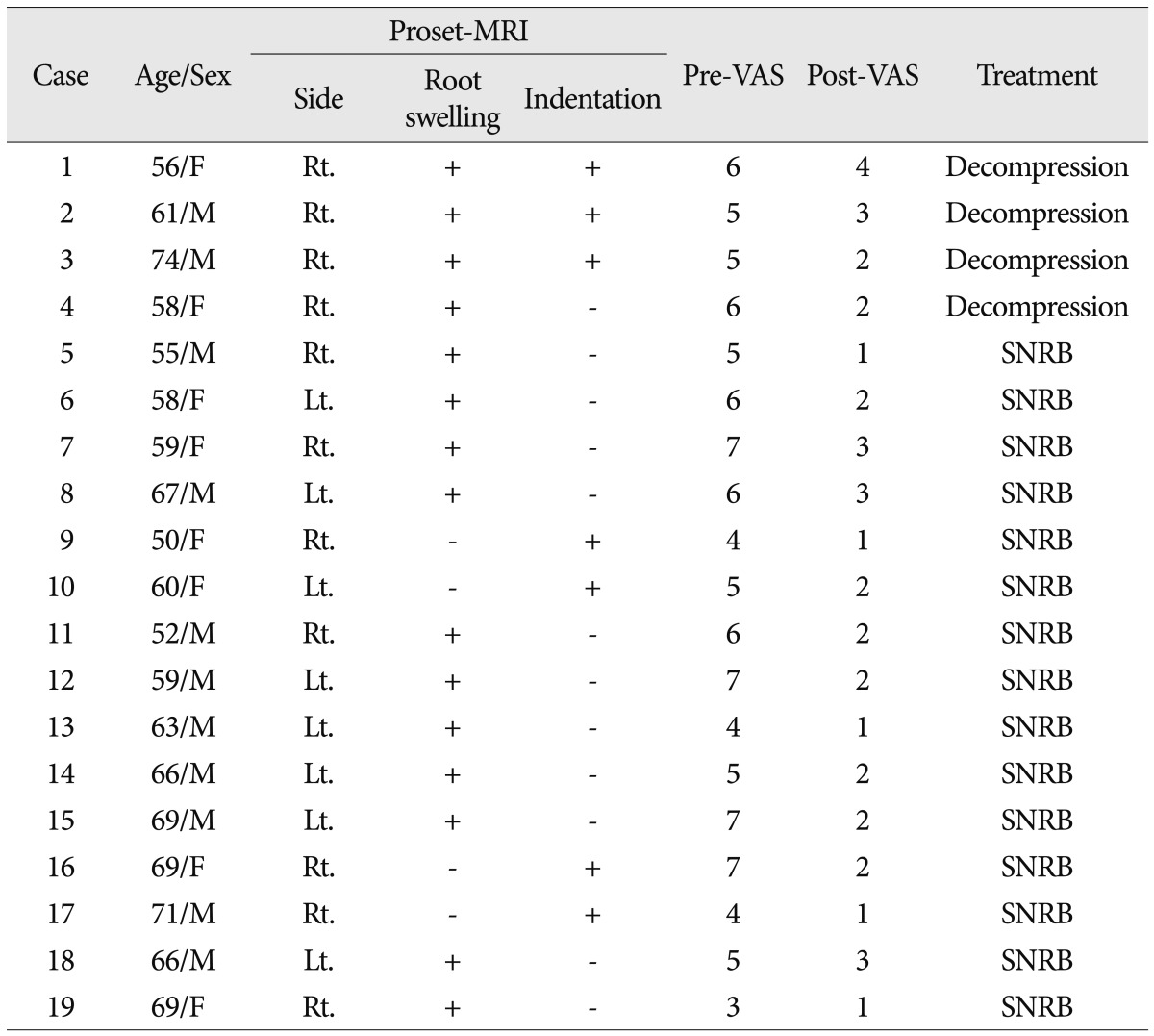
Nineteen patients with symptomatic L5-S1 stenosis were checked by Proset-MRI. Four patients were performed decompressive surgery and 15 patients were performed selective nerve root block (SNRB) at L5. The pain scale of patients was checked by Visual Analogue Scale (VAS) scores at the pre- and post-treatment state.
Results
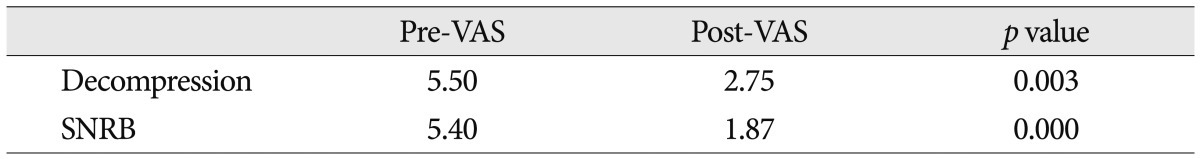
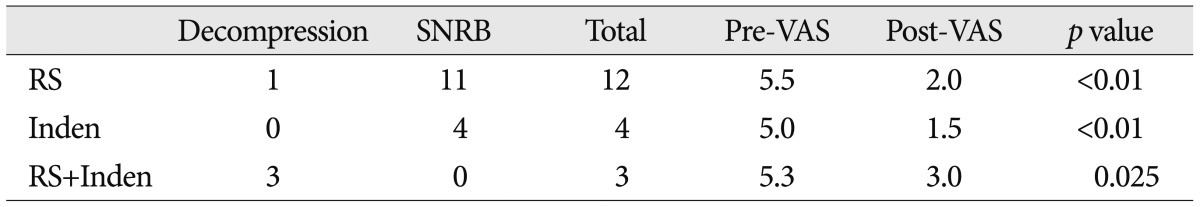
Proset-MRI findings of patients with symptomatic stenosis are root swelling (RS) and indentation. The comparisons with VAS scores had a meaningful statistical result at each RS (p<0.01) and indentation (p<0.01). However, the findings of RS combined with indentation lacked statistical significance (p=0.0249). In addition, according to a comparison with the treatment modalities, reducing of VAS scores had statistical meaningful significance in decompressive surgery cases (p<0.01), and also in SNRB cases (p<0.01) after a 3-month follow-up period.
It is hard to distinguish symptomatic spinal stenosis (SS) from asymptomatic SS in case of patients with radiological multiple stenosis. Especially, the diagnosis of foraminal and extaforaminal stenosis at L5-S1 is also difficult because of bony and ligament structures surrounding this level4). Many radiological modalities were reported to diagnose foraminal and extraforaminal stenosis at L5-S1, such as computed tomography (CT), magnetic resonance image (MRI)8,9,11), magnetic resonance myelography (MRM)6) and so on. If some diagnostic modalities have high concordance between clinical symptoms and radiologic findings, these have high sensitivity for diagnosing foraminal and extraforminal stenosis at L5-S1.
The purpose of this study is to evaluate the usefulness of the new diagnostic technique of principles of the selective excitation technique MRI (Proset-MRI) to know and suggest the precise radiologic findings that can prove symptomatic stenosis at L5-S1.
Twenty-eight patients (15 men, 13 women; mean age, 60.0±10.0 years; range 36-74 years) with foraminal and extraforaminal stenosis at L5-S1, who underwent decompressive surgery or selective nerve root block (SNRB) in the author's hospital between November 2009 and June 2011, were included in this study. However, on 19 patients were enrolled (Table 1). All of them suffered from radiculopathy of L5 dermatome. We performed MRI, inclusive of 3-dimensional coronal fast-field echo (FFE) sequences with selective water excitation using the Proset. To have images of lumbosacral nerve roots and dorsal root ganglion (DRG), the setting of imaging plane is parallel to the longitudinal axis of the lumbosacral spinal canal. For image processing, an Aquarius 3d work station equipped with commercially available automated analysis 3D rendering software (TeraRecon Inc., San Mateo, CA, USA) was used.
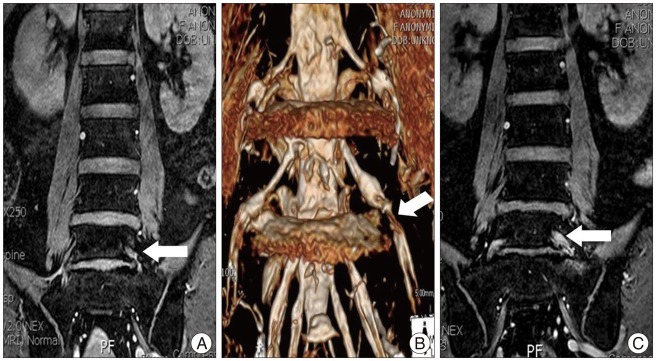
The change of symptomatic L5 nerve root was revealed by root swelling (RS) (Fig. 1) and indentation (Fig. 2). Swelling and indentation of the nerve roots were evaluated on 3D MR rendering images of the lumbosacral spine. These abnormal findings were compared with contralateral asymptomatic side on the same level.
Interobserver variability of the nerve root swelling and indentation was assessed by using the κ statistics. A κ value of less than 0.40 indicated poor agreement; 0.41 to 0.60, moderate agreement; 0.61 to 0.80, substantial agreement; and 0.81 or greater, almost perfect agreement.
Twenty-six patients were evaluated with Proset-MRI before the treatment. Comparison of pre-treatment pain with post-treatment pain was taken by Visual Analogue Scale (VAS) scores. Seven of the 26 cases were excluded from the study because 2 decompressive surgeries and 2 SNRB cases were not evaluated for VAS scores, and 3 SNRB cases were dropped due to follow-up loss. Finally, 4 decompressive surgery and 15 SNRB cases were included in our study. All of the including cases were taken pre-treatment Proset-MRI, which also revealed nerve root swelling and/or indentation. The Mann-Whitney U test was used for analysis of nonparametric data. p<0.01 was considered to be statistically significant.
According to the meaningful Proset-MRI findings of symptomatic stenosis, the pre- and post-treatment VAS have a statistical significance (p<0.01) at the RS and indentation. However, comparison with Proset-MRI cases combining RS with indentation do not have any statistical significance (p=0.025) (Table 2).
According to the treatment modalities, we compared with VAS scores before and after treatment. On the decompression case, there are 4 patients (2 men, 2 women; mean age, 62.3±8.1 years; range 56-74 years). On the Proset-MRI, 3 cases revealed nerve root swelling and indentation, and 1 case revealed only nerve root swelling. Two cases were added postoperative one-month Proset-MRI, which revealed diminished nerve root swelling, but indentation was resolved partially (Fig. 2C). In addition, VAS scores of these patients reduced from 5.50 to 2.75 (p<0.01) after over 3 months of a follow-up period. On the SNRB case, there are 15 patients (9 men, 6 women; mean age, 62.2±6.6 years; range 50-71 years). On the Proset-MRI, 11 cases revealed only nerve root swelling, and 4 cases revealed only indentation of the nerve root, but there is no case that reveals combining nerve root swelling with indentation. Further, VAS scores of these patients reduced from 5.40 to 1.87 (p<0.0001) after a 3-month follow-up period (Table 3). Agreement with respect to the recognition of nerve root swelling and indentation was excellent (κ=0.86 and 0.78).
According to the conventional MRI, central and lateral stenosis can be seen easily. Unlike central and lateral stenosis, the diagnosis of foraminal and extraforaminal stenosis at L5-S1 is very difficult and vague. That is often caused by the narrow space between L5 transverse process and sacral ala. These pathologic conditions were described as the term, such as far-out syndrome, lumbosacral tunnel, lumbosacral bony tunnel (LSBT)3,4), and so on. Although many clinicians think there is no doubt that foraminal or extraforaminal stenosis at L5-S1 is diagnosed via the conventional MRI2), such patients do not complain of severe stenotic symptoms. Many studies were reported to diagnose foraminal and extraforaminal stenosis at L5-S1 precisely and many clinicians tried to match up patient's symptoms with radiologic findings.
Lee et al.8) reported that reliable conventional MR findings of extraforaminal with or without foraminal disk herniation are focal eccentricity of the disk contour, obliteration of the epidural fat surrounding the nerve root, change in the thickness of the nerve root, and displacement of the nerve root. However, there are many cases of incorrect diagnoses or unmatched clinical and radiological findings. Moon et al.9) studied the reliability of MRI findings in detecting symptomatic lesions and they reported the most reliable findings of symptomatic lesions, which is the focal eccentricity of the disc. However, this study has a limitation of confirming the symptomatic lesion owing to not adding and comparing with the other imaging protocols. Nakao et al.10) also studied to diagnose the extraforaminal stenosis at the lumbosacral junction. They used 3-dimensional CT imaging of LSBT surrounding the L5 transverse process, L5 vertebral body, and sacral ala at the extraforaminal lesion. Kim et al.7) studied using the coronal source images of MRM. MRM provides the precise coronal images that are close to the operative views, and two useful findings are DRG swelling and abnormal running course of L5 exiting nerve root. However, this study had low sensitivity to detecting the meaningful findings of MRM, such as DRG swelling and running course abnormality. In addition, Heo et al.5) also studied using an oblique MRI that is parallel to the connecting the posterior margin of the upper to lower endplate of the affected level's functional segmental unit. Through this MR modality, they knew the relationship of the nerve root, DRG, lumbar spinal nerve root of foraminal and extraforaminal stenosis, and could detect the symptomatic lesions compared with the aymptomatic contralateral side. However, this study also has a limitation in diagnosing the symptomatic lesion. This modality may fail to clearly reveal foraminal and extraforaminal anatomy in patients with spinal deformities, such as scoliosis or severe lordosis.
Proset-MRI was first suggested by Borthne et al.1) to obtain excellent bowel image. The principle of this modality is a selective excitation to suppress either fat or water by exploiting the difference between the water and fat resonance frequencies. SI of fat can be suppressed, and then SI of water can be revealed. Through this principle, we used the Proset-MRI to see the status of nerve root images at the lumbosacral space with three dimensional coronal FFE sequences. We confirmed the symptomatic site through SNRB. If pain and/or radiculopathy are provocated and relieved during SNRB, we confirmed as symptomatic stenosis. According to these symptomatic stenotic lesions, we could know the definite findings of symptomatic lesion at three dimensional Proset-MRI that had root swelling and/or indentation. In addition, when the pain and/or radiculopathy symptoms are relieved after decompressive surgery at foraminal and extraforaminal stenosis, we detected the same reliable three dimensional Proset-MRI findings.
There are some limitations of our study. When there are reliable symptomatic findings of Proset-MRI, we will predict good results after SNRB or decompressive surgery. However, we do not have long-term follow-up data that may show the degree of reducing nerve root swelling and/or root indentation. Although we obtained meaningful results of pain, we do not know the precise expectant radiological period to obtain good effects of treatments and indication of each treatment options. We did not know the exact degree of RS and indentation to induce the symptoms. The degree to induce the symptoms can provide us to detect the accurate period of treatment. In our study, we had one-month follow-up with Proset-MRI at decompressive surgery of only two patients. These patients' findings of Proset-MRI showed only a reduction in nerve root swelling, and not fully recovered indentation. Although there was remained indentation of nerve root, patients' VAS scores had good meaningful result with statistical significance. We do not exactly know the asymptomatic cases with abnormal Proset-MRI findings because we just reviewed the abnormal radiologic changes combined with clinical symptoms. Therefore, we need further studies with many pretreatment cases of Proset-MRI and evaluate the status of posttreatment Proset-MRI.
We think that the three dimensional Proset-MRI can be a very useful and sensitive technique to diagnose the symptomatic foraminal and extraforaminal stenosis at L5-S1. Therefore, we can see root swelling and indentation that are the most important radiological findings to match clinical symptoms more accurately by this Proset-MRI. Further studies and long-term follow-up will be necessary to verify the clinical usefulness of the three dimensional Proset-MRI in these patients.
References
1. Borthne AS, Dormagen JB, Gjesdal KI, Storaas T, Lygren I, Geitung JT. Bowel MR imaging with oral Gastrografin : an experimental study with healthy volunteers. Eur Radiol. 2003; 13:100–106. PMID: 12541116.

2. Byun WM, Ahn SH, Ahn MW. Significance of perianular enhancement associated with anular tears on magnetic resonance imagings in diagnosis of radiculopathy. Spine (Phila Pa 1976). 2008; 33:2440–2443. PMID: 18923321.

3. Ebraheim NA, Xu R, Huntoon M, Yeasting RA. Location of the extraforaminal lumbar nerve roots. An anatomic study. Clin Orthop Relat Res. 1997; 230–235. PMID: 9224261.

4. Elster AD. Bertolotti's syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976). 1989; 14:1373–1377. PMID: 2533403.
5. Heo DH, Lee MS, Sheen SH, Cho SM, Cho YJ, Oh SM. Simple oblique lumbar magnetic resonance imaging technique and its diagnostic value for extraforaminal disc herniation. Spine (Phila Pa 1976). 2009; 34:2419–2423. PMID: 19829256.

6. Kang SH, Choi SH, Seong NJ, Ko JM, Cho ES, Ko KP. Comparative study of lumbar magnetic resonance imaging and myelography in young soldiers with herniated lumbar disc. J Korean Neurosurg Soc. 2010; 48:501–505. PMID: 21430976.

7. Kim SB, Jang JS, Lee SH. Morphologic changes of L5 root at coronal source images of MR myelography in cases of foraminal or extraforaminal compression. J Korean Neurosurg Soc. 2009; 46:11–15. PMID: 19707488.

8. Lee IS, Kim HJ, Lee JS, Moon TY, Jeon UB. Extraforaminal with or without foraminal disk herniation : reliable MRI findings. AJR Am J Roentgenol. 2009; 192:1392–1396. PMID: 19380567.

9. Moon KP, Suh KT, Lee JS. Reliability of MRI findings for Symptomatic Extraforaminal Disc Herniation in Lumbar Spine. Asian Spine J. 2009; 3:16–20. PMID: 20404941.

10. Nakao S, Yoshida M, Yamada H, Hashizume H. A new 3-dimensional computed tomography imaging method to diagnose extraforaminal stenosis at the lumbosacral junction. J Spinal Disord Tech. 2010; 23:e47–e52. PMID: 20924293.

11. Yoshida H, Fujiwara A, Tamai K, Kobayashi N, Saiki K, Saotome K. Diagnosis of symptomatic disc by magnetic resonance imaging : T2-weighted and gadolinium-DTPA-enhanced T1-weighted magnetic resonance imaging. J Spinal Disord Tech. 2002; 15:193–198. PMID: 12131418.

Fig. 1
The right L5 nerve root swelling (arrow) at Proset-MRI. A : Coronal Proset-MRI. B : Three-dimensional Proset-MRI. Proset-MRI : principles of the selective excitation technique-magnetic resonance images.
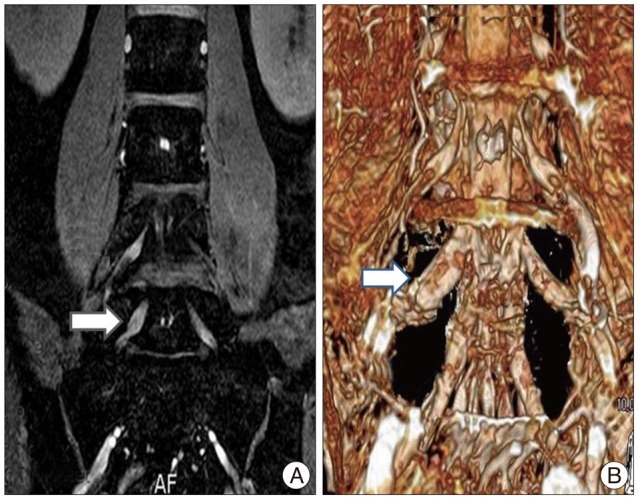
Fig. 2
The left L5 nerve root indentation (arrow) at Proset-MRI. A : Coronal Proset-MRI. B : Three-dimensional Proset-MRI. C : Not fully reducing of indentation at postoperative one-month follow-up Proset-MRI. Proset-MRI : principles of the selective excitation technique-magnetic resonance images.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download