Abstract
Objective
Spinal dysraphism defects span wide spectrum. Wound dehiscence is a common postoperative complication, and is a challenge in the current management of cerebrospinal fluid (CSF) leaks and wound healing. The purpose of this study is to evaluate the risks of CSF-related morbidity in the surgical treatment of spinal dysraphism.
Methods
Ten patients with spinal dysraphism were included in this retrospective study. The median age of the cohort was 4.8 months. To assess the risk of CSF morbidity, we measured the skin lesion area and the percentage of the skin lesion area relative to the back surface for each patient. We then analyzed the relationship between morbidity and the measured skin lesion area or related factors.
Results
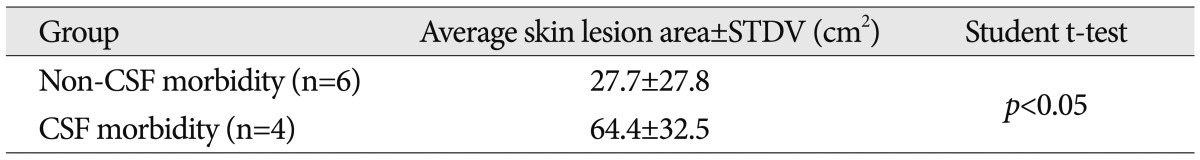
The overall median skin lesion area was 36.2 cm2 (n=10). The percentage of the skin lesion area relative to the back surface ranged from 0.6% to 18.1%. During surgical reconstruction, 4 patients required subsequent operations to repair CSF morbidity. The comparison of the mean area of skin lesions between the CSF morbidity group and the non-CSF morbidity group was statistically significant (average volume skin lesion of 64.4±32.5 cm2 versus 27.7±27.8 cm2, p<0.05). CSF morbidity tended to occur either when the skin lesion area was up to 44.2 cm2 or there was preexisting fibrosis before revision with an accompanying broad-based dural defect.
Spinal dysraphism refers to various forms of congenital malformation caused by neural tube defects during different stages of embryogenesis, specifically neurulation. Pathophysiologically, dysraphisms are derived from three different stages of embryogenesis : primary neurulation, secondary neurulation, and gastrulation. The various disease spectrums are characterized by individual anomalies of defects such as meningocele, myelomeningocele, lipomeningocele, lipomyelomeningocele, spinal lipoma, and so forth. From the surgical perspective, however, these disease spectrums can be classified morphologically as open or 225closed neural tube defects, including the transitional type. Open and closed dysraphisms are distinguished by the presence or absence of visible overlying full-thickness skin coverage11,12).
The prevalence of spinal dysraphism has been on the decline worldwide during the past two decades, as a consequence of better maternal nutrition, timely folate replacement, and better prenatal care with high-resolution ultrasound giving women the option of terminating a pregnancy when such a defect is diagnosed in the fetus. In addition, a liberal assay of maternal serum alpha-fetoprotein is also an important contributing factor for prenatal diagnosis2).
Management of spinal dysraphism aims to provide immediate closure of the neural tube followed by closure of the dura and the skin without any undesirable tension. The most important surgical procedures are; 1) identifying the neural placode as well as the intermediate epithelial layer, which is bounded by the skin, pia, arachnoid, and dura, 2) carefully preserving neural tissue, 3) subsequently reconstituting the normal neural environment, and 4) finally closing the complete skin to prevent cerebrospinal fluid (CSF) leaks3). Regarding the timing of surgical intervention, early primary closure is often closely related to an excellent outcome although the risk of neurological sequelae varies depending on the severity of the anomalies. Large skin defects require additional intervention and present complications including wound dehiscence, wound infection, and CSF leaks. The morbidities of wound healing and CSF leaks during surgical management remain challenges to the current management of spinal dysraphism.
The objective of this study was to evaluate the relationship between skin lesion size and the risk of CSF morbidity, including wound dehiscence in surgical treatment. Related articles are reviewed to identify the optimal surgical strategy in managing-wound- and CSF-related morbidity.
A retrospective study was conducted among 10 patients with spinal dysraphism who underwent reconstructive surgery at our neurosurgical service and affiliated hospital for humanitarian aid in Afghanistan during 2010 and 2011. All patients were subjected to a thorough history-taking and complete neurological assessment. The clinical data was collected and analyzed to investigate factors related to wound dehiscence, CSF leaks, and their management.
The patients were divided into two groups; 6 had open dysraphism, and 4 had closed dysraphism. The age of the patients ranged from 8 days to 48 years, with a median age of 4.8 months. The patients included 8 males and 2 females. Of the 10 patients, 5 had a lumbosacral lesion, 4 had an upper or lower lumbar lesion, and 1 had a thoracic lesion.
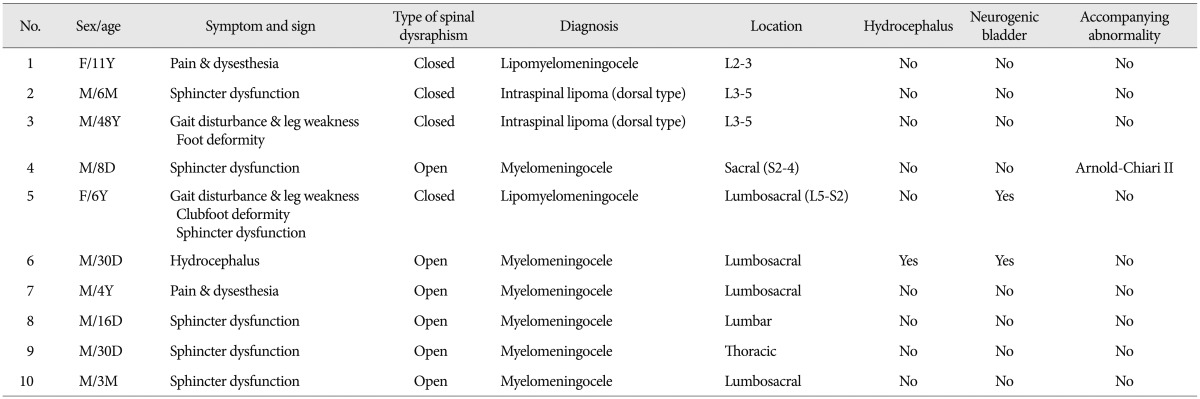
The patients presented with a wide variety of signs and symptoms in combination with cutaneous, orthopedic, spinal, anorectal, and urological abnormalities. In our study, 2 patients had gait disturbance and leg weakness, 2 patients had leg pain and dysesthesia, 2 patients had clubfoot deformity, and 6 patients had bowel and urinary incontinence, the most common clinical presentation or symptom. All patients underwent one or more imaginge studies, including sonography, CT, or MRI. One of the 10 patients had hydrocephalus, and another patient had type II Arnold-Chiari malformation at the time of surgery. The clinical characteristics of the enrolled patients are summarized in Table 1.
To measure the skin lesion area, the patients were classified into two groups according to the shape of the mass (e.g., round or elliptical). Then each skin lesion was measured using one of the following equations according to its shape. For a round lesion, we used π×r2 (where r is the radius) and π× [(R+r)/2]2 (where R is the long radius and r is the short radius) (Fig. 1) for an elliptical lesion4,16).
Total body surface area (TBSA) was measured using the following equation to calculate the percentage of the skin lesion area related to the back surface of each patient : TBSA (m2)={[body weight (kg)×4]+7}/[body weight (kg)+90]. The back surface was calculated according to the "rule of nines", which says that the back constitutes 18% of the total body surface area4). The percentage of the skin lesion area relative to the back surface area was also measured in individual patients to elucidate the relationship between wound complication and the size of the defect area.
Dural defects were also categorized as small or broad defects, which were defined as the dural prolapse through stalk-like lesions and broad-based dural prolapse lesions, respectively.
The statistical test was measured using GraphPad Prism (Version 5.01, GraphPad Software Inc., La Jolla, CA, USA).
Surgical reconstruction was performed on all enrolled patients to preserve the neural component and prevent subsequent infection. The surgical procedure involved closing the skin and dural defects and releasing the filum terminale to eliminate the tethered cord. The skin closure method was determined according to the percentage of the skin lesion over the back surface area.
For example, Fig. 2 shows the surgical procedure for case 6, a patient who had a round mass lesion at the lumbosacral junction with a diagnosis of myelomeningocele. The center of the myelomeningocele was a transparent yellowish membrane, which implies the neural placode. An incision was made between the lateral margin of the placode and the intermediate epithelial layer to optimally dissect the neural structure. The margin of the neural placode, central canal, and primitive neural groove was identified. After the placode was dissected from the epithelial layer, dissection of the dura started from the lateral margin and moved toward the rostral and the caudal poles. Once the surrounding structures were entirely separated, the placode was closed into a tube using 5-0 Prolen. Then the dural was closed in a watertight manner using either the original redundant dura directly or using dural substitutes such as lyophilized dura, fascia lata, or lumbosacral muscle fascia. Myofascial coverage over bony defects (dysraphic vertebrae) is also a useful procedure for preventing CSF leaks following reconstruction, primarily in the case of large anomalous defects. Finally, various surgical skin-closure techniques were used to minimize tension on the skin to facilitate successful wound healing. These methods included V-Y plasty, Z-plasty, and S-plasty. In most of the surgeries, wound reconstruction was successfully performed using S-plasty and Z-plasty.
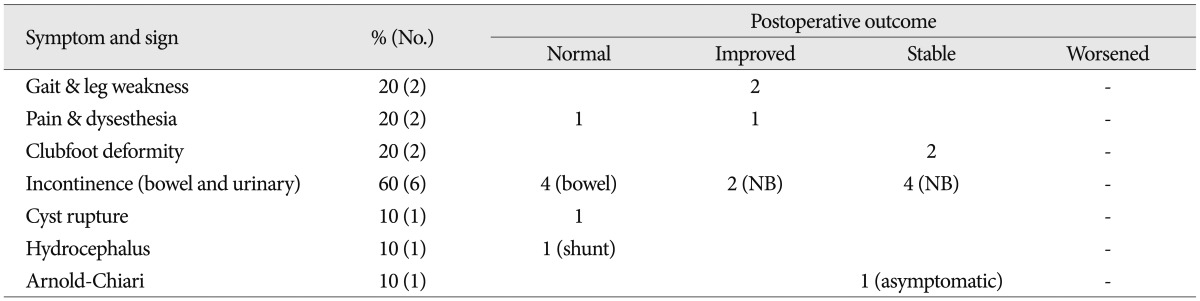
After surgery, 4 patients who had gait disturbance and leg weakness as well as leg pain and dysesthesia improved. All 4 patients with bowel incontinence also returned to normal. Bladder incontinence remained in a total of 6 patients, but neurogenic bladder symptoms improved slightly in 2 of the patients, and the other 4 were stable condition after the surgery. The clinical outcomes for the enrolled patients are summarized in Table 2.
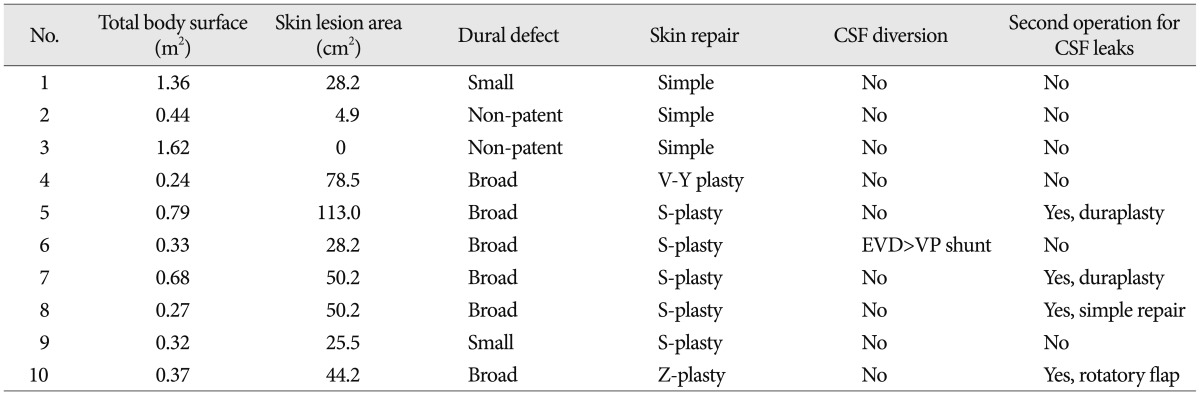
Regarding the shape of the skin lesion (Table 3), 5 patients were classified as having an elliptical lesion, and 4 patients had a round lesion. Only 1 patient showed a small skin dimple (Case 3 in Table 4) . The radius of the elliptical lesion ranged from 1.0×1.5 cm for the smallest lesion area to 3.5×4.5 cm for the largest lesion area. The surface area of the elliptical lesion was calculated in the range of 4.9 to 50.2 cm2. The average skin lesion area was 30.6 cm2 with a median lesion area of 28.2 cm2. The percentage of skin lesion over the back surface area ranged from 0.6% to 10.3% with an average of 4.6% (median percentage of 4.4%) in the elliptical lesion group. The radius of the round lesion ranged from 3 to 6 cm. The surface area was calculated, and the range was 28.2 to 113.0 cm2. The average area of the round skin lesion was 67.5 cm2, and the median area was 64.3 cm2. The percentage of the skin lesion ranged from 4.1% to 18.1% with an average of 8.7% (with thea median defect percentage 6.3%) in the round-skin lesion group. The average skin lesion area in both groups was 47.0 cm2 with a median defect area of 44.1 cm2. The average skin lesion percentage over the surface of the back was 6.4% with a median percentage of 4.7% in both groups (n=9). In terms of the pattern of dural defects, 2 patients had a small dural defect, and 6 had a broad-based dural defect.
The skin was closed using S-plasty in 5 patients and Z-plasty and V-Y plasty in 1 patient each. For the remaining 3 patients, a direct single closure was performed (Table 4). The patient with hydrocephalus initially underwent an external ventriculostomy eventually followed by a VP shunt.
Subsequent surgical intervention was required by 4 patients to repair a pseudomeningocele, CSF leak, or wound dehiscence. Wound morbidity was successfully controlled with second-look duraplasty in 2 patients and direct secondary closure in 1 patient. A 3-month-old patient with a myelomeningocele and a large skin lesion and dural defect, which covered 6.6% of the surface of the back in the lumbosacral region, subsequently required an extensive rotatory flap operation to treat recurrent wound dehiscence and CSF leaks.
Based on the results of the skin lesion measurement and surgical outcomes, the patients were divided into two groups : a non-CSF morbidity group of 6 patients and a CSF morbidity group of 4 patients. When the average area of the skin lesion is compared between the CSF morbidity group and the non-CSF morbidity group, there is statistically a significant difference (p=0.045, one-tailed unpaired Student t-test). The average skin lesion area was significantly larger in the CSF morbidity group than in the non-CSF morbidity group since the mean skin lesion area was 64.4±32.5 cm2 versus 27.7±27.8 cm2, respectively (Table 5). Although CSF morbidity mostly tended to occur in patients with large skin lesions, there was no statistically significant difference between the two groups when the percentage of skin lesion over the back surface area and CSF morbidity was compared (p=0.26). Among those in the CSF morbidity group, the patient in case 7 had several years' history of previous postoperative scarring before this definitive reconstructive surgery.
The case 4 patient also had a 78.5 cm2 skin lesion, relatively large compared to the average in the non-CSF group. A V-Y skin plasty effectively succeeded in complete reconstruction in spite of a concomitant broad dural defect.
Spinal dysraphism include a wide spectrum of dysraphic abnormalities caused by neural tube defects during the different stages of embryogenesis. Embryogenetically, spinal dysraphic malformations can be classified as primary or secondary neurulation or gastrulation lesions.
The spectrum of this disease varies according to the degree of dysraphic defects occurring during the embryogenetic stages of anomaly development. Often, spinal dysraphism stratifies into two types according to the presence of full thickness of skin coverage over the dysraphic prolapse of the dura or neural elements. One is the open form of spinal dysraphism, which is characterized by exposing the neural placode to the environment through a congenital bony defect. Myelomeningocele, myelocele, hemimyelomeningocele, hemimyelocele, and other abnormalities are included in this form. The other is the closed form of spinal dysraphism. In a closed dysraphism, the neural placode is entirely covered by skin. The spectrum of the closed form includes lipomyelomeningocele, intradural lipoma, dermal sinus, diastematomyelia, and so forth6,7,11,12).
Worldwide, the incidence of neural tube defects varies from 0.17 to 6.39 per 1000 live births. Myelomeningocele is the most common type of neural tube defect. The prevalence of myelomeningocele has decreased remarkably because of several factors : the improvement in nutrient and folic acid supplements and the development of prenatal diagnosis with consequent termination of affected fetuses2).
The principle of surgical treatment is to restore a wide range of structural defects to prevent the development of tethered cord syndrome or related morbidities that result in infection or other neurological and orthopedic sequelae3). Identifying the optimal timing of surgical reconstruction is an important issues for obtaining better therapeutic outcomes. A randomized control trial1) was conducted to compare prenatal with postnatal surgery in treating myelomeningocele. Although prenatal surgery had better neurological outcomes than postnatal surgery at 30 months, the study had to be terminated because early intervention was strongly associated with increasing the risk of maternal and fetal morbidity. Consequently, the optimal timing of surgical intervention is now as early as possible in the postnatal period or generally between 3 and 6 months.
Pang et al.9,10) reported on the long-term outcomes of surgical reconstruction of spinal cord lipoma. The surgical results and overall outcomes were significantly affected by residual lesions detected with MRI and morbidities including CSF leaks and wound infection and dehiscence in particular. Immediate and delayed complications of the surgery are closely related to wound dehiscence. Pseudomeningocele and CSF fistula are common surgical complications during the period the wound is healing. CSF morbidity is the major challenge. Great effort has been devoted to reducing wound complications and CSF morbidity.
Skin wound and CSF leak repair techniques are a matter of tension following the early phase of surgery. Regarding the optimal wound closure method, various skin reconstruction methods have been introduced, such as S-plasty, basic Z-plasty, and V-Y plasty. S-plasty5,14), or "lazy S", is a variation of the fusiform excision that effectively increases the total length of the scar while keeping the linear distance between the two apices constant. This technique redirects the tension vectors to eliminate standing cones and improves the cosmetic outcome by orienting the ends of the wound away from the areas of maximal convexity. Additionally, S-plasty functions to reduce suture-line traction and thus facilitates wound healing, decreasing the likelihood of central scar depression. Basic Z-plasty13) involves creating two triangular flaps of equal dimension that are then transposed. The flap area is created using an angle of 60 degrees. In practice, the lengthening and reorientation are less, owing to increased wound tension. Z-plasty is reserved for improving thin linear scars and is not used as a primary closure technique. Turhan Haktanir et al.17) covered a skin defect with dural repair using bilateral fasciocutaneous flaps in 5 patients with large myelomeningoceles.
Multiple factors are associated with surgical outcomes and a high rate of symptomatic recurrence of myelomeningocele. Effort was made to identify factors that affect surgical outcomes. The risk of a CSF leak increases in patients who have hydrocephalus or Arnold-Chiari malformation and spinal dysraphism as the size of the defect increases15). Generally, early adequate intervention with CSF diversion procedures effectively provides CSF pressure through the reconstruction wound. Managing intrathecal CSF pressure includes external ventriculostomy, ventriculoperitoneal shunt, temporary lumbar drainage, and foramen magnum decompression for the Arnold-Chiari malformation, including the recent use of dural grafts, which are of either synthetic collagen material or allograft dura. Narotam et al.8) reported that collagen matrix reduced CSF leaks in 95% of patients requiring dural repair following spinal surgery.
Detailed objective data showing the relationship between the degree of the dysraphic defect and the risk of wound complications, specifically CSF- and wound-related morbidity, is lacking. Ghozlan and Eisa4) analyzed the size of skin defects and calculated the percentage of the defect over the thoracolumbar region using the TBSA and the "rule of nines". The equation for calculating the defect area for elliptical defects differed from the authors' calculation method. They presented a technique for closing broad-based myelomeningocele defects using bilateral inter-connected latissimus dorsi myocutaneous and gluteal region fasciocutaneous flaps without lateral relaxing flank incisions in the thoracolumbar and lumbosacral lesion. They did not encounter any major wound complication or CSF leaks. There are methods that use dural substitutes to reduce CSF leaks.
In our study, we intended to elucidate the relationships between the extent of an anomalous skin lesion and CSF morbidity. The risk parameters of CSF morbidity were analyzed by measuring and calculating skin lesion and dura defects by comparing the surgical methods and the measurement results. Although the number of patients in our study was limited, CSF morbidity was closely associated with a large skin-lesion area of more than 44.2 cm2 in the CSF morbidity group with broad-based dura defects (Fig. 3). The other risk factor for CSF leaks is residual or incomplete initial surgical reconstruction, which was demonstrated by case 7. Previous postoperative scarring may interfere with adequate wound healing, which results in increasing risk of wound morbidity.
Although the percentage of the skin lesion area over the back surface area did not show a statistically significant result in our study, about 5% of the skin lesion area relative to the back surface may tend to increase the risk of CSF leaks when simple applicable skin plasty was used for wound reconstruction. There were some limitations in our study. The small number of cases was due to the difficulty recruiting an adequate number of dysraphic anomalous patients in recent years. For a patient with a large skin lesion area greater than 78.5 cm2 (as in case 4) with an accompanying broad dura defect, V-Y skin plasty or more extensive rotatory skin flaps leads to success in effective and complete reconstruction of the dysraphic lesion. In addition, second-look duraplasty may localize and minimize the extent of the CSF leak site from the dura reconstruction over time, while allograft or synthetic dura effectively manages the pressure gradient between the spinal dura sac and the pseudomeningocele space, which may allow a certain degree of wound healing to proceed from the initial operation, resulting in satisfactory localization of CSF leaks over time.
A large skin lesion with the prolapse of the neural element into a broad-based dura defect was more likely to increase CSF and wound morbidity. Assessing skin lesions and dural defects by measuring the skin lesion area and the percentage of the skin lesion area over the back surface and related surgical parameters offers useful predictors for anticipating the risk of wound problems and can consequently lead to selecting the optimal procedures for successful reconstruction in treating spinal dysraphism.
References
1. Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011; 364:993–1004. PMID: 21306277.

2. Bowman RM, Boshnjaku V, McLone DG. The changing incidence of myelomeningocele and its impact on pediatric neurosurgery : a review from the Children's Memorial Hospital. Childs Nerv Syst. 2009; 25:801–806. PMID: 19326126.

3. Chapman PH, Davis KR. Surgical treatment of spinal lipomas in childhood. Pediatr Neurosurg. 1993; 19:267–275. discussion 274-274. PMID: 8398852.

4. Ghozlan NA, Eisa AM. Reconstruction of broad-based myelomeningocele defects : a modified technique. Egypt J Plast Reconstr Surg. 2007; 31:213–219.
5. Kim P, Kim HJ. S-plasty--clinical applications for skin surgery. Aust Fam Physician. 2011; 40:224–225. PMID: 21597534.
6. La Marca F, Grant JA, Tomita T, McLone DG. Spinal lipomas in children : outcome of 270 procedures. Pediatr Neurosurg. 1997; 26:8–16. PMID: 9361112.

7. Müller F, O'Rahilly R. The development of the human brain, the closure of the caudal neuropore, and the beginning of secondary neurulation at stage 12. Anat Embryol (Berl). 1987; 176:413–430. PMID: 3688450.

8. Narotam PK, José S, Nathoo N, Taylon C, Vora Y. Collagen matrix (DuraGen) in dural repair : analysis of a new modified technique. Spine (Phila Pa 1976). 2004; 29:2861–2867. discussion 2868-2869. PMID: 15599291.

9. Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode : part I-surgical technique. Neurosurgery. 2009; 65:511–528. discussion 528-529. PMID: 19687697.
10. Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode, part II : outcome analysis and preoperative profiling. Neurosurgery. 2010; 66:253–272. discussion 272-273. PMID: 20042988.
11. Quiñones-Hinojosa A, Schmidek HH. Schmidek & Sweet operative neurosurgical techniques : indications, methods, and results. Philadelphia, PA: Elsevier/Saunders;2012.
12. Rossi A, Cama A, Piatelli G, Ravegnani M, Biancheri R, Tortori-Donati P. Spinal dysraphism : MR imaging rationale. J Neuroradiol. 2004; 31:3–24. PMID: 15026728.
13. Salam GA, Amin JP. The basic Z-plasty. Am Fam Physician. 2003; 67:2329–2332. PMID: 12800961.
14. Sebastian S, Bang RH, Padilla RS. A simple approach to the S-plasty in cutaneous surgery. Dermatol Surg. 2009; 35:1277–1279. PMID: 19469794.

15. Siasios J, Kapsalaki EZ, Fountas KN. Surgical management of patients with Chiari I malformation. Int J Pediatr. 2012; 2012:640127. PMID: 22811732.

16. Spears CP. Volume doubling measurement of spherical and ellipsoidal tumors. Med Pediatr Oncol. 1984; 12:212–217. PMID: 6727778.

17. Turhan Haktanir N, Eser O, Demir Y, Aslan A, Köken R, Melek H. Repair of wide myelomeningocele defects with the bilateral fasciocutaneous flap method. Turk Neurosurg. 2008; 18:311–315. PMID: 18814125.
Fig. 1
Measurement of elliptical skin lesion area (R is the long radius, and r is the short radius).
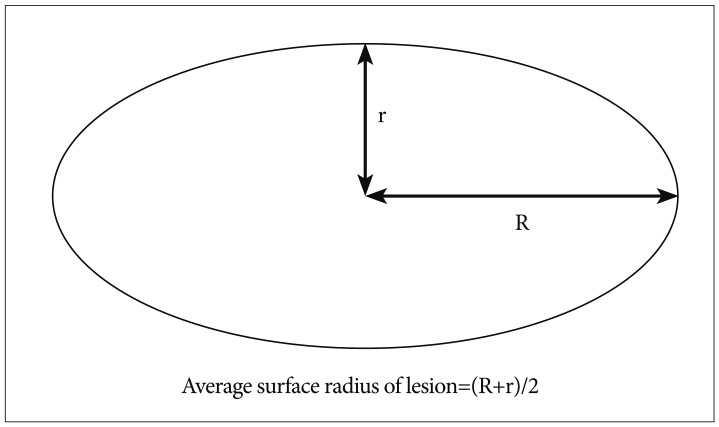
Fig. 2
Case 6. A : Gross finding of myelomeningocele (the asterisk with the closed black arrow denotes the neural placode). B : Incise and dissect between the neural placode and intermediate epithelial layer to identify the neural placode, intermediate epithelial layer, skin, and the pia, arachnoid, and dura mater. C : Approximating paraspinal muscle fascia. D : Skin closure with S-plasty.
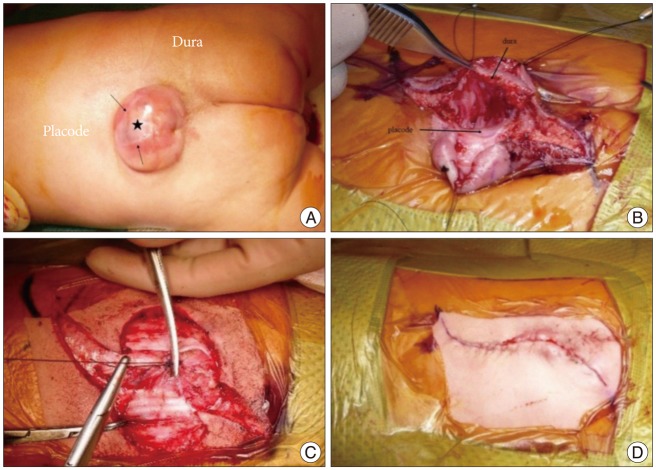
Fig. 3
Graph of box and whisker plot in comparison of two groups; CSF morbidity versus non-CSF morbidity. CSF morbidity group shows significantly larger skin lesion area than that of non-CSF morbidity group (The average skin lesion area of 64.4±32.5 cm2 versus 27.7±27.8 cm2, respectively, p=0.045, one tailed unpaired Student t-test). CSF : cerebrospinal fluid.
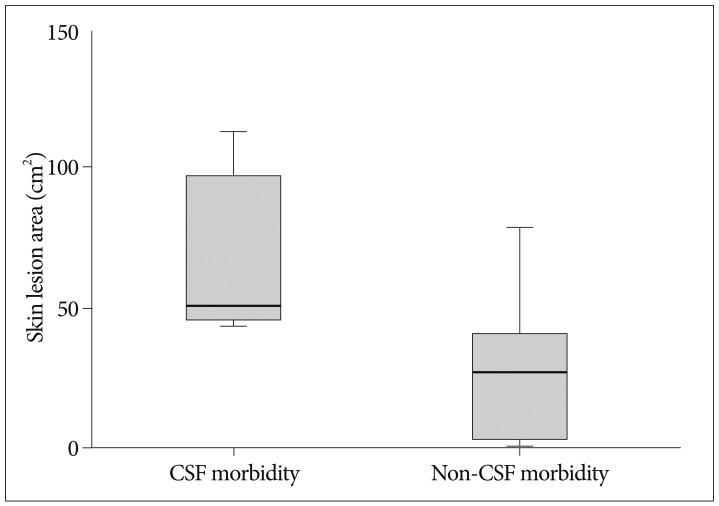
Table 3
Measurement of the skin lesion area and percentage skin lesion area relative to back surface
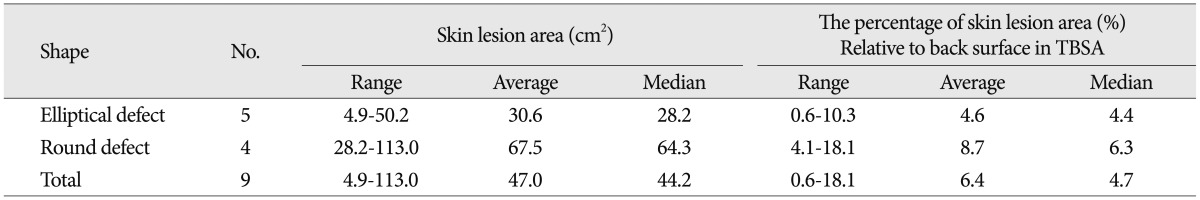
An unmeasurable skin lesion of case 3 which was shown in Table 4 was excluded in this measurement. TBSA : total body surface area




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download