1. Albayram S, Selcuk H, Kara B, Bozdag E, Uzma O, Kocer N, et al. Thromboembolic events associated with balloon-assisted coil embolization: evaluation with diffusion-weighted MR imaging. AJNR Am J Neuroradiol. 2004; 25:1768–1777. PMID:
15569744.
2. Bendszus M, Koltzenburg M, Burger R, Warmuth-Metz M, Hofmann E, Solymosi L. Silent embolism in diagnostic cerebral angiography and neurointerventional procedures: a prospective study. Lancet. 1999; 354:1594–1597. PMID:
10560674.

3. Debrun GM, Aletich VA, Kehrli P, Misra M, Ausman JI, Charbel F. Selection of cerebral aneurysms for treatment using Guglielmi detachable coils: the preliminary University of Illinois at Chicago experience. Neurosurgery. 1998; 43:1281–1295. discussion 1296-1297. PMID:
9848841.

4. Han MH, Kwon OK, Yoon CJ, Kwon BJ, Cha SH, Chang KH. Gas generation and clot formation during electrolytic detachment of Guglielmi detachable coils: in vitro observations and animal experiment. AJNR Am J Neuroradiol. 2003; 24:539–544. PMID:
12637312.
5. Hwang G, Park H, Bang JS, Jin SC, Kim BC, Oh CW, et al. Comparison of 2-year angiographic outcomes of stent- and nonstent-assisted coil embolization in unruptured aneurysms with an unfavorable configuration for coiling. AJNR Am J Neuroradiol. 2011; 32:1707–1710. PMID:
21852378.

6. Klötzsch C, Nahser HC, Henkes H, Kühne D, Berlit P. Detection of microemboli distal to cerebral aneurysms before and after therapeutic embolization. AJNR Am J Neuroradiol. 1998; 19:1315–1318. PMID:
9726475.
7. Koebbe CJ, Veznedaroglu E, Jabbour P, Rosenwasser RH. Endovascular management of intracranial aneurysms: current experience and future advances. Neurosurgery. 2006; 59(5 Suppl 3):S93–S102. discussion S3-S13. PMID:
17053622.

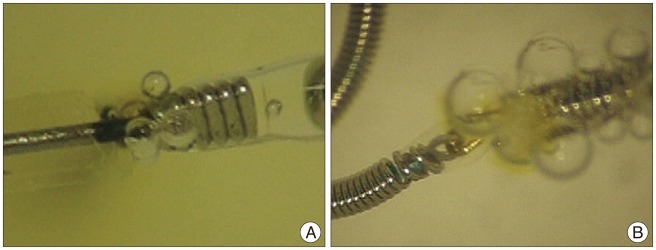
8. Lee DH, Hwang SM, Lim OK, Kim JK. In vitro observation of air bubbles during delivery of various detachable aneurysm embolization coils. Korean J Radiol. 2012; 13:412–416. PMID:
22778562.

9. Moret J, Cognard C, Weill A, Castaings L, Rey A. The "Remodelling Technique" in the Treatment of Wide Neck Intracranial Aneurysms. Angiographic Results and Clinical Follow-up in 56 Cases. Interv Neuroradiol. 1997; 3:21–35. PMID:
20678369.

10. Murayama Y, Nien YL, Duckwiler G, Gobin YP, Jahan R, Frazee J, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years' experience. J Neurosurg. 2003; 98:959–966. PMID:
12744354.

11. Murayama Y, Viñuela F, Duckwiler GR, Gobin YP, Guglielmi G. Embolization of incidental cerebral aneurysms by using the Guglielmi detachable coil system. J Neurosurg. 1999; 90:207–214. PMID:
9950490.

12. Nelson PK, Levy DI. Balloon-assisted coil embolization of wide-necked aneurysms of the internal carotid artery: medium-term angiographic and clinical follow-up in 22 patients. AJNR Am J Neuroradiol. 2001; 22:19–26. PMID:
11158882.
13. Padolecchia R, Guglielmi G, Puglioli M, Castagna M, Nardini V, Collavoli PL, et al. Role of electrothrombosis in aneurysm treatment with Guglielmi detachable coils: an in vitro scanning electron microscopic study. AJNR Am J Neuroradiol. 2001; 22:1757–1760. PMID:
11673174.
14. Pelz DM, Lownie SP, Fox AJ. Thromboembolic events associated with the treatment of cerebral aneurysms with Guglielmi detachable coils. AJNR Am J Neuroradiol. 1998; 19:1541–1547. PMID:
9763391.
15. Qureshi AI, Suri MF, Khan J, Kim SH, Fessler RD, Ringer AJ, et al. Endovascular treatment of intracranial aneurysms by using Guglielmi detachable coils in awake patients: safety and feasibility. J Neurosurg. 2001; 94:880–885. PMID:
11409514.

16. Rordorf G, Bellon RJ, Budzik RE Jr, Farkas J, Reinking GF, Pergolizzi RS, et al. Silent thromboembolic events associated with the treatment of unruptured cerebral aneurysms by use of Guglielmi detachable coils: prospective study applying diffusion-weighted imaging. AJNR Am J Neuroradiol. 2001; 22:5–10. PMID:
11158880.
17. Sakai H, Sakai N, Nakahara I, Shimozuru T, Higashi T, Takahashi JC, et al. Embolic Complications of Endovascular Surgery for Cerebrovascular Diseases. Evaluation with Diffusion-Weighted MR Imaging. Interv Neuroradiol. 2000; 6 Suppl 1:223–226. PMID:
20667253.

18. Soeda A, Sakai N, Sakai H, Iihara K, Yamada N, Imakita S, et al. Thromboembolic events associated with Guglielmi detachable coil embolization of asymptomatic cerebral aneurysms: evaluation of 66 consecutive cases with use of diffusion-weighted MR imaging. AJNR Am J Neuroradiol. 2003; 24:127–132. PMID:
12533341.
19. Viñuela F, Duckwiler G, Mawad M. Guglielmi detachable coil embolization of acute intracranial aneurysm: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg. 1997; 86:475–482. PMID:
9046305.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download