Abstract
Objective
This consecutive retrospective study was designed to analyze and to compare the efficacy and outcomes of anterior cervical discectomy and fusion (ACDF) using a fibular and femur allograft with anterior cervical plating.
Methods
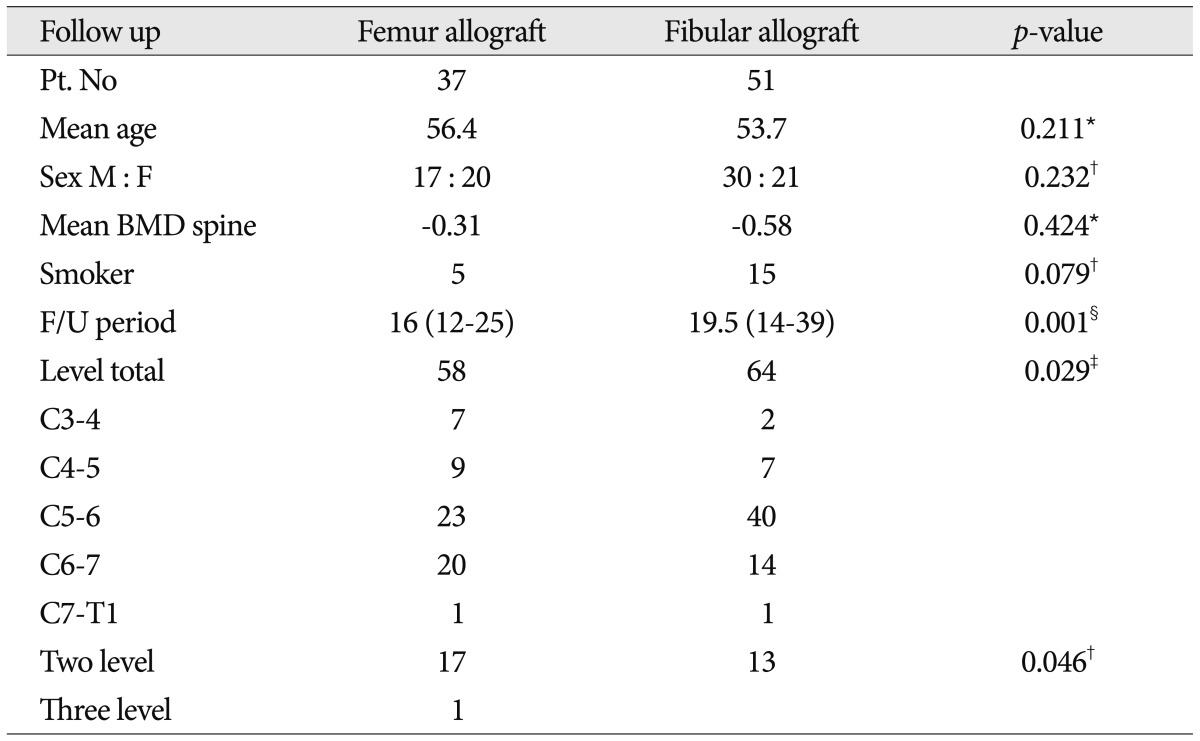
A total of 88 consecutive patients suffering from cervical degenerative disc disease (DDD) who were treated with ACDF from September 2007 to August 2010 were enrolled in this study. Thirty-seven patients (58 segments) underwent anterior interbody fusion with a femur allograft, and 51 patients (64 segments) were treated with a fibular allograft. The mean follow-up period was 16.0 (range, 12-25) months in the femur group and 19.5 (range, 14-39) months in the fibular group. Cage fracture and breakage, subsidence rate, fusion rate, segmental angle and height and disc height were assessed by using radiography. Clinical outcomes were assessed using a visual analog scale and neck disability index.
Results
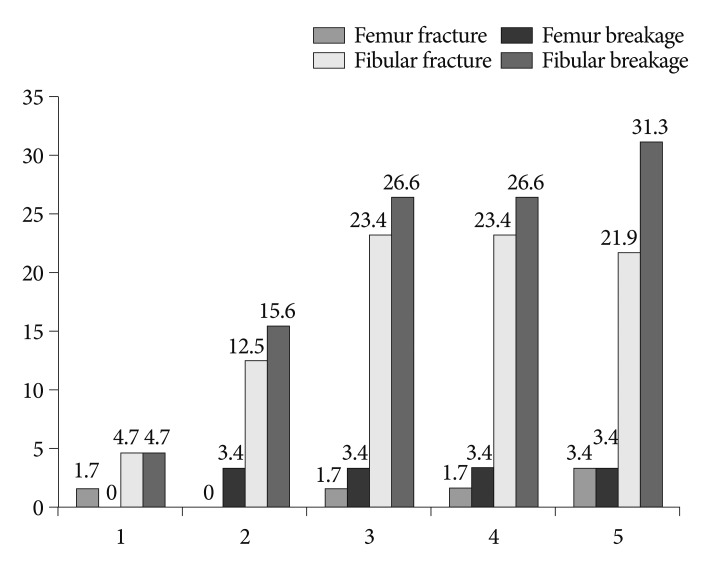
At 12 months postoperatively, cage fracture and breakage had occurred in 3.4% (2/58) and 7.4% (4/58) of the patients in the femur group, respectively, and 21.9% (14/64) and 31.3% (20/64) of the patients in the fibular group, respectively (p<0.05). Subsidence was noted in 43.1% (25/58) of the femur group and in 50.5% (32/64) of the fibular group. No difference in improvements in the clinical outcome between the two groups was observed.
Conclusion
The femur allograft showed good results in subsidence and radiologic parameters, and sustained the original cage shape more effectively than the fibular allograft. The present study suggests that the femur allograft may be a good choice as a fusion substitute for the treatment of cervical DDD.
Although anterior cervical discectomy and fusion (ACDF) was initially described in the 1950s, the ideal interbody graft material for use in this procedure remains to be identified. A tricortical iliac crest autograft is still considered by many to be the gold standard, but bone grafting is associated with a high rate of donor site morbidity and adds to the operative time. Therefore, allografts are commonly used to bridge bone defects after a discectomy. Fibular grafts are popular among spine surgeons for cervical fusions. Although cortical allografts are readily available and are reported to result in successful ACDF procedures14), a potential downside to their use is the prolonged time for remodeling and full incorporation27). Additionally, due to their significantly greater stiffness in comparison to the cervical endplate, they may promote subsidence, particularly if the endplate has been resected during surgery or in patients with decreased vertebral body bone density16).
Femur allografts are reported to possess more cortical thickness and compressive strength than rib and iliac crest allografts in biomechanical studies30). We hypothesized that femur material may reduce the likelihood of graft collapse and resorption before fusion as compared to fibular grafts. However, no clinical or biomechanical results have been reported on this subject. Although a previously published study on allografts reported various fusion rates with subsidence23), it did not show what types of allografts had superior fusion rates and less subsidence, breakage, and fracture. The purpose of this study was to analyze and compare the efficacy and outcomes of anterior cervical fusion using a fibular and femur allograft with the anterior cervical plating system in degenerative disc disease (DDD), using plain radiographs and computed tomography (CT) scan analysis to assess the results.
From September 2007 to August 2010, a total of 93 consecutive patients were enrolled in the study. The level of operation was between C3 and C7. All patients had suffered from degenerative cervical radiculopathy that was resistant to conservative treatment for at least 6 months and they had no history of prior cervical surgery. The patients underwent ACDF with allografts and the anterior plating system. We analyzed the clinical outcomes of the patients who underwent treatment with femur allograft cages (Ultra C1®; Tissuenet, FL, USA) (37 patients, 58 levels) or a fibular allograft (51 patients, 64 levels). No specific guidelines or indications were used in dividing the patients between the 2 groups. The demographic and clinical data were comparable in the 2 groups, though there was a statistical difference in the operation level and follow-up period (Table 1). In the femur allograft group, there were 17 men and 29 women, and the mean age was 56.4 years (range, 32-76 years). In the fibular allograft group, there were 30 men and 21 women, and the mean age was 53.7 years (range, 29-76 years). Cervical DDD was confirmed by cervical radiography, CT, and magnetic resonance imaging (MRI). The levels of segment fusion are shown in Table 1, and the most common cervical level involved was C5-6.
Operations in the 2 groups were performed by 2 surgeons and were consecutively investigated. All patients were treated using a standard Robinson and Smith's approach to the cervical spine. A simple lateral radiograph was used to determine the position of the skin incision, which was made transversely along a skin crease. The correct level was ensured using a second lateral radiograph, and a cervical blade with a self-retractor and a pin for longitudinal distraction was placed in the adjoining vertebral bodies. A microscope was used in most cases during the discectomy. In all cases, the posterior longitudinal ligament was opened transversely, and osteophytes that were possibly compressing the nerve root were removed with a 2 mm Kerrison punch and drill to obtain adequate exposure and decompression of the dura mater and nerve root origin. Endplates were cleaned and fashioned with curettes and a high-speed pneumatic drill, and we tried to preserve the endplate as much as possible to prevent cage subsidence. For femur allograft cage treatment, the cage size was determined by both preoperative templating and intraoperative evaluation using a trial cage for sizing to confirm the initial stability. For fibular allograft cage treatment, a pre-sized allograft was selected and impacted into place as the cage height was modified by a drill until the intraoperative evaluated height was achieved. For all patients in both groups, an adequate amount of dried cancellous allobone chip was prepared and placed into a pre-sized cage before impaction. The cage was inserted, and longitudinal distraction was slightly adjusted. After the cage was positioned and distraction was released, we confirmed that there was no minute movement of the cage using a ball probe. Regarding the anterior plating methods, four different types of plating systems were used in the study, but this factor was not included in the analysis. Before closing the superficial layers, a lateral radiograph was obtained, and the correct position of the implant and overdistraction was checked by comparison with the preoperative image. After surgery, patients with an uneventful recovery were discharged within a week. All patients were treated with the same protocol, consisting of immobilization with the Philadelphia cervical collar for 6 to 8 weeks.
Clinical outcome was assessed using visual analog scale (VAS) scoring for the neck and arm (0-10, with 0 reflecting no pain); functional outcomes were measured using the neck disability index (NDI) score. The NDI score is based on responses to 10 questions addressing pain intensity, personal care, lifting, reading, headache, concentration, working, driving, sleeping, and recreation. The resultant scores from 0% to 100% reflect the amount of disability (100% is maximum disability). The NDI score was used to compare the pre- and postoperative course; scores were collected before surgery and at three months, six months, nine months, and 1 year after surgery.
Radiological assessment was performed using radiography and CT. Radiographs were obtained before surgery and at 3 months, 6 months, 9 months, and 1 year after surgery, and at the last follow-up. Three-dimensional CT reconstruction was performed when evidence of bone fusion could be observed by radiography at approximately 3 to 6 months postoperatively. Fusion was considered as the presence of trabecular bone across the interface without lucencies between the cage and vertebral endplates, and bony bridging formation between the superior and inferior endplates. In 14 patients (5 in the femur group and 9 in the fibular group), CT evaluation was not permitted. Therefore, dynamic radiography was used to assess fusion, which was defined as less than a 2 mm difference in the interspinous distance between the flexion and extension dynamic radiographs.
An independent observer who was not in charge of the operations measured all radiographic parameters using a measuring program with a built-in picture-achieving communication system (PiView; INFINITT Co. Ltd., Seoul, Korea). The disc height, segmental height, and segmental angle were evaluated on the lateral view of each radiograph (Fig. 1). Disc height was measured as the mean value of the anterior and posterior disc height at the attempted fusion levels. Segmental height was measured as the length of the fusion segment from the midpoint of the upper endplate to the midpoint of the lower endplate. Segmental angle was measured by checking Cobb's angle between parallel lines from the upper endplate and the lower endplate at the fusion level.
We classified the cage condition according to cage shape (Fig. 2). Grade I was defined as an intact cage that sustained its original shape. Grade II was defined as a cage that had eroded either the upper or the lower endplate by less than 25% of the cage height. Grade III was defined as a cage that had caused both upper and lower endplate erosion of less than 50% of the cage height. Grade IV was defined as a cage that had sunk more than 50% of the cage height. We also investigated the fracture lines and breakage of the cage. We classified fracture lines as fractures that were visible on the cage, but showed no distraction or breakage. Cage breakage was defined as a broken cage that was distracted between the broken pieces.
The statistical significance of the differences between groups was tested by using the non-parametric Mann-Whitney U test and the chi-squared test. Continuous variables were compared using the t-test where applicable. Significance was set at 0.05. Values are given as mean±standard deviation. Statistical tests were performed with SPSS software (SPSS, Chicago, IL, USA).
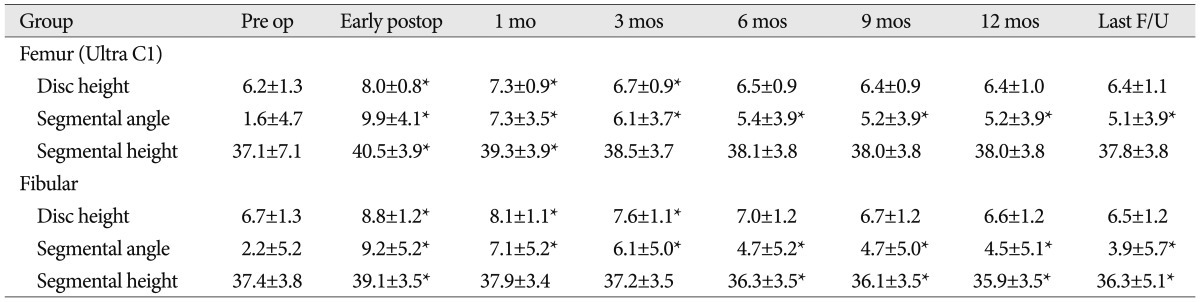
The results on disc space height, segmental angle, and segmental height are listed in Table 2. There was significant improvement in the disc space height in both groups during the first 3 postoperative months when compared with the preoperative state (p<0.05). At the last follow-up, the results show that some resorption and remodeling had occurred at the interspace level in both groups, and there was no significant difference between the groups. An intra-group comparison of the preoperative and early postoperative height showed no significant difference between the groups; this result indicates that the distraction force at the attempted fusion levels was adjusted equivalently in both groups.
There was significant improvement in the segmental angle between the preoperative and postoperative values in both groups, and there was no significant difference between the groups. After 6 months, the femur group had more sustained angulations than the fibular group.
The segmental height was increased by surgery in both groups (p<0.05). In the femur group, the postoperative value gradually decreased until 6 months, after which time, it showed a sustained tendency. In the fibular group, the 6-month postoperative values were lower than the preoperative values and continuously decreased until the last follow-up. Subsidence was defined as a difference of more than 3 mm between the preoperative and 6-month postoperative values; it was observed in 31.0% (18/58) of the patients in the femur group and 37.5% (24/64) of those in the fibular group. At 12 months postoperatively, subsidence was present in 43.1% (25/58) of patients in the femur group and in 50.5% (32/64) of those in the fibular group. Although there were no significant differences in these results, the femur allograft appeared to be superior to the fibular allograft with respect to subsidence.
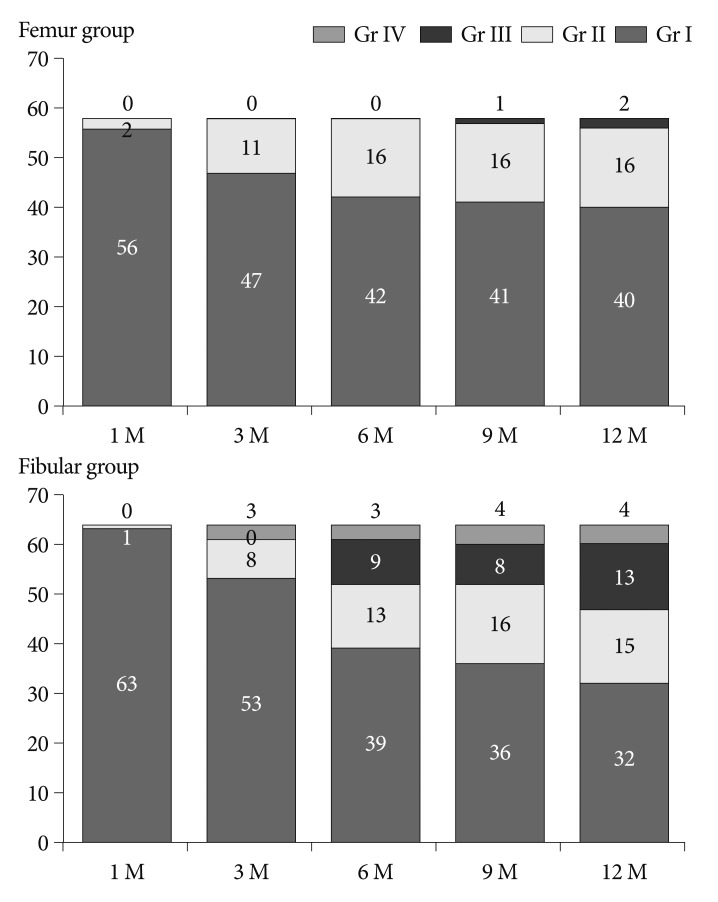
The cage condition results for both groups are presented in Fig. 3. In the femur group, there were 40 Grade I, 16 Grade II, and 2 Grade III cages at 12 months postoperatively. There were no Grade IV cages in the femur group. In the fibular group, there were 32 Grade I, 15 Grade II, 13 Grade III, and 4 Grade IV cages at 12 months postoperatively.
The cage fracture and breakage results are presented in Fig. 4. At the 12-month follow-up, there were only 2 fractures and 2 breakages in the femur allograft group. In contrast, there were 14 fractures and 20 breakages in the fibular group. Femur allografts sustained a better original cage shape than fibular allografts.
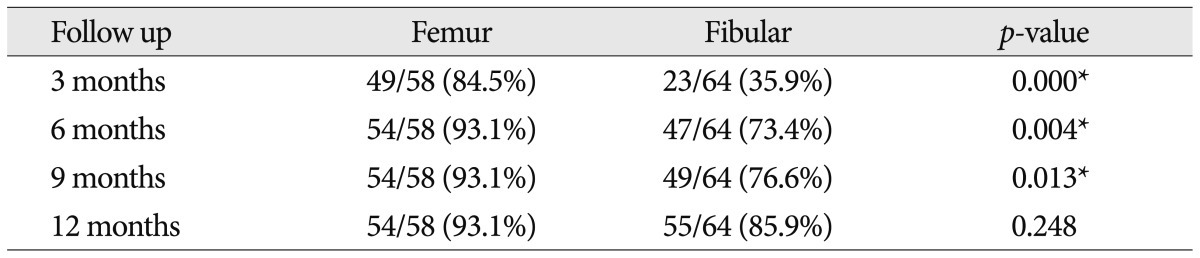
In the femur group, fusion was confirmed in 93% (54/58) of the patients at 6 months, and this result was consistent at 12 months. In the fibular group, fusion had occurred in 72.6% (47/64) of the patients at 6 months and 85.5% (55/64) of the patients at 12 months (Table 3). At 6 months postoperatively, there was a significant difference between the groups (p<0.05), but no difference was identified at 12 months postoperatively.
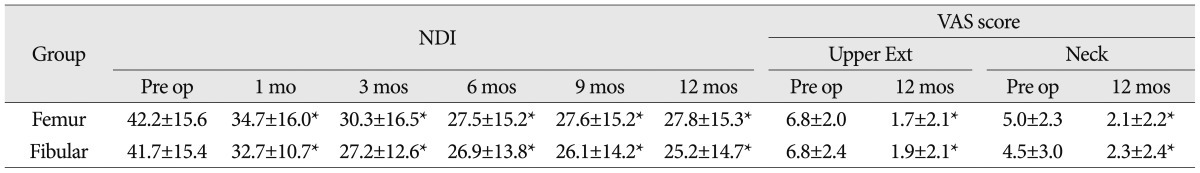
The clinical outcomes are summarized in Table 4. There was a significant reduction in the severity of neck and arm pain between the pre- and postoperative periods based on VAS scores in both groups (p<0.05). A significant increase in muscle strength was noted in patients in both groups according to the NDI score during the postoperative period (p<0.05). There was no significant difference between the 2 groups regarding reduction in postoperative pain and neurological recovery. All patients were discharged within 10 days. There were no immediate procedure-related complications in either group. During the follow-up period, 1 case of screw loosening and 1 case of cage migration was observed in the femur group. In the fibular group, there was 1 case of screw loosening and 2 cases of cage migration. These patients showed good clinical outcomes on follow-up, and no revision surgery was necessary.
Pseudarthrosis and graft collapse are the main issues that can occur after anterior cervical fusion. To decrease the incidence of these problems after surgery, several variables, including graft selection, fusion extenders or graft substitutes, and plate design, have been considered. In terms of graft selection, a higher fusion rate was reported with the use of autografts1,9,31). However, owing to the donor site morbidity of autografts, allografts have become more popular, although more time may be required to complete fusion4,10,17,31).
Many reports have concluded that a fibular allograft is an effective substrate for achieving fusion after an anterior discectomy14,18). However, this allograft cannot support the interspace height for long-term measurement because of graft slippage, subsidence, and compression5). Allografts and bone substitute have higher rates of non-union than autografts, and may be associated with a higher incidence of graft collapse1,2,9,18). Graft-related problems in the neck include collapse and extrusion, as well as failure of fusion due to pseudarthrosis31). Allograft subsidence and fracture likely stem from multiple causes, including osteoporosis, aggressive endplate preparation, excessive anterior distraction22), postoperative exogenous forces, and bracing3,9,20). Cage subsidence or migration has also been observed and results in disc height collapse and kyphotic deformity21). In addition to a high fusion rate, successful treatment depends on the maintenance of the interspace height and segmental angle15). Moreover, in the postoperative period, significant changes occur in the mechanical properties of both the graft and the endplate. Enneking et al.8) found that during the period of graft incorporation, vascular ingrowth is associated with a decrease in mechanical strength. Later, this strength returns8). These changes in the mechanical properties of the host and graft bone may also account for graft fracture or subsidence. In this study, we classified cage shape and compared the femur group and fibular group over a time course, as presented in Fig. 2. We placed importance on cage deformation as a cause of subsidence, and classified the common features of cage deformation. Our results show that compared to fibular allografts, femur allografts are superior in sustaining their original shape and show better results for subsidence, segmental angle, and disc height during the follow-up period.
During the analysis of bone quality in human long bones by CT, the cortical density was found to be similar between the femur and fibular shafts, but the bone strength index was higher in the femur shafts than in the fibular shafts26). In biomechanical studies, grafts from the distal tibia and femoral head were shown to be significantly stronger than those from the distal femur, proximal tibia, and humeral head, making them optimal allograft materials6). In addition, femur allografts possess greater cortical thickness and compressive strength than rib and iliac crest allografts30). A femoral ring allograft is one of the most commonly used materials in lumbar fusion because of its strength in compression and its osteoinductive and osteoconductive properties29). In addition to cervical fusion, there have been several reports on the successful implantation of femoral head allografts18).
Five prospective studies have compared allografts with autografts1,2,4,28,31). These studies encompassed 251 single-level fusions with a fusion rate of 94% for autografts and 85.3% for allografts. Suchomel et al.28) found a 94.6% fusion rate using autografts, compared with a rate of 85.5% for allografts at 1 year postoperatively. The authors showed progressive fusion rates for both allografts and autografts up to 1 year after surgery. Our results of an 85.9% fusion rate in the fibular group are similar to the previous prospective data on single-level fusions28).
However, our findings in the femur group indicate a much higher success rate for femur allografts than for fibular allografts. At the 1-year follow-up, the average change in the disc height was 2.6 mm, the change in the segmental angle was 4.7°, the change in the segmental height was 2.5 mm, and there was no significant difference in the average changes between this group of patients and the fibular group. The high fusion rate (93.1%) and clinical outcome scores of the patients in the femur group compare favorably with those in the fibular group. During follow-up, 3 patients presented with cage migration, and 2 patients presented with screw loosening. However, no patient required additional surgery during the follow-up period. In these cases, the amount of cage resorption was not different from the mean results, and as the patients had good postoperative NDI scores, the clinical outcome was unaffected.
Ann et al.7) used the degree of subsidence as a direct measurement of change in the intervertebral disc space height, and reported a subsidence rate of 19% at 12 months' follow-up. We defined subsidence as a difference of more than 3 mm between the immediate postoperative segmental angle and the follow-up segmental angle, as reported for synthetic interbody cages11), since subsidence is thought to be overestimated by the bone growth of the upper and lower endplates in the intervertebral disc space. In the femur group, the subsidence rate was 31.0% (18/58) at 6 months and 43.1% (25/58) at 12 months. In the fibular group, subsidence was 37.5% (24/64) at 6 months and 50.5% (32/64) at 12 months. These results suggest that femur allografts were superior to fibular allografts in preventing subsidence, although there was no significant difference in this result.
The femur allograft used in the current study was collected from human cadaveric donors and prepared in a precision tooled cortical cervical spacer7). This allograft was then processed and preserved via freeze-drying or freezing for 2 years13). No irradiation was used in the sterilization process. Our results in the femur group, especially the resistance to postoperative disc and segmental height loss and increased kyphosis, suggest an improvement in the quality of this graft over previous grafts. It contains tooth-like protrusions on the superior and inferior surfaces that aid in resisting retropulsion. It also has a lordotic angle from anterior to posterior of about 5 degrees. This design may help to keep the femur allograft intact for a longer period, thus prolonging its life as a mechanical device before it is finally incorporated into the surrounding bone during the fusion process.
Our clinical results showed significant improvement in patient pain and disability when compared with the preoperative condition. Neck and arm pain scores were most significantly improved, but they are less statistically reliable as an outcome measure than the NDI scores. Our NDI results were similar to the results from other reports on fusion using allografts19). The NDI scores were statistically improved after 1 month in each group and also improved over time, with the improvement stabilizing after 6 months in both groups. The 12-month postoperative NDI scores for the 2 groups were nearly identical (27.8 in the femur group and 25.2 in the fibular group), indicating that a good clinical outcome was achieved with both types of interbody grafts. The overall performance of the femur allograft appears to be comparable with that of the fibular allograft.
An anterior cervical plate can increase the immediate postoperative stability and thus enhance fusion. It also decreases the extent of graft collapse and subsidence, preventing postoperative kyphosis formation24,25). Although clinical outcomes and fusion rates are similar in patients with fixed-hole or slotted hole dynamic plates, the use of a fixed-hole dynamic plate is more favorable with regard to graft subsidence and implant translation in the follow-up period12). In this study, although all patients underwent anterior plating, the results based on plating were not included in our investigation because different types of plates were used. This is a limitation of the current study.
References
1. An HS, Simpson JM, Glover JM, Stephany J. Comparison between allograft plus demineralized bone matrix versus autograft in anterior cervical fusion. A prospective multicenter study. Spine (Phila Pa 1976). 1995; 20:2211–2216. PMID: 8545714.

2. Bishop RC, Moore KA, Hadley MN. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate : a prospective comparative analysis. J Neurosurg. 1996; 85:206–210. PMID: 8755747.

3. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993; 75:1298–1307. PMID: 8408151.

4. Brown MD, Malinin TI, Davis PB. A roentgenographic evaluation of frozen allografts versus autografts in anterior cervical spine fusions. Clin Orthop Relat Res. 1976; 231–236. PMID: 782759.

5. Celik SE, Kara A, Celik S. A comparison of changes over time in cervical foraminal height after tricortical iliac graft or polyetheretherketone cage placement following anterior discectomy. J Neurosurg Spine. 2007; 6:10–16. PMID: 17233285.

6. Chen D, Kummer FJ, Spivak JM. Optimal selection and preparation of fresh frozen corticocancellous allografts for anterior interbody lumbar spinal fusion. J Spinal Disord. 1997; 10:532–536. PMID: 9438821.

7. Ehrler DM, Vaccaro AR. The use of allograft bone in lumbar spine surgery. Clin Orthop Relat Res. 2000; 371:38–45. PMID: 10693548.

8. Enneking WF, Burchardt H, Puhl JJ, Piotrowski G. Physical and biological aspects of repair in dog cortical-bone transplants. J Bone Joint Surg Am. 1975; 57:237–252. PMID: 1089671.

9. Fernyhough JC, White JI, LaRocca H. Fusion rates in multilevel cervical spondylosis comparing allograft fibula with autograft fibula in 126 patients. Spine (Phila Pa 1976). 1991; 16:S561–S564. PMID: 1801273.

10. Goldberg VM, Stevenson S. Natural history of autografts and allografts. Clin Orthop Relat Res. 1987; 7–16. PMID: 3315383.

11. Ha SK, Park JY, Kim SH, Lim DJ, Kim SD, Lee SK. Radiologic Assessment of Subsidence in Stand-Alone Cervical Polyetheretherketone (PEEK) Cage. J Korean Neurosurg Soc. 2008; 44:370–374. PMID: 19137081.

12. Hong SW, Lee SH, Khoo LT, Yoon SH, Holly LT, Shamie AN, et al. A comparison of fixed-hole and slotted-hole dynamic plates for anterior cervical discectomy and fusion. J Spinal Disord Tech. 2010; 23:22–26. PMID: 20051923.

13. Jinno T, Miric A, Feighan J, Kirk SK, Davy DT, Stevenson S. The effects of processing and low dose irradiation on cortical bone grafts. Clin Orthop Relat Res. 2000; 275–285. PMID: 10853179.

14. Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002; 50:229–236. discussion 236-238. PMID: 11844257.

15. Kao FC, Niu CC, Chen LH, Lai PL, Chen WJ. Maintenance of interbody space in one- and two-level anterior cervical interbody fusion : comparison of the effectiveness of autograft, allograft, and cage. Clin Orthop Relat Res. 2005; 108–116. PMID: 15662311.
16. Lim TH, Kwon H, Jeon CH, Kim JG, Sokolowski M, Natarajan R, et al. Effect of endplate conditions and bone mineral density on the compressive strength of the graft-endplate interface in anterior cervical spine fusion. Spine (Phila Pa 1976). 2001; 26:951–956. PMID: 11317120.

17. Malloy KM, Hilibrand AS. Autograft versus allograft in degenerative cervical disease. Clin Orthop Relat Res. 2002; 27–38. PMID: 11795743.

18. Martin GJ Jr, Haid RW Jr, MacMillan M, Rodts GE Jr, Berkman R. Anterior cervical discectomy with freeze-dried fibula allograft. Overview of 317 cases and literature review. Spine (Phila Pa 1976). 1999; 24:852–858. discussion 858-859. PMID: 10327505.
19. Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion : a randomized controlled clinical trial. J Neurosurg Spine. 2007; 6:198–209. PMID: 17355018.

20. Natarajan RN, Chen BH, An HS, Andersson GB. Anterior cervical fusion : a finite element model study on motion segment stability including the effect of osteoporosis. Spine (Phila Pa 1976). 2000; 25:955–961. PMID: 10767808.
21. Niu CC, Chen LH, Lai PL, Fu TS, Chen WJ. Trapezoidal titanium cage in anterior cervical interbody fusion : a clinical experience. Chang Gung Med J. 2005; 28:212–221. PMID: 16013340.
22. Olsewski JM, Garvey TA, Schendel MJ. Biomechanical analysis of facet and graft loading in a Smith-Robinson type cervical spine model. Spine (Phila Pa 1976). 1994; 19:2540–2544. PMID: 7855678.

23. Ryken TC, Heary RF, Matz PG, Anderson PA, Groff MW, Holly LT, et al. Techniques for cervical interbody grafting. J Neurosurg Spine. 2009; 11:203–220. PMID: 19769500.

24. Ryu SI, Mitchell M, Kim DH. A prospective randomized study comparing a cervical carbon fiber cage to the Smith-Robinson technique with allograft and plating : up to 24 months follow-up. Eur Spine J. 2006; 15:157–164. PMID: 15980998.

25. Savolainen S, Rinne J, Hernesniemi J. A prospective randomized study of anterior single-level cervical disc operations with long-term follow-up : surgical fusion is unnecessary. Neurosurgery. 1998; 43:51–55. PMID: 9657188.

26. Sievänen H, Koskue V, Rauhio A, Kannus P, Heinonen A, Vuori I. Peripheral quantitative computed tomography in human long bones : evaluation of in vitro and in vivo precision. J Bone Miner Res. 1998; 13:871–882. PMID: 9610752.

27. Stevenson S, Emery SE, Goldberg VM. Factors affecting bone graft incorporation. Clin Orthop Relat Res. 1996; 66–74. PMID: 8595779.

28. Suchomel P, Barsa P, Buchvald P, Svobodnik A, Vanickova E. Autologous versus allogenic bone grafts in instrumented anterior cervical discectomy and fusion : a prospective study with respect to bone union pattern. Eur Spine J. 2004; 13:510–515. PMID: 15042453.

29. Thalgott JS, Fogarty ME, Giuffre JM, Christenson SD, Epstein AK, Aprill C. A prospective, randomized, blinded, single-site study to evaluate the clinical and radiographic differences between frozen and freeze-dried allograft when used as part of a circumferential anterior lumbar interbody fusion procedure. Spine (Phila Pa 1976). 2009; 34:1251–1256. PMID: 19412139.

30. Wittenberg RH, Moeller J, Shea M, White AA 3rd, Hayes WC. Compressive strength of autologous and allogenous bone grafts for thoracolumbar and cervical spine fusion. Spine (Phila Pa 1976). 1990; 15:1073–1078. PMID: 2263975.

31. Zdeblick TA, Ducker TB. The use of freeze-dried allograft bone for anterior cervical fusions. Spine (Phila Pa 1976). 1991; 16:726–729. PMID: 1925745.

Fig. 1
This diagram shows how disc height, segmental height and angle were determined in this study.
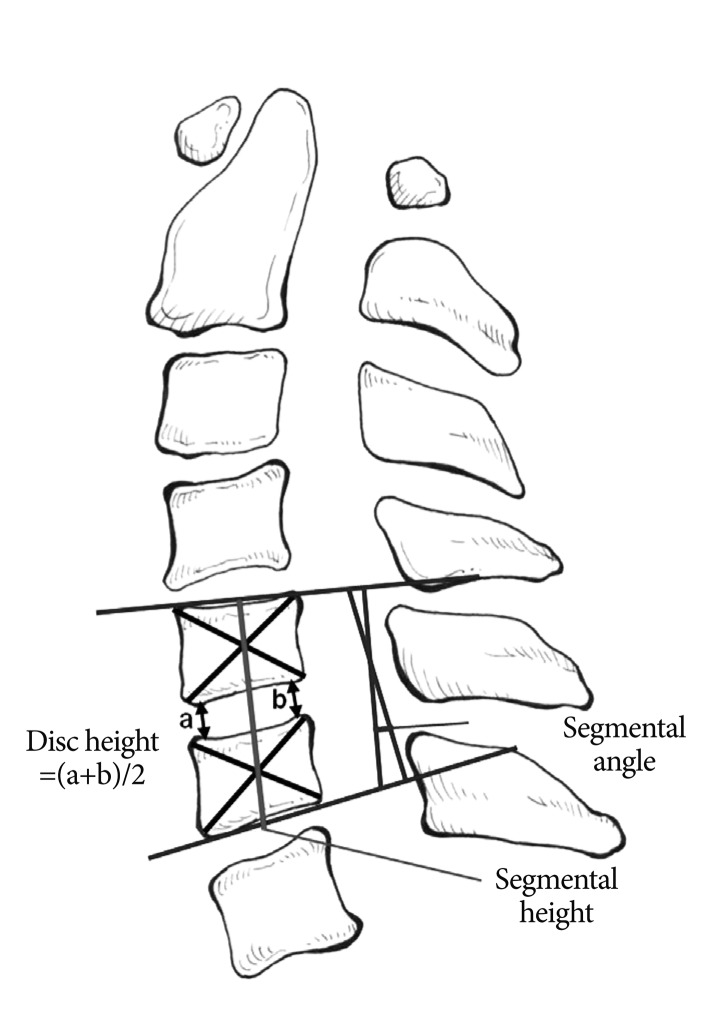
Fig. 2
Classification of cage condition and the definition of cage breakage and fracture line of cage.
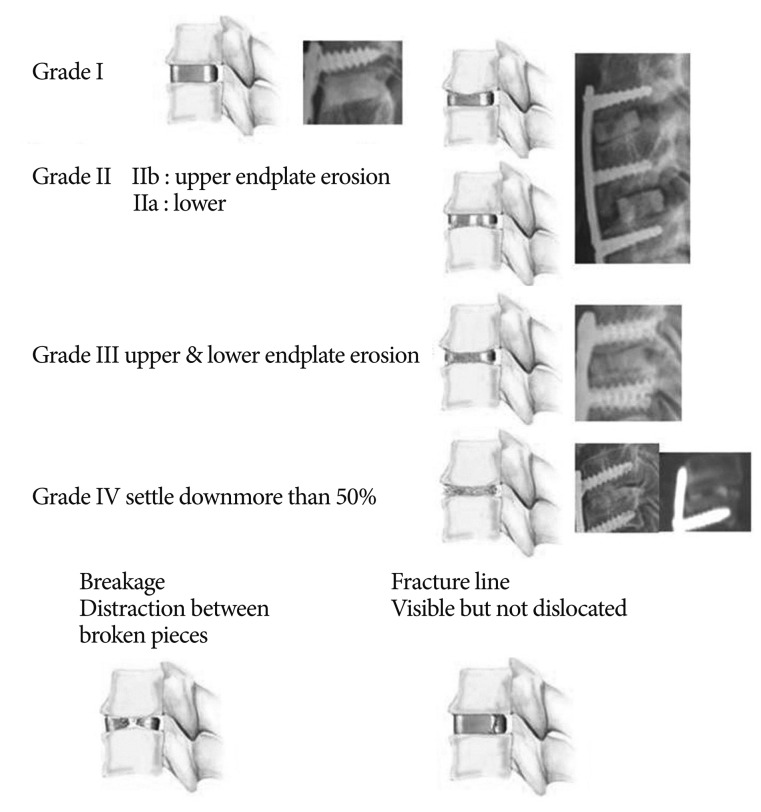
Table 2
Summary of disc height, segmental angle, segmental height measurements in femur and fibular group




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download