Abstract
Perforation of the hypopharynx, which can occur after anterior cervical approach, is a very rare type of complication. If diagnosed late, it can lead to very fatal course, such as mediastinitis and hematosepsis. Therefore, a precise and prompt diagnosis is crucial. When conservative treatment alone is not expected to heal the perforated site or is likely to lead to serious complications, surgical treatment becomes necessary. This report demonstrates that surgical intervention performed immediately after an early diagnosis can lead to the successful treatment of a large perforation in the hypopharynx on a 58-year-old male patient.
Anterior cervical approach is an increasingly prevalent type of cervical surgery. However, it may cause unexpected complications during or after surgery, the most common of which include temporary dysphagia, hematoma, and hoarseness due to the injury of recurrent laryngeal nerve7). In rare cases, perforation may occur in the esophagus or hypopharynx3). The authors experienced a case of a large perforation in the hypopharynx that occurred after an anterior cervical discectomy in a patient transferred to our institute with major complaints of slight fever and subcutaneous emphysema. To avoid a catastrophic complication, surgical intervention was undertaken and achieved a successful outcome. Here, we report a case of large perforation of hypopharynx with a review of relevant literature, then we discuss the imaging and clinical features of this rare complicated case.
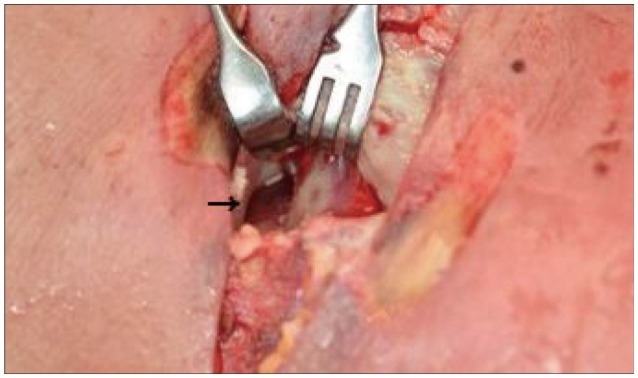
A 58-year-old male transferred to our emergency room (ER) complaining of painful swelling in the anterior cervical region. The patient underwent C3-4 discectomy and total disc replacement 3 days ago with the diagnosis of C3-4 disc herniation in local spine clinic. A physical examination identified painful edema in the surgical site of the anterior cervical region and necrotic skin tissue. Other findings included subcutaneous emphysema with crepitus in the area of the surgical site. His body temperature was 37.2℃ when he was transferred to ER. A hematological analysis demonstrated that his leukocyte count was 9670/mL, with an erythrocyte sedimentation tare of 70 mm/hr and a C-reactive protein of 19.9 mg/dL. Subcutaneous and mediastinal emphysema were identified by cervical computed tomography scans (Fig. 1). An esophagogram with gastrografin showed that a large amount of contrast medium had leaked into the right lateral cervical region (Fig. 2). Based on these findings, the patient was diagnosed with a perforation in the hypopharynx following the anterior cervical discectomy. As a result, an emergency surgery was performed to repair the perforation under general anesthesia. The operative findings included extensive soft tissue necrosis and abscess formation, both of which were removed and cultured. The perforated site was approximately 2 cm long and was found outside the pyriform sinus in the right hypopharynx (Fig. 3). The mucous membrane was sutured with Vicryl 3-0 in two layers from the outside. There was an attempt to reinforce the perforated part with the surrounding muscle, but severe inflammation prevented its use. Consequently, Tissel® was spread on the surgical site before the tube was inserted for drainage. On the 10th day after the operation, the drainage tube was removed. An esophagogram conducted on the 13th day after the operation showed no contrast leakage (Fig. 4). A liquid diet was permitted 15 days after the operation. Thereafter, the patient was transferred to the plastic surgery department of our institute to receive skin graft. A full-thickness skin graft was performed before the patient was discharged from the hospital. The patient was monitored for six months after the operation and showed no sign of complications.
Although anterior approaches to the cervical spine are popular and safe, they are not free of complications7). Dysphagia is one of the most common complications that occur after anterior cervical approach. Other complications include hematoma, vocal cord paralysis due to damage of the recurrent laryngeal nerve, leakage of cerebrospinal fluid, and perforation of the esophagus or hypopharynx. Among these complications, the incidence of esophageal perforation is low and it has been reported to be approximately 0.3%; the rate of hypopharynx perforation is much lower than that of esophageal perforation3). The symptoms of hypopharynx perforation include hemorrhage, pain, dysphagia, and subcutaneous emphysema. Among these symptoms, the common initial symptom is subcutaneous emphysema with crepitus upon cervical palpation. As the symptom develops, it can lead to cellulitis of the soft tissue due to inflammation, edema of the cervical region, fever, and hematosepsis5,6). In this case, the patient did not have a conspicuous fever but had painful swelling in the anterior cervical region as well as cellulitis and necrosis in the surrounding soft tissue. In addition, other findings included subcutaneous emphysema and pneumomediastinum in the cervical region. If hypopharynx perforation is diagnosed late, it is likely to cause fatal complications, such as retropharyngeal abscess, mediastinitis, hematosepsis, and meningitis, which may lead to death4,8). To diagnose perforation of hypopharynx at an early stage, it is critical to examine the medical history and conduct a careful physical examination. Cervical and chest radiographs enable the detection of subcutaneous emphysema, pneumomediastinum and pneumothorax, and cervical or chest CT scans enable the detection of a cervical abscess. The esophagogram which uses the water soluble contrast medium, gastrografin and CT may also determine the accurate location and degree of damage, including whether it has spread to the mediastinum, based on an air-biliarygram. Therefore, such methods are essential for determining the appropriate surgical treatment and access route2,11). If clinical suspicion remains, the use of barium, which is more sensitive, is suggested instead of a water-soluble contrast medium1). This case also showed that it was possible to make a precise diagnosis using CT and an esophagogram with gastrografin after examining the medical history and conducting a physical examination. Because the perforation was large, it was conspicuous enough to avoid the use of barium. Conservative treatment may be effective when the perforation less than 2 cm, the damage is limited to the pharynx without spreading to the cervical esophagus, the cervical abscess is not found, or there are no general symptoms of mediastinitis or hematosepsis. The conservative treatment for perforation requires the extensive administration of intravenous antibiotics and strict restriction of oral diet. The treatment also requires feeding through a nasogastric tube9). When a perforation is diagnosed early and its size is considered large, emergent repair is essential. In addition, surgical intervention is also necessary when contrast medium has leaked into the mediastinum or the pleural cavity, leading to the symptoms of pneumothorax and hematosepsis5). As soon as the patient, in this case, transferred the ER, cervical CT and esophagogram with gastrografin were performed to confirm the perforation of hypopharynx. Due to the suspicion of inflammation and abscess formation at the surgical site, the patient underwent exploration and drainage, and the primary suture was performed without implant removal. As shown in this study, primary suture can be sufficient for healing the damage to the hypopharynx. However, if the damage is more large, pedicled sternocleidomastoid muscle flap interposition may be required to reinforce the sutured site10). In this case, oral food intake after the cervical discectomy resulted in a leakage of the ingested food into the surrounding tissues. This leakage aggravated inflammation of the tissue and abscess formation, which led to severe necrosis of the surrounding region. As a result, it was impossible to use the muscle for reinforcement. However, the irrigation and complete removal of the necrotic tissues were performed without muscle reinforcement. After anterior cervical discectomy, a diagnosis of perforation of hypopharynx must be precise and prompt if conservative treatments are unlikely to suffice or if serious complications, such as mediastinitis or hematosepsis, are likely to arise. Immediate surgical intervention may be required.
References
1. Buecker A, Wein BB, Neuerburg JM, Guenther RW. Esophageal perforation : comparison of use of aqueous and barium-containing contrast media. Radiology. 1997; 202:683–686. PMID: 9051016.

2. Endicott JN, Molony TB, Campbell G, Bartels LJ. Esophageal perforations : the role of computerized tomography in diagnosis and management decisions. Laryngoscope. 1986; 96:751–757. PMID: 3724326.
3. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007; 32:2310–2317. PMID: 17906571.

4. Heater DW, Haskvitz L. Suspected pharyngoesophageal perforation after a difficult intubation : a case report. AANA J. 2005; 73:185–187. PMID: 16010770.
5. Hinojar AG, Díaz Díaz MA, Pun YW, Hinojar AA. Management of hypopharyngeal and cervical oesophageal perforations. Auris Nasus Larynx. 2003; 30:175–182. PMID: 12753990.

6. Kras JF, Marchmont-Robinson H. Pharyngeal perforation during intubation in a patient with Crohn's disease. J Oral Maxillofac Surg. 1989; 47:405–407. PMID: 2926551.

7. Lee JS, Kang DH, Hwang SH, Han JW. Oral extrusion of screw after anterior cervical interbody fusion. J Korean Neurosurg Soc. 2008; 44:259–261. PMID: 19096688.

8. Lee TS, Jordan JS. Pyriform sinus perforation secondary to traumatic intubation in a difficult airway patient. J Clin Anesth. 1994; 6:152–155. PMID: 8204237.

9. Niezgoda JA, McMenamin P, Graeber GM. Pharyngoesophageal perforation after blunt neck trauma. Ann Thorac Surg. 1990; 50:615–617. PMID: 2222052.

10. Orlando ER, Caroli E, Ferrante L. Management of the cervical esophagus and hypofarinx perforations complicating anterior cervical spine surgery. Spine (Phila Pa 1976). 2003; 28:E290–E295. PMID: 12897507.

11. Shockley WW, Tate JL, Stucker FJ. Management of perforations of the hypopharynx and cervical esophagus. Laryngoscope. 1985; 95:939–941. PMID: 4021688.

Fig. 1
Preoperative computed tomography scans show a large amount of subcutaneous emphysema in the anterior lateral cervical regions.

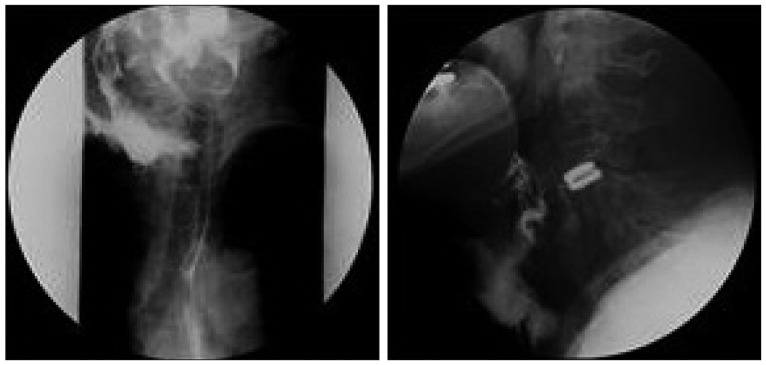
Fig. 2
Contrast study reveal a large fistulous tract and contrast leaking from the right pyriform sinus into the operation site.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download