Abstract
Objective
We performed a retrospective analysis of medical records and radiographic images of patients who never underwent spinal treatment including diagnosis. The objective of this study is to explain the biomechanical and physiologic characteristics of cervical alignment related to thoracic inlet angle including T1 slope changes in each individual.
Methods
We reviewed the cervical CT radiographs of 80 patients who visited ENT outpatient clinic without any symptom, diagnosis and treatment of cervical spine from January 2011 to September 2012. All targeted people were randomized without any prejudice. We assessed the data-T1 slope, Cobb's angle C2-7, neck tilt, sagittal vertical axis (SVA) C2-7 and thoracic inlet angle by the CT radiographs.
The sagittal balance of whole spine is affected critically in the clinical healthy state and optical biomechanical motion6). Each regional spine level keeps balance against the global axis of gravity with spinal curvature7). Imbalance of the spine in the sagittal plane is an important factor for clinical symptoms, degenerative disease and perioperative care4).
In the spinal regional division, the strong correlation of pelvic incidence and lumbar lordosis has been noted in several studies9). The relations have been used to extrapolate from clinical symptoms to operative predisposing factors. This spinopelvic balance as regional component of whole spine is already known as unique and proven1,12).
Sagittal balance in cervical spine is as important as pelvic incidence and related with the concept of T1 slope. The T1 slope is a landmark of an overall spinal sagittal balance and is a critical issue as the relationship between pelvic incidence and lumbar lordosis5,8). The sagittal balance of cervical spine must be affected by the shape and orientation of T1 slope value for keeping upright and horizontal plane. But, the normal cervical sagittal balance and physiological cervical lordosis is not clearly defined yet8). The T1 slope is a newly studied concept but it has a significant role in cervical sagittal alignment. Even in research that studied thoracic inlet angle and 1st thoracic spine, T1 slope checked by upright plain X-ray of cervical spine could not be exactly enough examined due to the anatomical interference limitation of shoulder contour density especially in obese people with thick thoracic trunk. Most research collected data by the T1 slope of unclear visible X-ray radiographs5,8).
To overcome the fundamental limitation of the X-ray radiographs, we studied the cervical sagittal balance by T1 slope and thoracic inlet angle with the more radical measurement with cervical 3 dimensional CT radiographs of asymptomatic persons. The evaluated values at supine with cervical 3D CT position were clearly exact because of no invisible limitation.
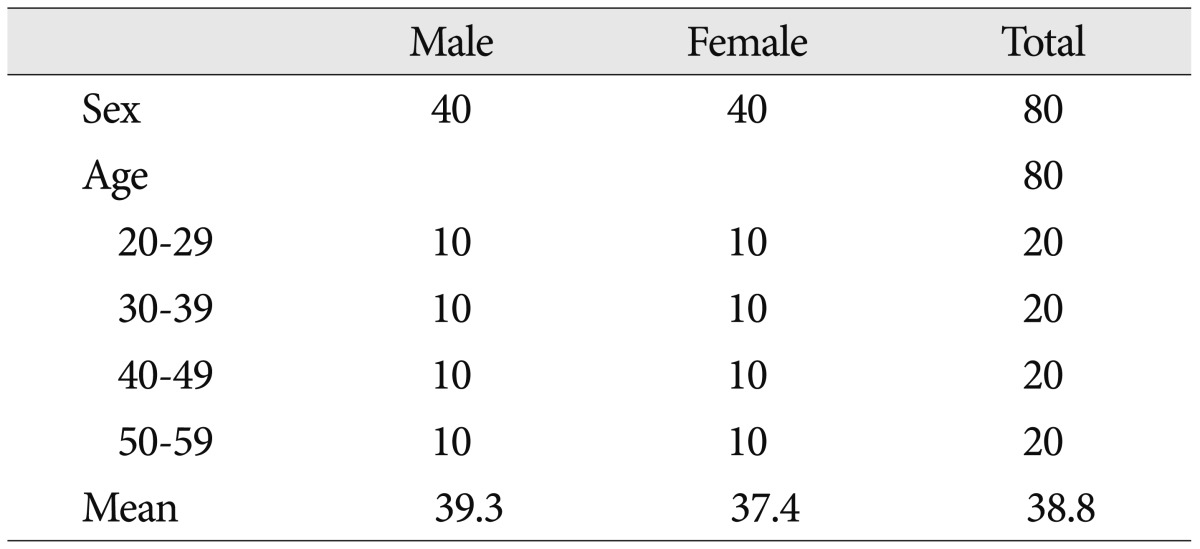
Asymptomatic 80 adults from 3rd decade to 6th decade who never had been treatment or diagnosis involved spinal problem were enrolled. The male to female ratio is equally 40 : 40, the mean age is 38.8 with a range of 30 to 59 year-old (Table 1). Cervical CT radiographs (Brilliance CT 64-channel scanner, Philips Electronics) checked from January 2011 to October 2012 were obtained with natural supine position with gaze on ceiling vertically without any uncomfortable involved factor10).
T1 slope, neck tilt, thoracic inlet angle, Cobb's angle C2-7 and sagittal vertical axis (SVA) C2-7 were measured by cervical CT radiographs data (Fig. 1)5,8). The T1 slope was measured as the angle between a horizontal line and the superior end plate of T1.
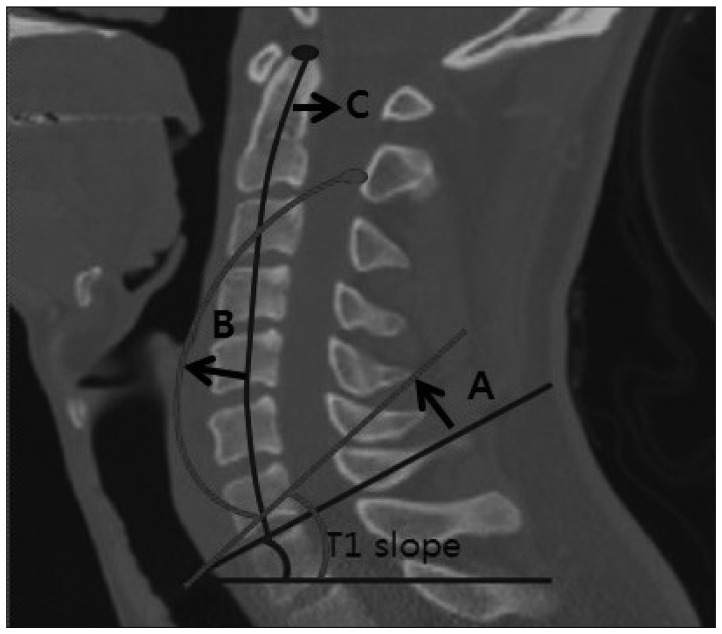
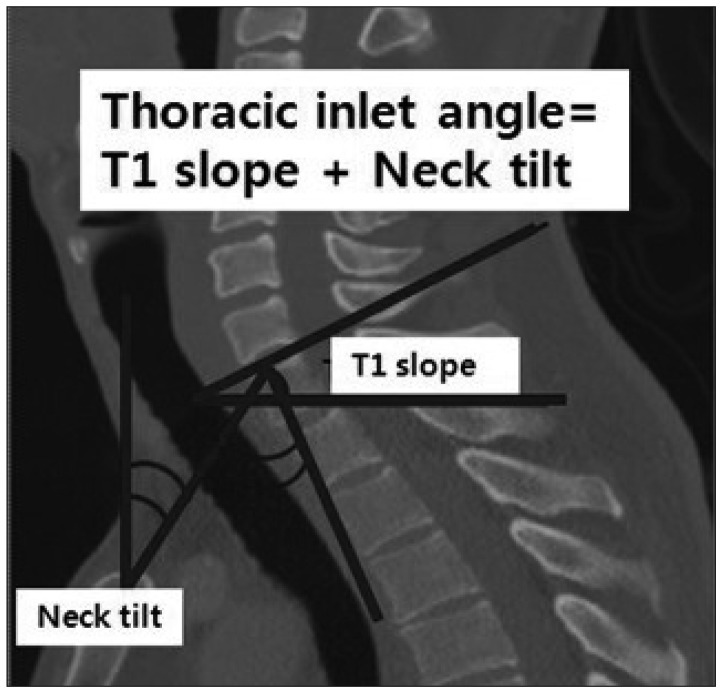
And, the neck tilt was defined as an angle formed by a vertical line of sternum tip and the line drawn in the center of upper end plate of the sternum connecting the center of the T1 upper end plate. The thoracic inlet angle (TIA) is a sum of T1 slope and neck tilt (Fig. 2). It was formed similar to relationship that pelvic incidence is the sum of sacral slope and pelvic tilting8,14). The distance between C2 vertical line and C7 vertical line constitutes the SVA C2-7.
In addition, Cobb's angle C2-7 was measured by formal Cobb methods that checked angle between the horizontal line of C2 lower end plate and the horizontal line of C7 lower end plate11,13). The radiographs were measured using standard techniques recommended by the Scoliosis Research Society.
The PACS system (p view, INFINITT , Seoul, Korea) was determined by 2 independent observers for the measurement. After the agreement between the observers, the each factor was measured twice independently by 2 spinal surgeons of neurosurgery department and the linear correlation coefficient was analyzed. The correlations between the parameters were analyzed with the Pearson correlation coefficient. For statistical analysis, the SPSS 19.0 (SPSS Inc., Chicago, IL, USA) was used and the p value <0.05 were considered significant.
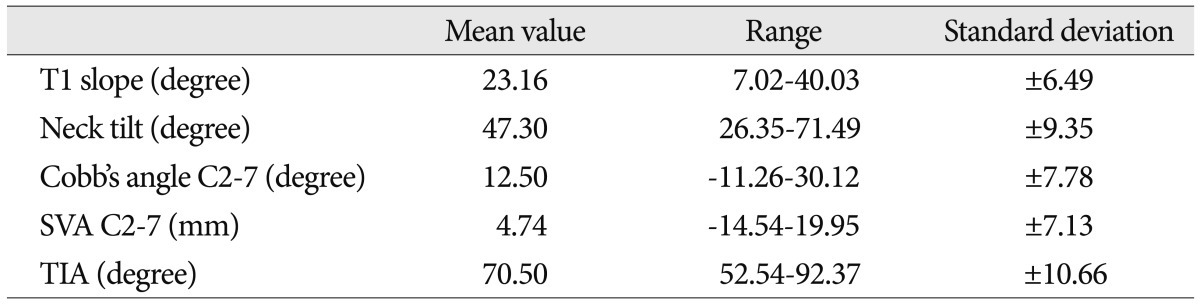
Before starting our study, we evaluated the possibility of checking T1 slope using cervical X-ray. It's difficult to estimate perfectly the randomized radiographs of the sternum and T1 vertebral body of 200 persons in our Spinal Center outpatient clinic from January 2011 to September 2012. We could check above the parameters from only 11% of 200 patients using cervical X-ray scans. In our patients' demographic data, the mean age was 38.79 (range 20 to 59, SD±11.47). The mean T1 slope was 23.20 (range 7.02 to 40.03, SD±6.49) and the mean neck tilt was 47.30 (range 26.35 to 71.49, SD±9.35). Also the mean TIA was 70.50 (range 52.54 to 92.37, SD±10.66) (Table 1).
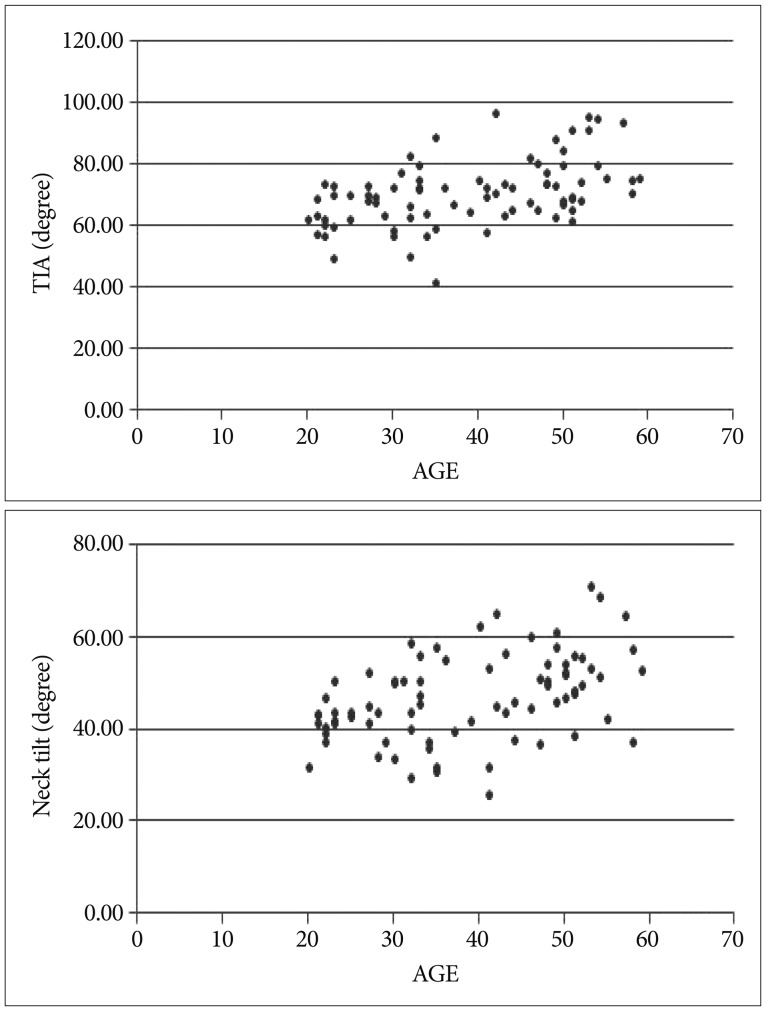
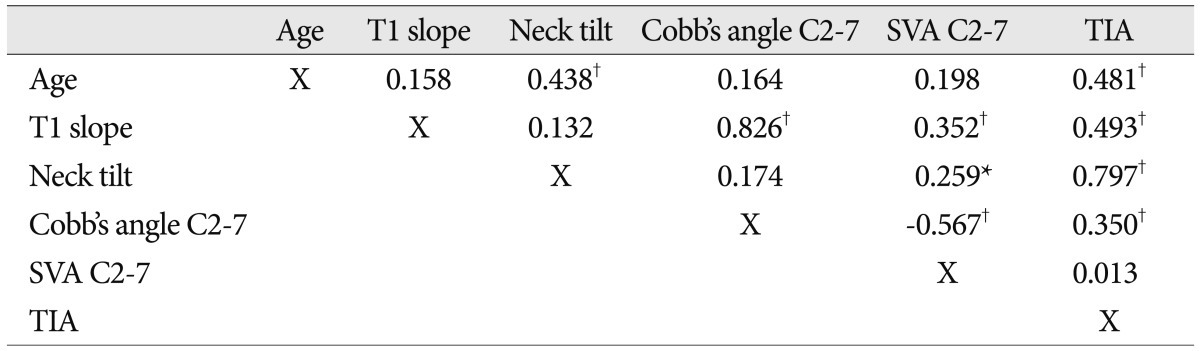
As the age was getting higher, the value of neck tilt and TIA had been increasing significantly with each Pearson correlation coefficient 0.44, 0.48 (p value <0.05) (Fig. 3).
The mean Cobb's angle C2-7 was 12.60 (range -11.26 to 28.80, SD±7.78). And the mean SVA C2-7 was 4.74 (range -14.54 to 19.95, SD±7.13) (Table 2). And, it shows the correlation factors between each value (Table 3).
The correlation coefficient for T1 slope and C2-7 Cobb's angle was found to be 0.83 (p value <0.05). T1 slope and SVA C2-7 also was -0.35 (p value <0.05). And, it was significantly correlated with TIA (0.49, p value <0.05). The TIA value is the sum of T1 slope angle and neck tilt angle. The correlation coefficient for C2-7 Cobb's angle and SVA C2-7 was found to be -0.57 (p value <0.05).
As known, the most optimal sagittal alignment of whole spine in each motion is keeping each component in proper balance. The global balance from the occiput to pelvis and regional balanced alignment is maintained in each curvature keeping optimal balance6). If this balance is broken, clinical symptoms related to unbalanced alignment arise. It is a critical factor of pre- and post-operative care4).
Many articles based on unclear cervical X-ray radiographs could weakly explain the T1 slope, neck tilt and TIA because of the invisible sternum tip contour in data targeted patients5,8). This means it is difficult to justify the relationship between the T1 slope and cervical lordosis. Therefore, we excluded the basic limitation of unclear parameters by using more accurate cervical CT 3 dimensional database of asymptomatic patients in ENT clinic without spinal disease or even neck pain.
There is a study about cervical alignment parameter and aging3). This article explains the association of increasing age with significant increases in neck tilt and TIA value. The superior end plate of T1 midpoint as a check point of neck tilt and T1 slope was affected by whole spine vertebral body and disc height loss due to the degenerative change. The relative angle value was larger in young age2).
The values of Cobb's angle C2-7 increase as the value of T1 slope rises. This was same as the previous study. The T1 slope as the axial base for cervical alignment was statistically significant. When T1 slope was increasing, the head center of gravity moved its position forward with anterior translation. Its overloading was compensated by reinforcing the cervical lordotic change. As a result, the high T1 slope increased Cobb's angle C2-7 (Pearson correlation coefficient 0.826) and increased C2-7 angle keep SVA C2-7 decreased (Pearson correlation coefficient -0.567) by a continuous and compensatory principle (Fig. 4)8).
As T1 slope value had been changed in various positions and aging, T1 slope cannot be used as a absolute predicting parameter for cervical lordosis. But, the TIA value is congregated in a constant value, about '70 degree' when comparing to previous study7). The TIA value in our article is 70.50 and 69.5 in previous study8). Therefore, the TIA could be considered the fixed reference value.
In addition, the high T1 slope made low SVA C2-7 by keeping C2 plumb line to the C7 plumb line and the SVA C2-7 could be negative value when much higher lordotic curvature. SVA C2-7 value also could not be the constant parameter and it means compensatory principles by head and cervical motion.
By using this fundamental principle, the spinal surgeon could make the proper fusion angle in the patients with deformity of cervico-thoracic junction by this formula. This could result in better postoperative outcomes than without optimal fusion angle8).
The limitation of this study is that each value was checked in supine position, not in upright position. It could not be absolutely compared to several previous studies with value in upright position. This article about T1 slope, neck tilt and TIA studied the basic parameters and the relationship between each parameter in supine position8). All data were collected in the upright position and the data value of T1 slope, neck tilt, TIA was different from the value of this study. But, its fundamental difference from different position means it limits itself, but it could be the database of variant motions.
The target range of this study was also made of each 20 healthy people in third decade to sixth decade. There were no control groups with healthy elder people. It was impossible to make the aging process completely with limited age group.
It could be further evaluated study by checking values in patients with each cervical spinal disease. We may explain the pathophysiology of unbalanced patients. The study could be improved by comparing to the parameters in upright position and supine by the data of cervical X-ray radiographs in upright position and cervical CT radiographs in supine position at the same time. Synchronizing both values in each neck position could be a meaningful discussion.
This analysis explains that several factors affect sagittal balance. We already know of the strong correlation between pelvis incidence and lumbar lordosis, but there are unexplored questions about cervical alignment. From the results of this study, we could discuss the change of neck tilt by aging and T1 slope, Cobb's angle C2-7, SVA C2-7. This study may lay a foundation for further study about cervical alignment.
References
1. Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007; 16:1459–1467. PMID: 17211522.

2. Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005; 18:40–47. PMID: 15687851.

3. Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence : standard values and prediction of lordosis. Eur Spine J. 2006; 15:415–422. PMID: 16179995.

4. Ferrara LA. The biomechanics of cervical spondylosis. Adv Orthop. 2012; 2012:493605. PMID: 22400120.

5. Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976). 1995; 20:1351–1358. PMID: 7676332.

6. Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 1986; 11:521–524. PMID: 3787320.

7. Hardacker JW, Shuford RF, Capicotto PN, Pryor PW. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976). 1997; 22:1472–1478. discussion 1480. PMID: 9231966.

8. Jang JS, Lee SH, Min JH, Kim SK, Han KM, Maeng DH. Surgical treatment of failed back surgery syndrome due to sagittal imbalance. Spine (Phila Pa 1976). 2007; 32:3081–3087. PMID: 18091505.

9. Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010; 10:994–998. PMID: 20970739.

10. Kuntz C 4th, Levin LS, Ondra SL, Shaffrey CI, Morgan CJ. Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults : a review and resynthesis of the literature. J Neurosurg Spine. 2007; 6:104–112. PMID: 17330576.

11. Lee CS, Chung SS, Kang KC, Park SJ, Shin SK. Normal patterns of sagittal alignment of the spine in young adults radiological analysis in a Korean population. Spine (Phila Pa 1976). 2011; 36:E1648–E1654. PMID: 21394071.

12. Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 2012; 25:E41–E47. PMID: 22037167.

13. Silber JS, Lipetz JS, Hayes VM, Lonner BS. Measurement variability in the assessment of sagittal alignment of the cervical spine : a comparison of the gore and cobb methods. J Spinal Disord Tech. 2004; 17:301–305. PMID: 15280759.

14. Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005; 87:260–267. PMID: 15687145.

Fig. 1
A : T1 slope : the angle between a horizontal line and the upper end plate of T1. B : Neck tilt : the angle formed by a vertical line of sternum tip and the line drawn in the center of upper end plate. C : Cobb's angle C2-7 : the angel between the horizontal line of C2 lower end plate and the horizontal line of C7 lower end plate. D : SVA C2-7 : the distance between the plumb line of C2 dens tip and the plumb line of the center of C7 upper end plate. SVA : sagittal vertical axis.
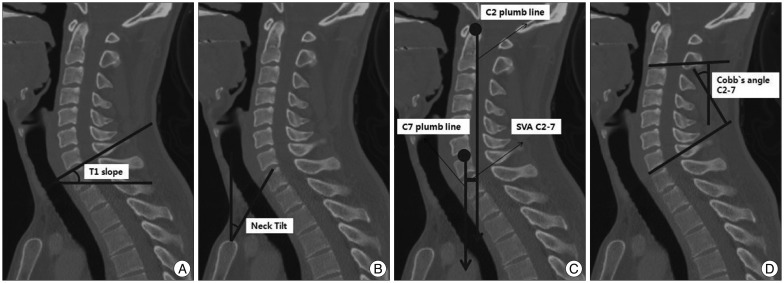
Fig. 4
As increasing T1 slope (A), the Cobb's angle C2-7 (B) is getting higher. Consecutively, SVA C2-7 is getting lower and closer to the center of one's body. It shows C2 plumb line moves from anterior to posterior comparing to fixed C7 plumb line (C). SVA : sagittal vertical axis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download