Abstract
Objective
Vertebral distraction is routinely performed during anterior cervical discectomy and fusion (ACDF). Overdistraction can injure the facet joints and may cause postoperative neck pain consequently. The purpose of this study was to investigate the clinical relevance of distraction force during ACDF.
Methods
This study included 24 consecutive patients with single level cervical disc disease undergoing single level ACDF. We measure the maximum torque just before the the arm of the Caspar retractor was suspended by the rachet mechanism by turning the lever on the movable arm using a torque meter. In order to turn the lever using the torque driver, we made a linear groove on the top of the lever. We compared the neck disability index (NDI) and visual analogue scale (VAS) scores between the high torque group (distraction force>6 kgf·cm) and the low torque group (distraction force≤6 kgf·cm) at routine postoperative intervals of 1, 3, 5 days and 1, 3, 6 months.
Results
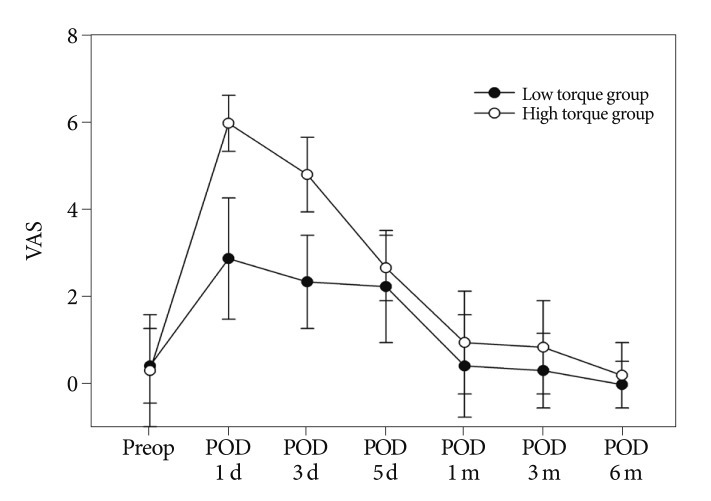
The VAS scores for posterior neck pain had a linear correlation with torque at postoperative 1st and 3rd days (y=0.99×-1.1, r2=0.82; y=0.77×-0.63, r2=0.73, respectively). VAS scores for posterior neck pain were lower in the low torque group than in the high torque group on both 1 and 3 days postoperatively (3.1±1.3, 2.6±1.0 compared with 6.0±0.6, 4.9±0.8, p<0.01). However, the difference in NDI scores was not statistically significant in all postoperative periods.
Vertebral distraction is routinely performed during anterior cervical discectomy and fusion (ACDF). This technique enhances surgical exposure for subsequent decompression and allows graft insertion1-4). During ACDF, it is likely that the surgeons may overdistract the vertebral bodies in order to achieve better visualization. However, overdistraction can result in the insertion of an overlarge graft13). The overlarge graft may force the anterior column to subsume an overlarge portion of the weight bearing duty. This can increase the risk of subsidence into the endplate. On the other hand, underdistraction may cause insufficient decompression and graft dislodgement or pseudarthrosis. In addition, overdistraction may cause abnormal tensile load on the facet joints. Overdistraction can be injurious to the contracted facet joints posteriorly7). We assumed that this injury may cause postoperative neck pain and disability. The purpose of this study was to investigate the clinical relevance of distraction force during ACDF.
Between 2010 and 2011, 24 consecutive patients with single level cervical disc disease undergoing single level ACDF at our hospital were included. After the approval from the Institutional Review Board of our hospital, 12 men and 12 women participated and completed this study. The age of the patients at the time of surgery ranged from 31 to 61 years (mean, 47.4±10.1 years). The inclusion criteria was single level degenerative disc disease between C3-C4 or C6-C7. All the patients had only radicular pain without neck pain refractory to a minimum 6 weeks of conservative treatment. The exclusion criteria included : multi-level disc disease; cervical stenosis; severe spondylosis; previous cervical surgery; deformity; and patient age more than 70 years. All operations were performed by D.A.S. using the same surgical protocol. Data were collected and analyzed by S.M.H.
The patient was positioned in a physiological neutral position. A standard Smith-Robinson approach was used to expose the symptomatic level in all the patients. The surgical technique used was basically the same in all the patients. The examination was performed during the intraoperative procedure. We used the Caspar retractor (Aesculap, PA, USA) in order to open up the disc space. The Caspar retractor consists of a rack-and-pinion and a two armed (one fixed and the other moveable) compartment. Each Caspar pin was placed in the center of the upper and lower vertebral bodies. After confirmation of pin placement, the Caspar retractor was attached to the pins. A square incision was made along the border of both the endplate and bilateral uncus using a number 11 blade. Anterior annular tissue was completely removed along with anterior longitudinal ligament using a pituitary rongeur. Then, the disc space was distracted by an average of additional 2 to 3 mm over the preoperative disc height by turning the lever on the movable arm using a torque meter (Tohnichi, Tokyo, Japan), which had a maximum capacity of 10.0 kgf·cm and had an accuracy of less than 3 percent. In order to turn the lever using the torque driver, we made a linear groove on the top of the lever (Fig. 1). We stopped turning the lever when sufficient intervertebral space was exposed. The maximum torque just before the arm was suspended by the ratchet mechanism was recorded. After the measurement, a standard discectomy was performed. According to preliminary data, the subjects were divided into two groups based on the torque force (high torque group : >6 kgf·cm; low torque group : ≤6 kgf·cm).
Clinical evaluation was performed by a nurse specializing in pain management who was blinded to the patients' treatment allocations. The patients were asked to check the neck disability index (NDI) and grade their pain intensity before surgery, and at routine postoperative intervals of 1, 3, 5 days and 1, 3, 6 months. The NDI scores were expressed in a range from 0 (no disability) to 50 (maximum disability). Pain intensity was reported on a scale of 0 to 10 using the subjective visual analogue scale (VAS; 0=no pain; 10=the worst pain imaginable). The intervertebral disc height was obtained from preoperative and postoperative cervical X-rays. The subject lay in a supine neural position and scans were performed. The middle disc height of images was measured by S.M.H.
The results were expressed as mean±standard deviation. Linear regression analysis was used to evaluate the relationship between the torque force and the VAS scores for neck pain. Statistical analysis was performed with SPSS Version 16.0 for Windows (SPSS, Inc., Chicago, IL, USA).
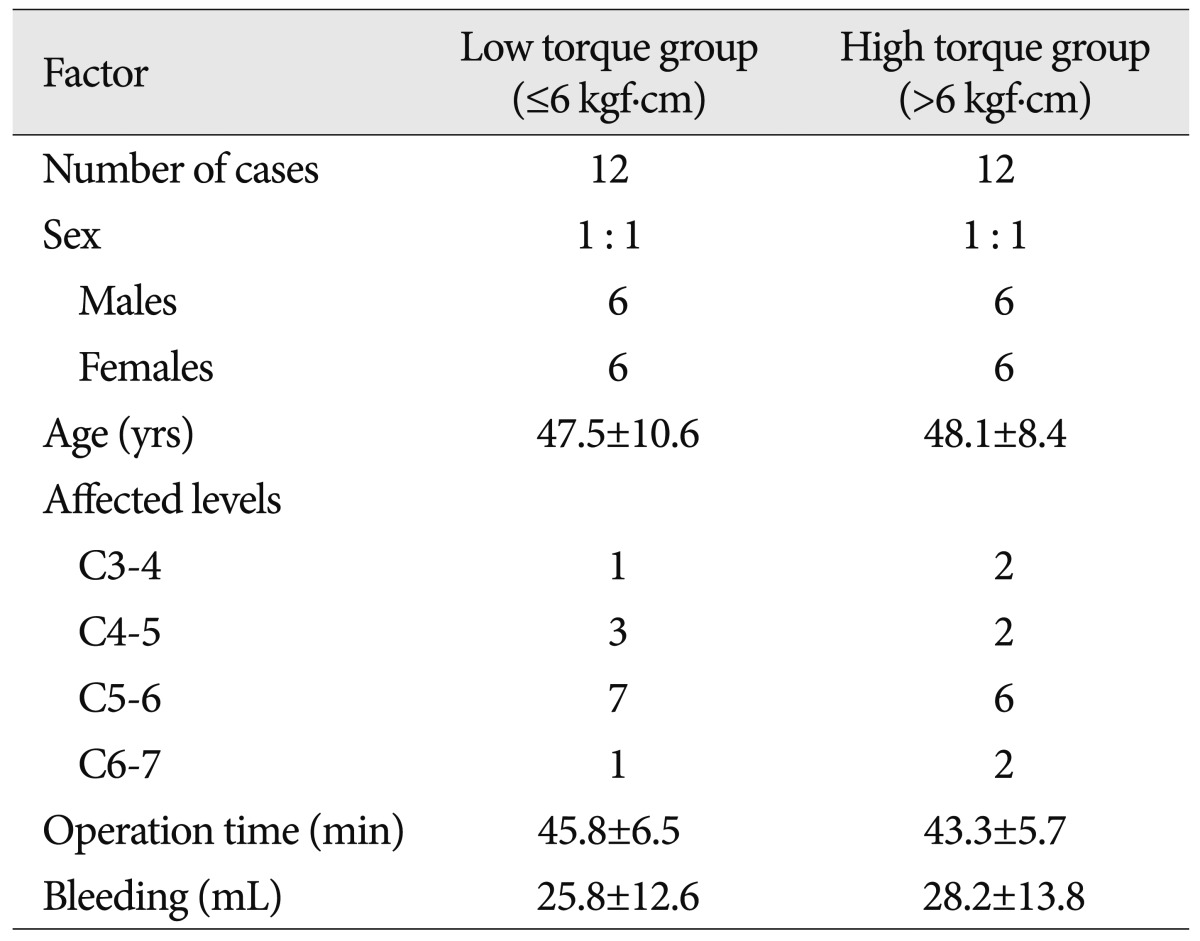
In the low torque group, the mean age of 12 patients (6 males and 6 females) undergoing ACDF was 47.5±10.6 years. The mean operation time was 45.8±6.5 minutes and the mean amount of bleeding was 25.8±12.6 mL. Meanwhile, in the high torque group, the mean age of 12 patients (6 males, 6 females) undergoing ACDF was 48.1±8.4 years. The mean operation time was 43.3±5.7 minutes and the mean amount of bleeding was 28.2±13.8 mL. From these data, it is apparent that there were no significant differences between the two groups with regard to age, sex, operation time, and amount of bleeding (Table 1).
The VAS scores for posterior neck pain had a linear correlation with torque at postoperative 1st and 3rd days (y=0.99×-1.1, r2=0.82; y=0.77×-0.63, r2=0.73, respectively Fig. 2). After 5 days postoperatively, there was no correlation between VAS scores for posterior neck pain and torque. Nine (37.5%) among twenty-four patients had VAS scores of more than 6 for neck pain. All cases with significant VAS pain scores of more than 6 had the torque value of more than 6 kgf·cm. The mean VAS scores for posterior neck pain in the low torque group were at 0.8±0.8 on admission, 3.1±1.3 on day 1 postoperatively, 2.6±1.0 on day 3 postoperatively, 2.5±1.2 on day 5 postoperatively, 0.8±1.1 at one month postoperatively, 0.7±0.8 at three months postoperatively, and 0.4±0.5 at six months postoperatively. In the high torque group, the equivalent values were 0.7±1.2, 6.0±0.6, 4.9±0.8, 2.9±0.7, 1.3±1.1, 1.2±1.0, and 0.6±0.7. VAS scores for posterior neck pain were lower in the low torque group than in the high torque group on both 1 and 3 days postoperatively (3.1±1.3, 2.6±1.0 compared with 6.0±0.6, 4.9±0.8, p<0.01) (Fig. 3).
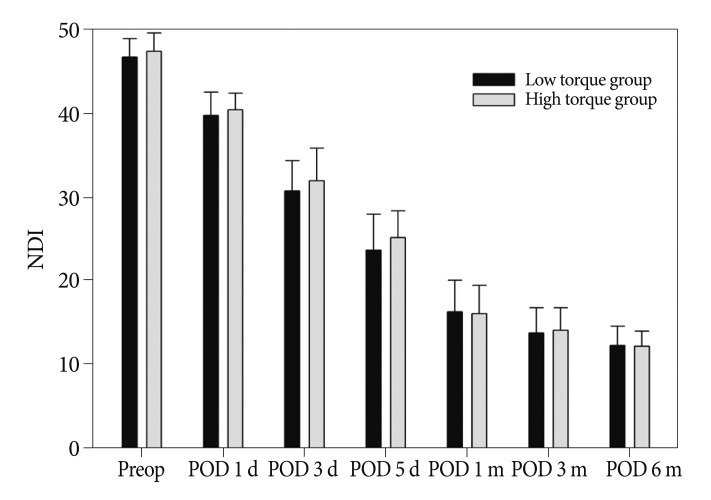
While VAS scores for posterior neck pain showed a linear correlation with torque at postoperative 1st and 3rd days, NDI scores did not show any correlation with torque in all postoperative periods. The mean NDI scores in the low torque group were 46.8±2.2 on admission, 39.8±2.8 on day 1 postoperatively, 30.8±3.6 on day 3 postoperatively, 23.7±4.3 on day 5 postoperatively, 16.3±3.8 at one month postoperatively, 13.8±3.0 at three months postoperatively, and 12.3±2.3 at six months postoperatively. In the high torque group, the equivalent values were 47.5±2.2, 40.5±2.0, 32.0±3.9, 25.2±3.2, 16.1±3.4, 14.1±2.7, and 12.2±1.8. The difference in NDI scores between the low torque group and the high torque group was not statistically significant in all postoperative periods (Fig. 4).
There was a mean increase of 2.1 mm in disc height at 24 operated segments. The mean disc height increased from 4.1±1.4 mm to 6.2±1.9 mm. In the low torque group, eleven of the 12 subjects gained height postoperatively. The mean gain in height was 1.9 mm while the standard deviation was 1.2 mm. In the high torque group, all subjects gained height after surgery (2.2±0.9). The difference in the intervertebral disc height between the low torque group and the high torque group was not statistically significant. In addition, there were not significant relationships among the intervertebral disc height, VAS scores, NDI scores and torque.
While cervical distraction is routinely performed in anterior cervical surgery, the appropriate amount of distraction is not well defined in the literature. The graft height is usually selected based on the preoperative radiographic data and intraoperative measurement without knowing the exact distraction load. When intervertebral disc space is insufficiently exposed after initial distraction, surgeons habitually turn the lever of the Caspar retractor without considering how much excessive force is being applied to the vertebra. There have been several studies evaluating and quantifying the appropriate distraction load during surgery. Truumees et al.15,16) examined the interrelations of preoperative disc height, graft height, and compressive and distractive forces in an anterior cervical surgery. Demetropoulos et al.5) developed a load sensing cervical distractor to assess the applied load during ACDF. Frank et al.6) investigated the intraoperative measurement of cervical motion segment stiffness by applying a distraction load. Aryan et al.1) examined the intraoperative distraction force of the cervical intervertebral disc segment during anterior cervical discectomy, and the results showed that a sharp reduction in the strain across the intervertebral space occurred after distraction. However, none of the studies evaluated the correlation between the clinical outcome and distraction force.
This is a novel research investigating the clinical relevance of distraction force during ACDF. The objective of this study was achieved because the correlations between distraction force and posterior neck pain and disability were determined. According to our analysis, posterior neck pain appeared to be worsened by a strong distraction force (>6 kgf·cm) at postoperative 1st and 3rd days. We assume that posterior neck pain was caused due to stretching of the facet joint by cervical distraction. There are numerous evidences that suggest that the facet joint is the pain generator11,14). In the in vivo experiments, it was proved that the mechanical load on the facet joints caused neck pain9,17). There are nociceptive nerve fibers throughout the structures of the facet joints, including the facet joint's capsular ligament. Also, anesthetic block of painful facet joints offers pain relief8,10,12). Therefore, it was assumed that vertebral distraction caused mechanical overload on the facet joints and subsequent neck pain. Moreover, we think that the patients with herniated cervical disc are more sensitive to distraction force because they have more number of degenerative facet joints and contracted ligaments.
On the other hand, NDI scores were not correlated with distraction force in all postoperative periods. The reason for this lack of correlation was that not only posterior neck pain but also wound pain and radicular pain may result in an increase in NDI scores during the postoperative period.
According to our study, surgeons are able to acknowledge the exact distraction force required and avoid excessive distraction by using a simple torque driver. If the distraction force affects the surgical outcome, controlling the distraction force will become essential. The results of this study highlight the clinical relevance of distraction force in the immediate postoperative period. As compared with the equipment reported previously, this device can be easily applied in anterior cervical surgery in which cervical distraction is essential.
This study has certain important limitations, however, mostly stemming from its small sample size. We also know that postoperative neck pain associated with vertebral distraction is transient. Also, the estimated distraction force is actually the rotation torque rather than the true distraction force. However, when we turn the lever of the Caspar retractor, we control the rotation force and not the distraction force. In addition, a further study is necessary to elucidate the changes of the segmental angle, and facet joint space according to the distraction force.
Acknowledgements
This study was partially supported by a grant of the Korea Healthcare technology R&D project, Ministry for Health & Welfare Affairs, Republic of Korea (A111016).
References
1. Aryan HE, Newman CB, Lu DC, Hu SS, Tay BK, Bradford DS, et al. Relaxation of forces needed to distract cervical vertebrae after discectomy : a biomechanical study. J Spinal Disord Tech. 2009; 22:100–104. PMID: 19342931.

2. Bailey RW, Badgley CE. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg Am. 1960; 42-A:565–594. PMID: 13848906.

3. Caspar W, Barbier DD, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery. 1989; 25:491–502. PMID: 2797387.

4. Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958; 15:602–617. PMID: 13599052.

5. Demetropoulos CK, Truumees E, Herkowitz HN, Yang KH. Development and calibration of a load sensing cervical distractor capable of withstanding autoclave sterilization. Med Eng Phys. 2005; 27:343–346. PMID: 15823476.

6. Frank E, Chamberland D, Ragel B. A proposed technique for intraoperative measurement of cervical spine stiffness. Neurosurgery. 1996; 39:147–150. PMID: 8805151.

7. Goffin J, Plets C, Van den Bergh R. Anterior cervical fusion and osteosynthetic stabilization according to Caspar : a prospective study of 41 patients with fractures and/or dislocations of the cervical spine. Neurosurgery. 1989; 25:865–871. PMID: 2601816.

8. King JS, Lagger R. Sciatica viewed as a referred pain syndrome. Surg Neurol. 1976; 5:46–50. PMID: 772852.
9. Kuslich SD, Ulstrom CL, Michael CJ. The tissue origin of low back pain and sciatica : a report of pain response to tissue stimulation during operations on the lumbar spine using local anesthesia. Orthop Clin North Am. 1991; 22:181–187. PMID: 1826546.
10. Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol M. Radiofrequency facet joint denervation in the treatment of low back pain : a placebo-controlled clinical trial to assess efficacy. Spine (Phila Pa 1976). 2001; 26:1411–1416. discussion 1417. PMID: 11458140.

11. Lee KE, Thinnes JH, Gokhin DS, Winkelstein BA. A novel rodent neck pain model of facet-mediated behavioral hypersensitivity : implications for persistent pain and whiplash injury. J Neurosci Methods. 2004; 137:151–159. PMID: 15262055.

12. Manchikanti L, Singh V, Falco FJ, Cash KM, Fellows B. Cervical medial branch blocks for chronic cervical facet joint pain : a randomized, double-blind, controlled trial with one-year follow-up. Spine (Phila Pa 1976). 2008; 33:1813–1820. PMID: 18670333.
13. Olsewski JM, Garvey TA, Schendel MJ. Biomechanical analysis of facet and graft loading in a Smith-Robinson type cervical spine model. Spine (Phila Pa 1976). 1994; 19:2540–2544. PMID: 7855678.

14. Panjabi MM. Clinical spinal instability and low back pain. J Electromyogr Kinesiol. 2003; 13:371–379. PMID: 12832167.

15. Truumees E, Demetropoulos CK, Yang KH, Herkowitz HN. Effects of disc height and distractive forces on graft compression in an anterior cervical discectomy model. Spine (Phila Pa 1976). 2002; 27:2441–2445. PMID: 12435972.

16. Truumees E, Demetropoulos CK, Yang KH, Herkowitz HN. Effects of disc height and distractive forces on graft compression in an anterior cervical corpectomy model. Spine (Phila Pa 1976). 2008; 33:1438–1441. PMID: 18520939.

17. Winkelstein BA, Santos DG. An intact facet capsular ligament modulates behavioral sensitivity and spinal glial activation produced by cervical facet joint tension. Spine (Phila Pa 1976). 2008; 33:856–862. PMID: 18404104.

Fig. 1
An illustration of the measurement of distraction force by a torque driver and the Caspar retractor.
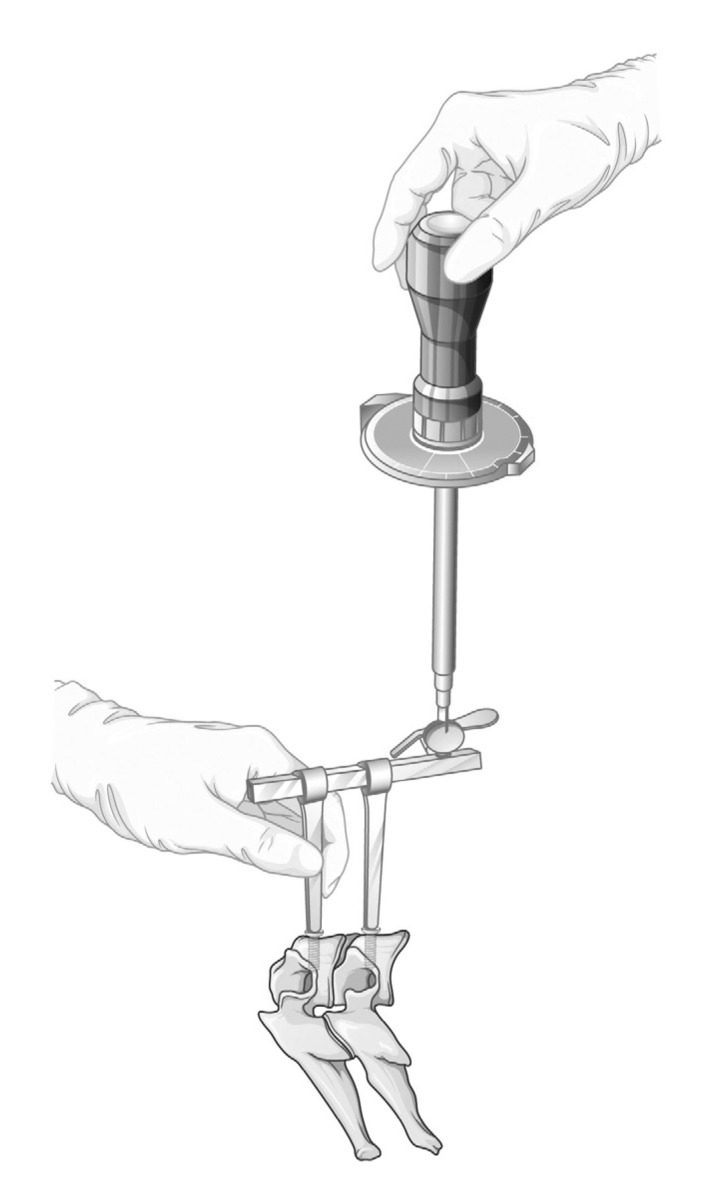
Fig. 2
The correlation between the VAS scores for neck pain and distraction force throughout the postoperative period in patients undergoing ACDF. VAS : visual analogue scale, ACDF : anterior cervical discectomy and fusion.
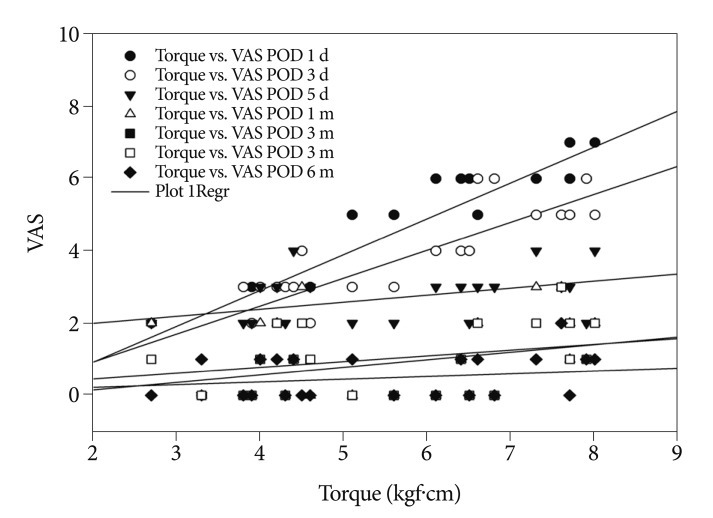
Fig. 3
The comparison of VAS scores for posterior neck pain throughout the postoperative period between the low torque group and the high torque group. VAS : visual analogue scale.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download