Abstract
Rhabdomyolysis is a rare but potentially life-threatening disorder caused by the release of injured skeletal muscle components into the circulation. The authors report a case of severe head injury, in which a hyperosmolar state and continuous seizure complicated by severe rhabdomyolysis and acute renal failure evolved during the course of treatment resulted in a fatal outcome despite intensive supportive treatment. Our bitter experience suggests that rhabdomyolysis should be born in mind in patients with severe head injury who may develop hyperosmolar state and continuous seizure.
Rhabdomyolysis causes muscle breakdown and the leakage of intracellular muscle constituents (e.g., enzymes, electrolytes, myoglobin) into the circulation and extracellular fluid3,4). When massive amounts of myoglobin are released, the binding capacity of plasma proteins is exceeded and the myoglobin reaches renal tubules and can cause acute renal failure8). Prolonged mental deterioration and convulsive seizures should be included among the neurological conditions in which rhabdomyolysis can develop1). A case is presented in which prolonged mental deterioration with hyperosmolar state and continuous convulsive seizure after head injury led to rhabdomyolysis and acute renal failure. The pathophysiological mechanism of this uncommon entity after severe head injury is discussed and a review of relevant literature is included.
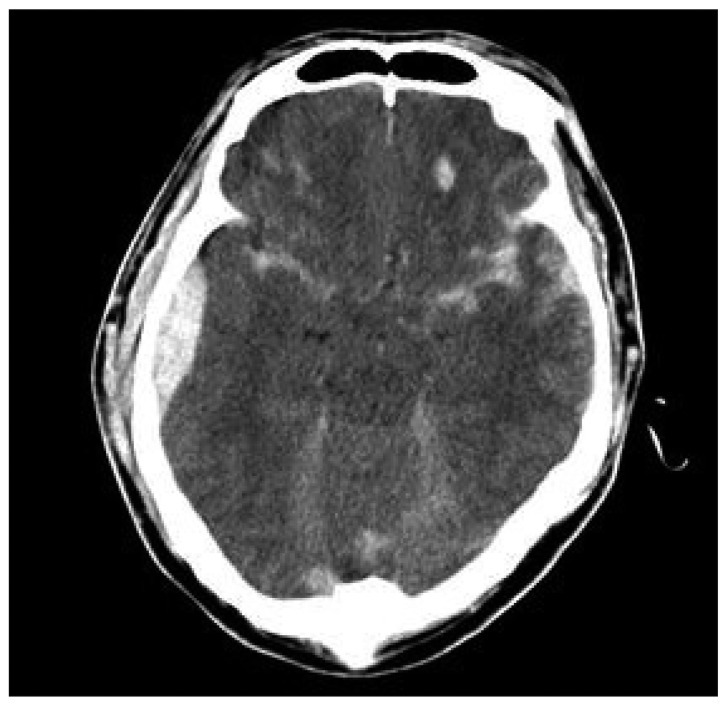
A previously healthy 42-year-old man was referred to our emergency department due to a deteriorating mental status after a car accident. Emergency services reported decreased mental status and a Glasgow Coma Scale score of 7. There were no associated systemic injuries, muscle contusions, internal organ damage or swelling of the extremities. However, he showed decerebrated rigidity at both arms and legs. On admission, sodium, potassium, and osmolarity were 143 meq/L, 3.5 meq/L, and 335 mmol/L, respectively. Computed tomography (CT) showed diffuse cerebral swelling consistent with hemorrhagic contusion and epidural hematoma at right temporoparietal area (Fig. 1). 150 mL of mannitol solution (20%) every 4 hours was prescribed. However, despite treatment to lower intracranial pressure (ICP), that is, mannitol, mild hyperventilation, and extraventricular drainage (EVD), his mental status remained semicomatose and recurrent convulsive generalized tonic-clonic seizures developed, and thus, he was admitted to the neurosurgical intensive care unit for adequate hydration, anticonvulsant and correction of the metabolic derangement. Unfortunately, myoglobinuria developed 3 days after admission with a high serum creatine kinase (CK) level up to 48, 837 IU/L (normal 55-215 IU/L). At this time, his serum sodium, potassium, and osmolarity were 152 meq/L, 3.0 meq/L and 352 mmol/L. Acute renal failure developed 3 days after admission despite intensive fluid replacement and diuresis. CK level peaked at 52, 825 IU/L on day 5, and serum myoglobin exceeded 25 mg/dL (normally <2.5 mg/dL). Despite intensive supportive treatment, the patient became anuric 5 days after admission and required hemodialysis. No source of muscle breakdown was evident, but his condition deteriorated rapidly, culminating in cardiorespiratory arrest with dilated non-reactive pupils. He died 8 days after admission.
Rhabdomyolysis is a frequent concomitant of multisystem trauma, and the source of muscle breakdown is often apparent from the pattern of injury2). Although mechanical damage to muscle is the most common cause of rhabdomyolysis in trauma patients, other causes should not be overlooked. In patients with severe head injury, a prolonged deteriorated mental status, convulsive seizure, and hyperosmolar states importantly predispose significant rhabdomyolysis9,10). Our patient had a decreased mental status, which probably played a role in the development of rhabdomyolysis. Experiments with human volunteers have demonstrated that sustained lying in a fixed and rigid position can cause sufficient intramuscular pressure to occlude capillaries7). Furthermore, mannitol-induced hyperosmolar states have also be known to cause significant rhabdomyolysis. Our patient had received mannitol solution (20%) intravenously 150 mL/4 hr for 5 days, which probably aggravated his hyperosmolar state. Singhal et al.9) reported relations between the hyperosmolar state and the pathogenesis of rhabdomyolysis, and observed that serum sodium and serum osmolarity were both linearly related to serum CK. It was also noted that hypokalemia and hypophosphatemia were present in patients who developed rhabdomyolysis. In our patient, a hyperosmolar state, hypernatremia, and hypokalemia, were all present, and serum CK reached an extremely high level. It is known that the combination of potential potassium and phosphate deficiency in combination with acidosis, hypernatremia, and a hyperosmolar state, can reduce sodium release from muscle cells, and thus, decrease transmembrane potentials, which animal experiments have shown is a crucial precursor of rhabdomyolysis5). In addition, our patient experienced convulsive seizures and intense rigidity, and in our opinion, these factors are also likely to predispose rhabdomyolysis. Partial and generalized seizures affect autonomic function during seizures. The cause of muscle injury in exertional rhabdomyolysis has been postulated to be energy deficiency. During maximal exertion, energy is obtained almost solely from muscle glycogen, and if exertional requirements exceed available energy stores, muscle glycogen is depleted10). Furthermore, if energy production is deficient, energy rich phosphate compounds are subject to subcellular competition and insufficient energy is available for muscle cell membrane structural maintenance, which results in changes ranging from reversible permeability to cell death. This type of cellular damage results in the release of intracellular potassium, purine, creatinine, myoglobin, and creatine kinase. Fever, malaise, weakness, and extremity pain, as well as swelling and tenderness are usually reported when the onset of rhabdomyolysis results from exertion. In patients with a deteriorated mental status, fever and discoloration of urine should suggest the condition.
Management of rhabdomyolysis and myoglobinuria begins with removing the cause, if possible. However, volume contraction, hypernatremia and the hyperosmolar state in neurosurgical patients treated with osmotic diuretic agents for brain swelling should be done with caution. The most appropriate treatment for hyperosmolar state-induced rhabdomyolysis is adequate hydration and alkaline diuresis. In patients with convulsive seizures or rigidity, sustained muscle contractions may be modified by the use of an anticonvulsant or muscle relaxant. Dialysis may be required if renal failure persists; indications for dialysis include hyperkalemia, uremic pericarditis, or encephalopathy, and evidence of volume overload6).
References
1. Briggs TB, Smith RR. Exertional rhabdomyolysis associated with decerebrate posturing. Neurosurgery. 1986; 19:297–299. PMID: 3748364.

2. Chen CM, Chen JC, Kao MC. Severe rhabdomyolysis with good recovery in a patient with head injury : case report. Neurosurgery. 1997; 41:293–296. PMID: 9218322.

3. Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review : rhabdomyolysis -- an overview for clinicians. Crit Care. 2005; 9:158–169. PMID: 15774072.
4. Jeon HJ, Cho BM, Oh SM, Park SH. Lumbosacral plexopathy, complicating rhabdomyolysis in a 57-year-old man, presented with sudden weakness in both legs. J Korean Neurosurg Soc. 2007; 42:481–483. PMID: 19096594.

5. Knochel JP, Carter NW. The role of muscle cell injury in the pathogenesis of acute renal failure after exercise. Kidney Int Suppl. 1976; 6:S58–S64. PMID: 135855.
6. Larner AJ. Rhabdomyolysis associated with cranial diabetes insipidus. Postgrad Med J. 1992; 68:149. PMID: 1520370.

7. Owen CA, Mubarak SJ, Hargens AR, Rutherford L, Garetto LP, Akeson WH. Intramuscular pressures with limb compression clarification of the pathogenesis of the drug-induced muscle-compartment syndrome. N Engl J Med. 1979; 300:1169–1172. PMID: 431646.
8. Poels PJ, Gabreels FJ. Rhabdomyolysis : a review of the literature. Clin Neurol Neurosurg. 1993; 95:175–192. PMID: 8242960.
9. Singhal PC, Abramovici M, Venkatesan J. Rhabdomyolysis in the hyperosmolal state. Am J Med. 1990; 88:9–12. PMID: 2294777.

10. Singhal PC, Chugh KS, Gulati DR. Myoglobinuria and renal failure after status epilepticus. Neurology. 1978; 28:200–201. PMID: 564002.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download