Abstract
Objective
Posture induced common peroneal nerve (CPN) palsy is usually produced during the prolonged squatting or habitual leg crossing while seated, especially in Asian culture and is manifested by the onset of foot drop. Because of its similarity to discogenic foot drop, patients may be diagnosed with a lumbar disc disorder, and in some patients, surgeons may perform unnecessary examinations and even spine surgery. The purpose of our study is to establish the clinical characteristics and diagnostic assessment of posture induced CPN palsy.
Methods
From June 2008 to June 2012, a retrospective study was performed on 26 patients diagnosed with peroneal nerve palsy in neurophysiologic study among patients experiencing foot drop after maintaining a certain posture for a long time.
Results
The inducing postures were squatting (14 patients), sitting cross-legged (6 patients), lying down (4 patients), walking and driving. The mean prolonged neural injury time was 124.2 minutes. The most common clinical presentation was foot drop and the most affected sensory area was dorsum of the foot with tingling sensation (14 patients), numbness (8 patients), and burning sensation (4 patients). The clinical improvement began after a mean 6 weeks, which is not related to neural injury times. Electrophysiology evaluation was performed after 2 weeks later and showed delayed CPN nerve conduction study (NCS) in 24 patients and deep peroneal nerve in 2 patients.
Foot drop may develop with various clinical conditions. It can be caused by posture induced common peroneal nerve (CPN) palsy, a kind of peripheral nerve entrapment syndrome common in Asian culture as a result of sitting preferences. Peroneal nerve innervates muscle groups related to ankle motion while walking, and patients have difficulties in normal gait if injured. As the clinical symptoms presented by peroneal nerve palsy are similar to that of discogenic foot drop, it is easy to misdiagnose, and may occasionally lead to unnecessary evaluations and treatments. Although several studies concerning peroneal nerve injury related with surgery, trauma, and tumor have been reported3), it is difficult to find clinical reports on posture induced peroneal nerve palsy, which is common in Asian culture. This study will explain the clinical characteristics of peroneal nerve palsy patients developed after maintaining a certain posture for a long time and will stipulate several important differentiation points for making a diagnosis in review of the literature.
From June 2008 to June 2012, a retrospective study examined the records of 35 patients diagnosed with peroneal nerve palsy in neurophysiologic study among patients experiencing foot drop after maintaining a certain posture for a long time. The information on individual clinical characters, such as motor and sensory presentations, related postures, period and pattern of clinical improvement, muscle strength assessments, such as ankle dorsiflexion (AKDF), big toe dorsiflexion (BTDF), and ankle eversion, were retrieved from medical records with a follow-up period of a minimum of 3 months to 36 months. Nine patients were excluded due to improper medical records; as such, 26 patients were enrolled in this study.
This study was confirmed with Hallym University Institutional Review Board, #2012-71.
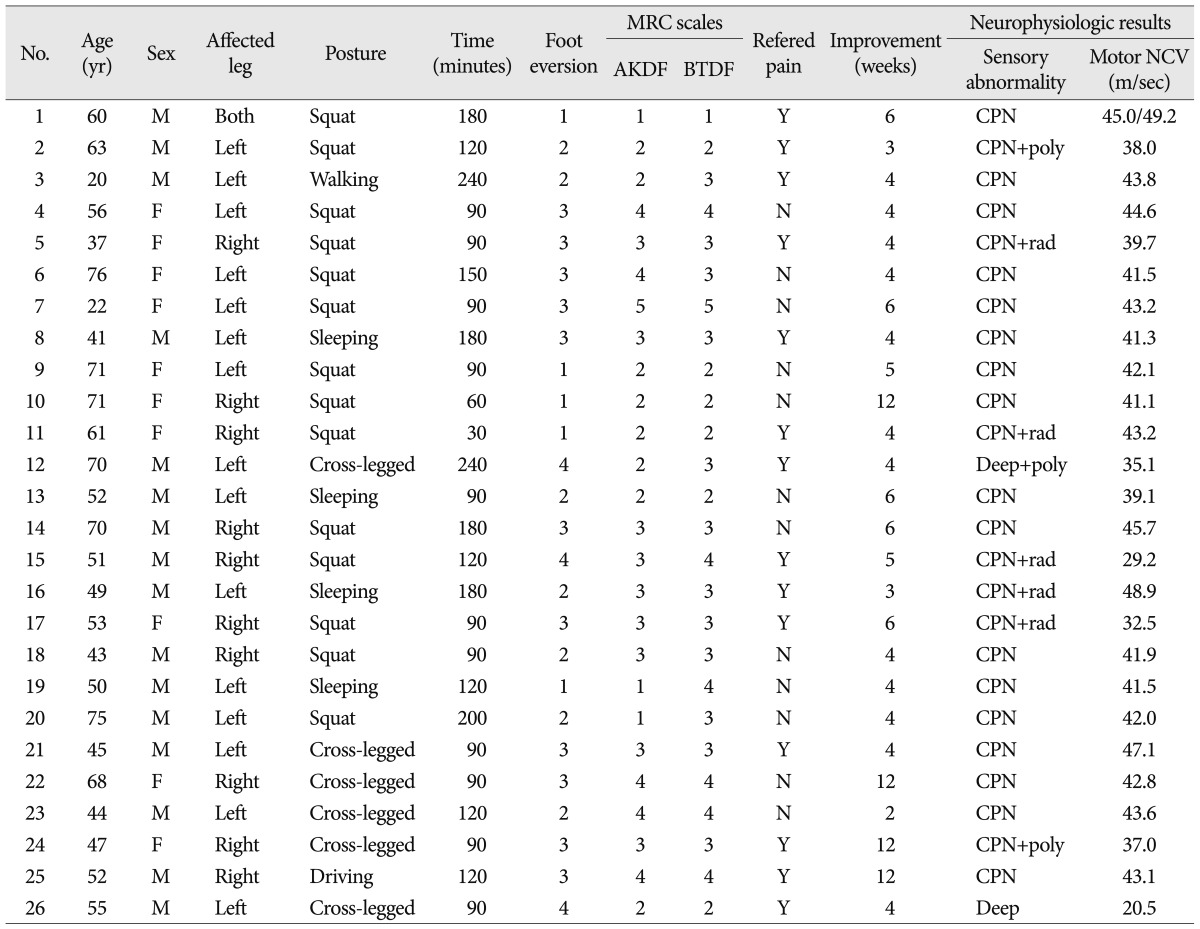
A summary of the entire series of patients is in Table 1. There were 16 males (61%) and 10 females (39%). The median age at diagnosis was 54 years (range, 22-76 years). Affected legs were on the right leg for 11 patients, left 14 patients and bilateral legs for 1 patient.
The inducing postures were squatting (14 patients), sitting cross-legged (6 patients), lying down (4 patients), walking for 4 hours (1 patient) and driving for 2 hours (1 patient). The peroneal nerve was affected by maintaining the same posture for an average of 124.2 minutes.
All patients visited the hospital for foot drop, but sensory deficit was observed in the dorsum of the foot, lateral side of the affected leg through physical examination. Except for 4 patients that slept in a drunken state, 22 patients preferentially experienced sensory disturbance (tingling sensation 63%, numbness 27%, burning sensation 10%) in the affected leg, while maintaining the same posture before experiencing a foot drop. Although these areas were related with sensory dermatome innervated by CPN or its branches, the affected areas complained by 14 patients (53%) included in the knee or the lower part of the thigh.
The muscle tones of AKDF, BTDF, and foot eversion were evaluated using medical research council (MRC) scale for muscle strength and the mean MRC grade 3/5 on AKDF and BTDF, 2/5 on foot eversion were observed. Eleven patients (42%) were rated at MRC grade below 2.
This neurophysiologic study occurred after 2 weeks. Delayed sensory conduction velocity of CPN was observed in 24 patients, deep peroneal nerve in 2 patients. Five patients also showed L5 radiculopathy, and 3 patients showed polyneuropathy. The mean motor conduction velocities of affected CPN were 41.13 (m/sec) on the right side and 42.26 (m/sec) on the left side (normal reference : 33-53 m/sec). Only one patient was observed with a severe delayed motor conduction velocity, 20.50 (m/sec).
Clinical improvement started with diminishing sensory disturbance and then motor weakness was also recovered. Clinical improvement took 6 weeks on average. Sixteen patients showed clinical improvement within 4 weeks, 6 patients during 4 to 6 weeks, and 4 patients improved late, after 12 weeks. When examined at 12 months, 20 patients had fully recovered, whereas 6 patients still had motor deficit and sensory disturbance. The period of clinical improvement was not related to the time in which patients maintained a posture that affected peroneal nerve.
Posture induced CPN palsy is a nerve entrapment syndrome presented as a foot drop after maintaining certain positions, such as squatting, kneeling or habitual leg crossing while seated in Asian culture. As unique cultural specificity, the previous reports about CPN palsy have been restricted to mechanical direct injuries, like as laceration, fracture, and surgery, and there are few reports on the etiology or clinical characteristics of posture induced CPN palsy.
Patient history and neurological examination area are the most important initial clinical approach to reach a diagnosis of suspected peroneal neuropathy. Hematologic and metabolic condition studies may give some clue regarding the risk factors like diabetes mellitus, hyperthyroidism, polyarteritis nodosa, and alcoholic polyneuropathy.
Although an accurate misdiagnosis rate has not been reported, Baima has reported that ankle inversion by tibialis posterior muscle showed ankle dorsiflexion, making it difficult to discriminate from foot drop caused by peroneal nerve palsy3). In this study, 5 out of 26 patients received a lumbar MRI examination. The examination was performed not because of difficulties in diagnosis, but to check the possibility of acute herniated lumbar disc as these patients were treated with radiculopathy prior to foot drop.
There are several clinical pitfalls that make differentiation from discogenic foot drop difficult. First, in their first visit patients that experienced back pain and paresthesia of the affected lower extremity in the past explained that they were treated for herniated lumbar disc and had visited the hospital once again due to worsened herniated lumbar disc symptoms. This prevented clinicians from having enough time to conduct history taking and make an accurate diagnosis, leading to inappropriate evaluations and unnecessary treatments. Second, as the referred pain by CPN can be formed from the knee and the lateral thigh to the dorsum of the foot, patients can describe referred pain as radiculopathy flowed from the above and complain of paresthesia and sensory deficit. Clinicians accustomed to referred pain related to discogenic radiculopathy can mistake the symptoms for herniated lumbar disc. Third, in some clinical aspects, complete palsy of CPN caused by direct injury can be seen as the only foot drop that is not always accompanied by sensory disturbance and can easily be diagnosed. However, in cases of posture induced CPN palsy with sensory deficit, caused by ischemia due to compression or stretching after maintaining posture8,12), Humphreys et al.6) reported that sensory disturbances were identified in 92% on CPN palsy patients, incomplete information that CPN is a pure motor nerve that may lead to misdiagnosis.
The problem in our patients developed with sensory disturbance in the affected legs before foot drop, except for the four drunken patients with deep sleep. Sensory deficit was recovered after 3 weeks and muscle strength was gradually improved afterward. Thus, sensory neurologic change should be checked from the onset time to the end of treatment, and the first symptom of sensory disturbance is not implicated only as a discogenic radiculopathy.
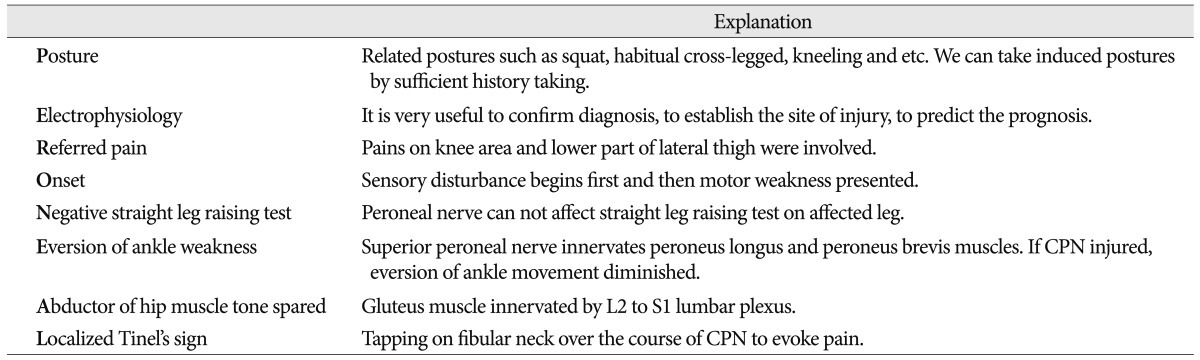
Although studies of clinical characteristics or physical examinations may be helpful for determining posture induced CPN palsy, they have not been reported, and several reports will be reviewed in relation to this study.
As the gluteus muscle is mostly innervated by the lumbosacral plexus, assessment of hip abductor muscle strength in foot drop patients is useful in differentiating CPN palsy and lumbar radiculopathy, with 85.7% sensitivity and 96.4% specificity7). The author also believes that as ankle foot motion is variable or patients are not accustomed to specific ankle motions, such as ankle inversion or eversion, it is useful to evaluate the strength of muscles that CPN does not innervate. A diminished hip abductor muscle tone can be simultaneously observed in patients with lumbar disc herniation that can induce a foot drop. A similar method tests non-evoked pain in straight leg raising test of the affected leg, meaning the possibility of discogenic foot drop is low.
Tinel's sign is an examination to detect an injured nerve by tapping over the fibro-osseous tunnel to induce a sensory disturbance along distribution of the nerve. It can apply to posture induced CPN palsy. Anatomically, the peroneal nerves superficially pass from the fibula neck3,9). If the CPNs are entrapped or irritated, tapping over the fibro-osseous tunnel will trigger pain or sensory presentation in peroneal nerve distribution. As with other entrapment syndromes, Tinel's sign is helpful to diagnose CPN palsy6).
Although understanding the clinical characteristics mentioned above helps differentiate discogenic foot drop and CPN palsy, the most important part of a diagnosis is careful, complete history taking and gathering information on symptoms after maintaining a certain posture or engaging in certain activities. Also, it is important to inspect trauma history and check bruising or skin changes, such as ulcer or inflammation in the affected legs of patients.
Neurophysiologic evaluations can decide confirm diagnosis, establish the site of injury, assess the nerve damage, predict the prognosis8,10,12).
In most cases of peroneal nerve palsy induced by posture, the nerve injury type is neuropraxia by Sunderland's classification system. Hence, although a peroneal motor nerve conduction study (NCS) should be performed first, recording from the extensor digitorum brevis (EDB) muscle, the superficial peroneal sensory nerve action potential (SNAP) is important to help differentiate L5 radiculopathy. The abnormality of SNAP implies that the lesion is distal to the dorsal root ganglion.
In case of demyelination, the related axon remains intact and remyelination usually occurs over several weeks. However, recovery from the axonal injury requires many months or may be incomplete8). This study found symptoms improved within 4 weeks for 61% of our patients and after 12 weeks for 16%. According to Aprile et al.2), good recovery was achieved from 3-18 months for 36 peroneal nerve palsy patients, excluding 2 chronic alcoholics. In another study that classified 34 patients into 4 groups according to motor nerve conduction velocity results4), all 13 patients over 30 m/sec velocity by the initial neurophysiologic study achieved good recovery for over a year, whereas most of the patients below 30 m/sec were improved to moderate or poor recovery with gait discomfort.
Generally, medications without surgical decompression are primary treatment methods, since most patients experience spontaneous recovery within 3 months. However, not all patients have clinical improvements spontaneously, and some patients have permanent walking disability. In practice, posture induced CPN palsy patients tend to undergo passive treatments and waiting by clinicians due to a benign prognosis.
In another clinical study4), 2 out of 14 patients (14%) were in the poor recovery group, and in this study, 4 patients (15%) have difficulty in walking at 2 years follow-up. For this reason, close observation for detecting clinical recovery is important, and more favorable results will be experienced by patients through regular neurophysiologic study and peroneal distribution MRC grade check up to perform surgical decompression1,5,11).
A study on the clinical outcomes after fibrous-osseous tunnel decompression found that if clinical improvement is not achieved within 12 months, early decompression surgery will bring improved muscle strength and good prognosis in sensory recovery. Improved motor strength was reported in 74%, with an odds ratio at 14.7 (95% CI, 1.4-133.5), although the sample group only consisted of 22 patients. Sensory improvement was reported in 68% and complete sensory improvement was achieved in 47%11). As mentioned earlier, changes in clinical symptoms and improvement of neurophysiologic study are important in determining the prognosis of patients. In another surgical outcome study6), the author performed CPN decompressions for 51 CPN palsy patients by trauma, previous surgery, no identifiable causes irrelevant to clinical injured period. Postoperatively, 85% patients had motor improvement (p<0.01) and 48% patients had sensory improvement (p<0.01) with 61% pain relief. In addition, there were no patients with motor and sensory function downgraded after surgery.
We suggest that although observation is the primary treatment method, as full recovery is always not achieved at follow up six months or later, it is necessary to consider the surgical treatments by repeated neurophysiologic evaluation at the regular interval3). There were no prospective or retrospective studies on clinical results from early CPN decompression in only posture induced CPN palsy groups. Therefore, a clinical study on surgical outcome must be conducted.
In another surgical outcome study6), the author performed CPN decompressions for 51 CPN palsy patients by trauma, previous surgery, no identifiable causes irrelevant to clinical injured period. Postoperatively, 85% patients had motor improvement (p<0.01) and 48% patients had sensory improvement (p<0.01) with 61% pain relief.
Reduced muscle strength makes it impossible to maintain normal walking balance, and patients can maintain normal gaiting posture by wearing an ankle foot orthosis (AFO) to prevent passive foot plantar flexion and contraction of the ankle joint. Therefore, a clinician might recommend this brace for foot drop patients as early as possible. Recently, the peroneal nerve stimulator was developed in foot drop patients to be clinically used to stimulate and contract muscles innervated by peroneal nerves according to the walking posture of patients13). However, while this device is effective in cases of preserved peroneal nerve function, such as stroke or spinal cord injury, it is ineffective in patients with damaged peroneal nerve function.
Posture induced peroneal nerve palsy is an entrapment syndrome that is encountered in the seating habits of the Asian culture. We suggest that awareness of this clinical characteristics and diagnostic assessment methods (Table 2) may help clinicians make a diagnosis of posture induced CPN palsy and preclude unnecessary studies or inappropriate treatment in foot drop patients.
References
1. Anselmi SJ. Common peroneal nerve compression. J Am Podiatr Med Assoc. 2006; 96:413–417. PMID: 16988171.

2. Aprile I, Padua L, Padua R, D'Amico P, Meloni A, Caliandro P, et al. Peroneal mononeuropathy : predisposing factors, and clinical and neurophysiological relationships. Neurol Sci. 2000; 21:367–371. PMID: 11441574.

3. Baima J, Krivickas L. Evaluation and treatment of peroneal neuropathy. Curr Rev Musculoskelet Med. 2008; 1:147–153. PMID: 19468889.

4. Berry H, Richardson PM. Common peroneal nerve palsy : a clinical and electrophysiological review. J Neurol Neurosurg Psychiatry. 1976; 39:1162–1171. PMID: 1011026.
5. Garozzo D, Ferraresi S, Buffatti P. Surgical treatment of common peroneal nerve injuries : indications and results. A series of 62 cases. J Neurosurg Sci. 2004; 48:105–112. discussion 112. PMID: 15557879.
6. Humphreys DB, Novak CB, Mackinnon SE. Patient outcome after common peroneal nerve decompression. J Neurosurg. 2007; 107:314–318. PMID: 17695385.

7. Jeon CH, Chung NS, Lee YS, Son KH, Kim JH. Assessment of hip abductor power in patients with foot drop : a simple and useful test to differentiate lumbar radiculopathy and peroneal neuropathy. Spine (Phila Pa 1976). 2013; 38:257–263. PMID: 22805342.
8. Masakado Y, Kawakami M, Suzuki K, Abe L, Ota T, Kimura A. Clinical neurophysiology in the diagnosis of peroneal nerve palsy. Keio J Med. 2008; 57:84–89. PMID: 18677088.

9. Ozçakar L, Ozçakar ZB. Diagnosing peroneal neuropathy : the quest for the golden fleece. Pediatr Neurol. 2004; 30:299. author reply 299. PMID: 15087113.
10. Rajabally YA, Narasimhan M. Electrophysiological entrapment syndromes in chronic inflammatory demyelinating polyneuropathy. Muscle Nerve. 2011; 44:444–447. PMID: 21996806.
11. Ramanan M, Chandran KN. Common peroneal nerve decompression. ANZ J Surg. 2011; 81:707–712. PMID: 22295311.

12. Rempel DM, Diao E. Entrapment neuropathies : pathophysiology and pathogenesis. J Electromyogr Kinesiol. 2004; 14:71–75. PMID: 14759752.
13. Sheffler LR, Hennessey MT, Naples GG, Chae J. Peroneal nerve stimulation versus an ankle foot orthosis for correction of footdrop in stroke : impact on functional ambulation. Neurorehabil Neural Repair. 2006; 20:355–360. PMID: 16885421.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download