Abstract
In most cases, subdural hematoma (SDH) is regarded as a complication of head injury and nontraumatic causes are rare. Moreover, spontaneous chronic SDH in child or adolescent is very unusual. Here, we present the case of a healthy 14-year-old girl who was diagnosed as a spontaneous chronic SDH. The patient presented with severe headache following blurring of vision two weeks ago without any history of trivial head injury. Computed tomography and magnetic resonance imaging depicted a chronic SDH. The cause of the hematoma was not established. After performing burr hole drainage of the hematoma, the patient made an uneventful recovery. We explore the potential risk factors and pathophysiology implicated in this condition. Possible pathogenic mechanisms of this unique case are discussed and a review of the pertinent literature is included.
Most acute subdural hematoma (SDH) cases are result of trauma and bleeding is commonly associated with laceration of a bridging vein in the subdural space5). On the other hand, nontraumatic causes are relatively rare with an incidence rate of 3% to 5%1,10), and they predominantly affect adults in their fifth to seventh decades8). Vascular abnormalities, hematological disorders and anticoagulant therapy have been reported as predisposing factors of spontaneous SDH5,11). However, few cases of spontaneous chronic SDH without any predisposing factor in healthy young adolescents have been documented. We present this unusual case, discuss the possible pathologic mechanism, and include a review of the literature.
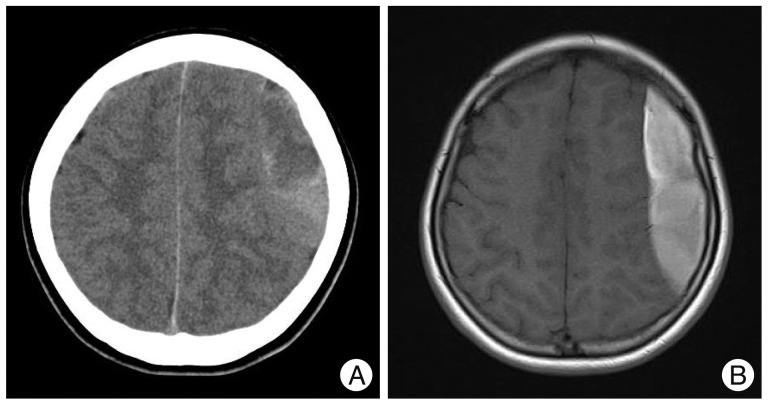
A previously healthy 14-year-old girl was admitted to our emergency room with a 2-week history of severe headache following blurring of vision, which resolved after a few minutes. She was a music student majoring in flute at middle school. There was no history of any trivial head injury. She had no previous history of anticoagulant therapy or hematological coagulopathy, and was in good health before this episode. On neurological examination, she was alert and fully oriented. No neurologic abnormalities were found in cranial nerves or the cerebellar system. Pupils were isocoric and reacted to light. However, a fundoscopic examination revealed bilateral papilledema on fundoscopic examination. A motor examination revealed slight hemiparesis (Grade IV+/Grade V) on the right side. The patient's coagulation profiles including platelet count, prothrombin time, and partial thromboplastin time were all within normal ranges. Brain computed tomography (CT) and magnetic resonance imaging (MRI) identified left-sided mixed density and high signal intensity suggesting chronic subdural hematoma (Fig. 1). She underwent burr hole evacuation of the chronic SDH; the evacuated hematoma had the typical dark appearance of chronic SDH with high pressure. She made an uneventful post-operative recovery (Fig. 2). Postoperative cerebral angiography was performed to exclude vascular risk factors for subdural hematoma, such as arteriovenous malformation, aneurysm and other vascular abnormality. However, angiographic findings were unremarkable. At her six-month follow-up, the symptoms had completely resolved. A follow-up MRI and MR angiography taken at 3 months after surgery was also unremarkable.
Acute SDH without traumatic brain injury is a rare pathological entity and accounts for fewer than 5% of SDHs1,5,10). Although this type of hematoma appears spontaneously, a cerebral aneurysm, arteriovenous malformation, hematological disorders, anticoagulant therapy, or dural arteriovenous fistula may predispose individuals to spontaneous SDH1,11). Acute spontaneous SDH appearing in the absence of predisposing conditions in young adolescents is very rare, and none of these predisposing conditions were present in our patient. Several mechanisms have been proposed to explain the occurrence of non-traumatic SDH after aneurysm rupture or bleeding of arterial origin. First, previous minor hemorrhages could fix an aneurysm to local arachnoid adhesions and result in bleeding directly into the subdural space when an arachnoid tear occurs after aneurysm rupture. Second, it could be caused by hemorrhage under high pressure, leading to pia arachnoid rupture and extravasation of blood into the subdural space10,11). In the absence of trauma and any predisposing conditions, subdural bleeding might instead result from a sudden increase in intravenous pressure, which can occur when forcible exhalation occurs against a closed glottis, for example, during the Valsalva maneuver or during coughing or defecation, but also while blowing. Brennan et al.2) presented a spontaneous subdural hematoma in a 37-year-old male marathon runner. They supposed that weight training, which could potentially cause subdural hematoma throught generation of valsalva maneuver. In our patient, she had been playing the flute for several months as a student of music. Non-invasive measurements have identified a rise in intraocular pressure reflecting increased intravenous under these conditions4,9). Jacome and Yanez6) also described a patient with spontaneous SDH apparently produced by straining while lifting a heavy weight. They proposed that the rupture of bridging dural veins while performing the valsalva maneuver on heavy lifting caused the bleed. Intracranial hypotension, another risk factor for spontaneous subdural hemorrhage, can occur following exercise, as bouts of submaximal dynamic exercise result in systemic vascular hypotension3). In one study, systolic blood pressure was found to reduce by 20 mm Hg at 10 min after exercise7). Intracranial hypotension can also be secondary to systemic hypotension resulting from a loss of circulating blood volume, such as, that accompanying dehydration. However, our patient was not clinically dehydrated on admission and had normal renal functions. Nevertheless, it is possible that an episode of acute and transient dehydration while exercising resulted in intracranial hypotension and precipitated a subdural hematoma. The onset of symptoms in our case was insidious and definitely not that usually described as rapid or sudden for acute spontaneous subdural hematoma in older patients. The investigation modality of choice is CT, which allows the diagnosis to be made out promptly. Cerebral angiography is needed to exclude vascular abnormalities, such as, dural arteriovenous malformations and fistulas. Coagulation abnormalities can be excluded by coagulation profiles. The prognosis for subdural hematoma is mainly dependent on preoperative neurological state regardless of its origin or cause. Therefore, the outcome of chronic subdural hematoma following prompt surgical evacuation should be good.
References
1. Avis SP. Nontraumatic acute subdural hematoma. A case report and review of the literature. Am J Forensic Med Pathol. 1993; 14:130–134. PMID: 8328432.
2. Brennan PM, Fuller E, Shanmuganathan M, Keston P, Fouyas I. Spontaneous subdural haematoma in a healthy young male. BMJ Case Rep. 2011; doi: 10.1136/bcr.01.2011.3694.

3. de Noronha RJ, Sharrack B, Hadjivassiliou M, Romanowski CA. Subdural haematoma : a potentially serious consequence of spontaneous intracranial hypotension. J Neurol Neurosurg Psychiatry. 2003; 74:752–755. PMID: 12754345.

4. Haykowsky MJ, Eves ND, R Warburton DE, Findlay MJ. Resistance exercise, the Valsalva maneuver, and cerebrovascular transmural pressure. Med Sci Sports Exerc. 2003; 35:65–68. PMID: 12544637.

5. Hesselbrock R, Sawaya R, Means ED. Acute spontaneous subdural hematoma. Surg Neurol. 1984; 21:363–366. PMID: 6701770.

6. Jacome DE, Yanez GF. Subdural haematoma upon straining. J Neurol Neurosurg Psychiatry. 1989; 52:134. PMID: 2709028.

7. MacDonald JR, MacDougall JD, Interisano SA, Smith KM, McCartney N, Moroz JS, et al. Hypotension following mild bouts of resistance exercise and submaximal dynamic exercise. Eur J Appl Physiol Occup Physiol. 1999; 79:148–154. PMID: 10029335.

8. Marconi F, Fiori L, Parenti G, Ravelli V. Acute spontaneous subdural haematoma. Description of four clinical cases. J Neurosurg Sci. 1991; 35:97–102. PMID: 1757810.
9. Schuman JS, Massicotte EC, Connolly S, Hertzmark E, Mukherji B, Kunen MZ. Increased intraocular pressure and visual field defects in high resistance wind instrument players. Ophthalmology. 2000; 107:127–133. PMID: 10647731.

10. Sung SK, Kim SH, Son DW, Lee SW. Acute spontaneous subdural hematoma of arterial origin. J Korean Neurosurg Soc. 2012; 51:91–93. PMID: 22500200.

11. Tokoro K, Nakajima F, Yamataki A. Acute spontaneous subdural hematoma of arterial origin. Surg Neurol. 1988; 29:159–163. PMID: 3276025.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download