Abstract
Objective
Neuroendoscopy is applied to various intracranial pathologic conditions. But this technique needs informations for the anatomy, critically. Neuronavigation makes the operation more safe, exact and lesser invasive procedures. But classical neuronavigation systems with rigid pinning fixations were difficult to apply to pediatric populations because of their thin and immature skull. Electromagnetic neuronavigation has used in the very young patients because it does not need rigid pinning fixations. The usefulness of electromagnetic neuronavigation is described through our experiences of neuroendoscopy for pediatric groups and reviews for several literatures.
Methods
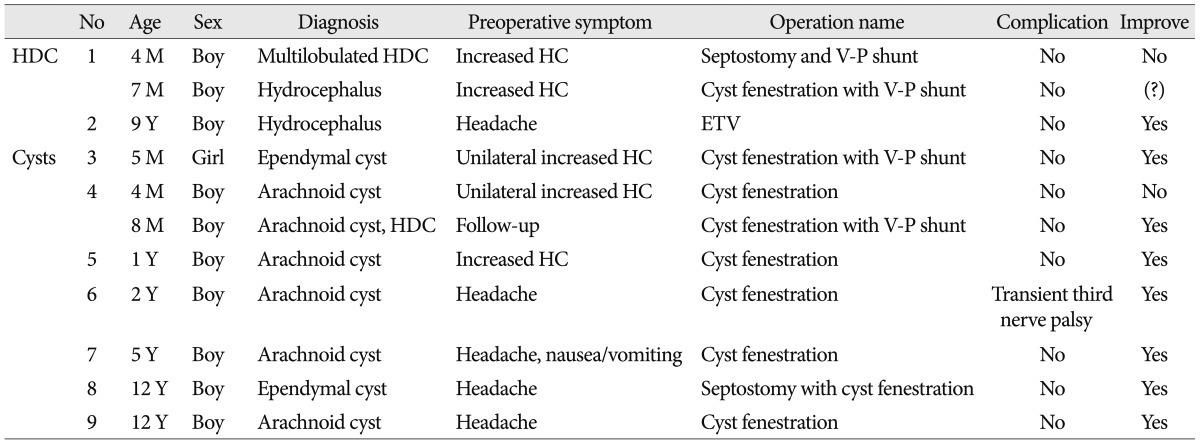
Between January 2007 and July 2011, nine pediatric patients were managed with endoscopic surgery using electromagnetic neuronavigation (AxiEM, Medtronics, USA). The patients were 4.0 years of mean age (4 months-12 years) and consisted of 8 boys and 1 girl. Totally, 11 endoscopic procedures were performed. The cases involving surgical outcomes were reviewed.
Results
The goal of surgery was achieved successfully at the time of surgery, as confirmed by postoperative imaging. In 2 patients, each patient underwent re-operations due to the aggravation of the previous lesion. And one had transient mild third nerve palsy due to intraoperative manipulation and the others had no surgery related complication.
The neuronavigation had proven to be a great device for the surgical treatment of variable neurosurgical problems such as tumor resection or biopsy, the surgery for epilepsy, vascular neurosurgery, the localization of functional and eloquent area, spinal neurosurgery and the operation for hydrocephalus9,13,16,17). Because the device helps the identification of pathologic condition and intraoperative anatomy distorted by pathologic anatomic conditions, the application of this device makes the operations more exact, safe, fast and less invasive due to finding the way and avoiding collision16,17).
The endoscopic surgery in pediatric patients can also be applied to the some operations such as shunt for the hydrocephalus, the fenestration for the cystic lesion and the biopsy or resection of intraventricular and periventricular lesions. But the pathologic condition distorts the normal anatomy, so the operator confuses normal anatomical structures in small endoscopic surgical view. For these difficulties, the neuronavigation can allow the safe procedure of neuroendoscopy in pediatric patients13).
The pinless electromagnetic (EM) image-guided neuronavigation has expanded the application of neuronavigation in intracranial neurosurgery, because the other neuronavigation systems needed the rigid pinning cranial fixation, these techniques were not always suitable for very young patients13). This fact supports that pinless EM neuronavigation can be useful for pediatric neurosurgery. In addition, some reported that this device has proven to be successful in pediatric patients17,18).
In this study, the usefulness of EM neuronavigation is described with the review for the neuroendoscopic surgery in 11 pediatric surgical cases in one institute.
Between Jan. 2007 and Jul. 2011, nine pediatric patients (8 boys and 1 girl) were managed with endoscopic surgery using pinless EM neuronavigation (AxiEM, Medtronics, USA). The age of the patients ranged from 4 months to 12 years (mean age: 4.0 years old). A total of 11 neuroendoscopic procedures on 9 patients with cystic lesions (7 patients) and hydrocephalus (2 patients) were performed. The cystic lesions consisted of five arachnid cysts and two ependymal cysts. In two hydrocephalus, one patient had an obstructive hydrocephalus due to an aqueductal stenosis by a tectal glioma and the other had the multi-loculated hydrocephalus caused by ventriculitis and ventricular abscess. The clinical signs and symptoms were increased head circumference, headache or the prematurity (Table 1).
Preoperative CT or MRI with ten fiducial markers on scalp was performed for neuronavigation. The equipment required for the procedures comprises the Stealth Station AxiEM neuronavigation system. Then the registration with fiducial markers and EM stylets was performed. With the guidance of neuronavigation, the endoscopic surgery was performed. All operations were performed by one neurosurgeon in one institute. The clinical outcome of the procedure was evaluated by improvements of symptoms and sign and the postoperative radiologic study.
On classical optical neuronavigation with rigid pinning cranial fixation, preoperative MRI or CT was performed with several fiducial markers (Fig. 1A) which were attached on patient's head (scalp and/or face). In the operation room (OR), the patient's head was fixed with rigid pinning fixation such as Mayfield frame (Fig. 1B). Then navigation system was set up. The preoperative navigation-image was transported to the navigation workstation in OR and reconstructed to 3-dimensional image. And then the position of the infra-red camera was controlled to recognize the reference frame and navigation pointer. After that, the image was registered with navigation pointer (Fig. 1C) and each fiducial marker between that of patient and images. At the end of the registration, the fiducial markers on patient's scalp were removed and the surgery started.
On pinless and frameless neuronavigation, adhesive tape replaces rigid pinning fixation as the fixation of head. The other process is same to classical system.
And on electromagnetic neuronavigation, this system does not fix the head. The patient's head was put on the gelly head ring and electromagnetic coil was installed around head (Fig. 2A). Then adhesive-based scalp array was used (Fig. 2B). The thin and flexible stylet (Fig. 2C) replaces thicker and rigid navigation pointer. The other process is same to other systems.
All procedures were performed with using of EM neuronavigation and not interfered by any magnetic devices during navigation. The operations consisted of the fenestration and the cerebrospinal fluid (CSF) diversion. The fenestration was performed for the cystic lesion and made on the cystic wall for communication to cistern and/or ventricle. The CSF diversion was performed for the patients suffered with hydrocephalus and included shunt operation, third ventriculostomy and septostomy. The combined procedures were performed at the same time in some cases. In author's study, the fenestration was used in 8 cases and the CSF diversion in 6 cases.
In all cases, the goal of surgery was accomplished successfully at the time of surgery, as confirmed immediately by postoperative imaging with the check of multiple pneumocephalus as the evidence of communication between the lesion and other space such as cistern or ventricle. Surgery related intraoperative problems such as error of the surgical trajectory, the CSF leakage, infection and the injury of neurovascular structures were not occurred in all patients. And postoperative permanent neurological complication was not occurred (Table 1).
One patient (case 6) had mild third nerve palsy due to manipulation intraoperatively and that was transient. The imaging study for postoperative status and follow-up showed the improvement and the stabilization of the lesion in 7 cases. In 2 cases, postoperative follow up imaging studies within 6 months revealed the aggravation of the lesions. So each patient needed second operation. All patients have the improvement of preoperative symptom and normal development except one baby who was transferred to the other hospital during follow up on out-patient department.
A 4-month-old male infant visited to the hospital due to incidentally detected intracranial cystic lesion. The baby was born with 2820 gram body weight at 38 weeks 5 days of gestation. The cystic lesion was detected on prenatal ultrasonography and the size enlarged on follow up examination. Brain MRI demonstrated about 8 cm sized interhemispheric multiloculated cystic lesion without enhancement and associated hypogenesis of corpus callosum, right lateral ventricular dilatation (Fig. 3A). The baby underwent endoscopic cystic wall fenestration at multiple sites and insertion external ventricular drainage (EVD) catheter in the cyst. Postoperative brain CT showed decreased size of the cyst and subdural hygroma on bilateral frontoparietal region (Fig. 3B). The baby discharged without any neurologic problem. But the cyst was enlarged again with the aggravation of ventriculomegaly on postoperative imaging study of 3 months (Fig. 3C). Therefore, the endoscopic cyst fenestration and ventriculoperitoneal shunt was performed because the function of CSF circulation might be impaired. The size of cyst and ventricle decreased and the brain mantle has gotten thicker (Fig. 3D). The boy has grown with normal development.
A 2-year-old boy visited with the complaint of prolonged headache after slipping down. On neurological examination, there was no specific finding. Brain CT showed about 6.5 cm sized cystic lesion on the right middle cranial fossa with midline shifting to the left side by 7 mm (Fig. 4A). The neuroendoscopic cyst fenestration with the guidance of EM neuronavigation and the insertion of EVD catheter were performed. The postoperative brain CT showed multiple pneumocephalus on cisterns around brain stem and cyst. The boy discharged with the removal of EVD catheter and mild ptosis and medial gaze limitation on right eye. On the follow-up on out-patient department, the symptom improved and the size of the cyst decreased (Fig. 4B).
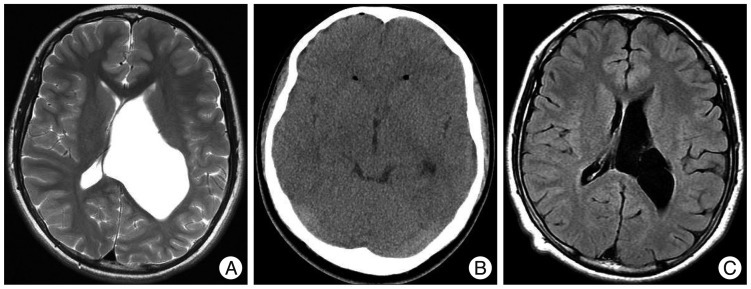
A 12-year-old boy visited to the hospital due to intermittent syncope and headache. There was no abnormal finding on neurological examination, on past history and on other examination such as electrocardiography. However, brain MRI demonstrated about 8 cm sized cystic lesion on antrum of left lateral ventricle without hydrocephalus (Fig. 5A). He underwent pinless EM image-guided neuroendoscopic septostomy and ventriculo-cystostomy through a right postcoronal burr hole on prone position. Postoperative brain CT demonstrated pneumocephalus on frontal horn of both lateral ventricles without any acute hemorrhagic or ischemic lesion (Fig. 5B). Postoperative neurologic examination was non-specific. On follow-up, the size of cyst had decreased (Fig. 5C) and symptom improved.
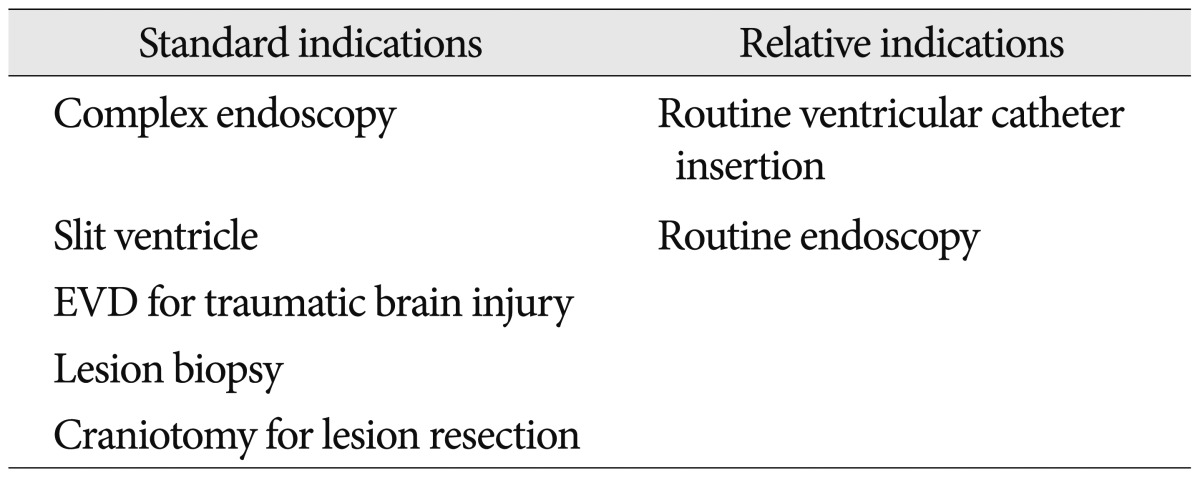
The neuroendoscopy has used since 1922 by Dandy1) and the appliance of endoscopy are variable in neurosurgical area22) : the biopsy or resection of intraventricular or periventricular lesion, third ventriculostomy, cyst fenestration for arachnoid or ependymal cyst, aqueductal stenosis, multilobulated hydrocephalus and the insertion of intraventricular catheter such as shunt proximal tip and Ommaya reservoir etc. This procedure requires exact anatomic orientation for every step of the operation due to narrow surgical view. In addition, variable pathologic anatomical changes add the difficulty in endoscopic surgery17,18). However, this procedure had relative high complication rate that reported up to 20%6,14,17,19,22) : the neurovascular injury, CSF leakage and infection, seizure and subdural fluid collection (Table 2). And Abtin et al.1) and Navarro et al.14) reported the discontinuation of the procedure due to the lack of anatomical landmark with distorted intracranial anatomy in several cases.
After the appliance of the neuronavigation makes the neurosurgical procedures more safe and easy, so it can help to reduce the complication and morbidity and improve outcome in neurosurgical procedures13,17) (Table 2). And the appliance of the neuronavigator helps the operator understand the orientation of distorted anatomy and blind areas over the septum and the cystic wall20). But the classical optical neuronavigation with rigid cranial fixation has some limitations for the application. The fixation has a risk of scalp laceration, skull fracture, extradural hemorrhage and intracranial injury13,17). In addition, the pain involved in using the fixation cause the increased use of anesthetic agents and the increased operation time7). The rigid pinning makes that the appliance to children with thin and immature skull is especially difficult. Therefore, the advance of pinless neuronavigation can lead to an increase in its range of uses in several neurosurgical conditions including pediatrics17). But this system does not solve the limitation of the operator's motion and that of the head fixation with adhesive tape.
EM neuronavigation leads to be non-invasive due to the use without rigid pinning cranial fixation and with free head motion on the operation. Due to non-invasiveness, the system can apply to very young pediatric patients who have very thin and immature skull. This advantage makes lower limitation of the application neuronavigation in age. As shown Table 2, the age in which neuroendoscopic surgery was performed is lower in EM neuronavigation than in classical neuronavigation. The system needs shorter time for set-up and registration compared with previous neuronavigation system. In addition, it allows head movement at any time after registration with no restriction on the freedom of movement of instruments within the surgical field and does not limit the operator motion due to no need of optical line between the pointer, reference frame, and the infrared camera. Also, the operation using neuronavigation can be performed under local anesthesia due to no fixation with pinning frame9,11,13,15-17,21). In an author's case, which was 5 months baby with congenital hydrocephalus, this device was very useful to decide the proper trajectory for proximal shunt tip with the change of head position after registration.
Several operators reported the appilication of EM neuronavigation on neuroendoscopic surgery in variable conditions3,7,9,13,17). McMillen et al.13) applied EM neuronavigation in 13 months children who had obstructive hydrocephalus caused by cystic hypothalamic glioma. In the case, neuroendoscopic surgery for shunt and cyst fenestration was performed in two different surgical points with head reposition without accuracy changes. In this study, the patient (case 1) had post-infectious multiloculated hydrocephalus and needed multiple fenestrations for multiple cystic walls. The decision for the site to fenestrate was difficult, because the loculated walls were not defined exactly and not discriminated clearly from normal ventricular walls, in addition, normal anatomy was distorted. The patient's age was too young, 4 months. EM neuronavigation without rigid pinning fixation was able to been applied for endoscopic surgery usefully and successfully.
Hayhurst et al.9) suggested some indications for appliance of EM neuronavigation in neurosurgical procedures (Table 3). Among them, the EM neuronavigation had additional several usefulness in neuroendoscopy with the advantage of previous system as follows2,8,9,13,16,17,23) : 1) The control of probe's depth due to the flexibility of the probe is feasible. 2) This system allows to be passed through the endoscope working channel for use in fenestration of both arachnoid and floor of the third ventricle on the tip of the endoscope. 3) This leads to fewer requirements for changing instruments and maneuvering to endoscope. 4) The handling of endoscope containing EM probe is not difficult due to a character of weightless stylet. 5) If the endoscope needed to be repositioned, the navigation stylets could easily be replaced in the endoscope's working channel to confirm the location of the tip of the instrument. 6) The additional procedure with head reposition can be performed without distortion of preoperative registration.
But this system had some disadvantages. The navigation devices such as probe and tracer were disposable and expensive, and some authors reported that the accuracy for application is lower than other system. Navigation system is distorted by external magnetic signals and lack of variety for devices. In addition, it has the risk of loss of sterility and unsuspected injury in awaken procedures due to not rigidity fixation9,17,21).
However, those disadvantages were not able to interfere the usage of EM navigation. Some authors reported that the EM neuronavigation in the insertion of the shunt proximal catheter insertion can be worthier than the cost of stylets because the costs for revision and/or complications which caused by not using EM neuronavigation might be higher than the cost for usage of EM neuronavigation7,9). In addition, Rosenow and Sootsman15) and Mascott12) reported that application accuracy of EM neuronavigation is not lower than optical navigation. Magnetic interference is not any problem because of using standard instruments7).
The usefulness of EM neuronavigation in neuroendoscopy has been reported and proven by several authors and cases. This technique in 9 pediatric patients who were younger than 12 year-old showed successful surgical management in this study, however, there were too small cases to prove usefulness of EM neuronavigation compared with other authors. But this result of operations is similar with others and can be supports for usage of EM neuronavigation and help prove usefulness of EM neuronavigation in neuroendoscopic surgery.
The appliance of the neuronavigation reduces the complication rate and enhances for the indication of the neuroendoscopic surgery. But the use of classical optical neuronavigation which needs rigid pinning fixations has been limited in several situations such as pediatrics with immature skull. EM neuronavigation, in this aspect, solved that problem without using rigid pinning fixation. In conclusion, it can be a useful device and alternative to a classical optical neuronavigation in the pediatric neuroendoscopic surgery.
References
1. Abtin K, Thompson BG, Walker ML. Basilar artery perforation as a complication of endoscopic third ventriculostomy. Pediatr Neurosurg. 1998; 28:35–41. PMID: 9693328.

2. Aldana PR, Kestle JR, Brockmeyer DL, Walker ML. Results of endoscopic septal fenestration in the treatment of isolated ventricular hydrocephalus. Pediatr Neurosurg. 2003; 38:286–294. PMID: 12759507.

3. Barszcz S, Roszkowski M, Daszkiewicz P, Jurkiewicz E, Maryniak A. Accuracy of intraoperative registration during electromagnetic neuronavigation in intracranial procedures performed in children. Neurol Neurochir Pol. 2007; 41:122–127. PMID: 17530573.
4. Beems T, Grotenhuis JA. Long-term complications and definition of failure of neuroendoscopic procedures. Childs Nerv Syst. 2004; 20:868–877. PMID: 15197569.

5. Buxton N, Macarthur D, Mallucci C, Punt J, Vloeberghs M. Neuroendoscopy in the premature population. Childs Nerv Syst. 1998; 14:649–652. PMID: 9840365.

6. Cinalli G, Spennato P, Ruggiero C, Aliberti F, Trischitta V, Buonocore MC, et al. Complications following endoscopic intracranial procedures in children. Childs Nerv Syst. 2007; 23:633–644. PMID: 17447074.

7. Clark S, Sangra M, Hayhurst C, Kandasamy J, Jenkinson M, Lee M, et al. The use of noninvasive electromagnetic neuronavigation for slit ventricle syndrome and complex hydrocephalus in a pediatric population. J Neurosurg Pediatr. 2008; 2:430–434. PMID: 19035692.

8. Hamada H, Hayashi N, Kurimoto M, Endo S. Endoscopic aqueductal stenting via the fourth ventricle under navigating system guidance : technical note. Neurosurgery. 2005; 56(1 Suppl):E206. discussion E206. PMID: 15799817.
9. Hayhurst C, Byrne P, Eldridge PR, Mallucci CL. Application of electromagnetic technology to neuronavigation : a revolution in image-guided neurosurgery. J Neurosurg. 2009; 111:1179–1184. PMID: 19326991.

10. Hopf NJ, Grunert P, Darabi K, Busert C, Bettag M. Frameless neuronavigation applied to endoscopic neurosurgery. Minim Invasive Neurosurg. 1999; 42:187–193. PMID: 10667823.

11. Lancon JA, Killough KR, Dhillon G, Parent AD. Interventional magnetic resonance imaging guided aspiration and biopsy of a cystic midbrain tumor. Pediatr Neurosurg. 1999; 30:151–156. PMID: 10352419.

12. Mascott CR. Comparison of magnetic tracking and optical tracking by simultaneous use of two independent frameless stereotactic systems. Neurosurgery. 2005; 57(4 Suppl):295–301. discussion 295-301. PMID: 16234678.

13. McMillen JL, Vonau M, Wood MJ. Pinless frameless electromagnetic image-guided neuroendoscopy in children. Childs Nerv Syst. 2010; 26:871–878. PMID: 20076987.

14. Navarro R, Gil-Parra R, Reitman AJ, Olavarria G, Grant JA, Tomita T. Endoscopic third ventriculostomy in children : early and late complications and their avoidance. Childs Nerv Syst. 2006; 22:506–513. PMID: 16404640.

15. Rosenow JM, Sootsman WK. Application accuracy of an electromagnetic field-based image-guided navigation system. Stereotact Funct Neurosurg. 2007; 85:75–81. PMID: 17167235.

16. Roth J, Beni-Adani L, Biyani N, Constantini S. Classical and real-time neuronavigation in pediatric neurosurgery. Childs Nerv Syst. 2006; 22:1065–1071. PMID: 16761161.
17. Sangra M, Clark S, Hayhurst C, Mallucci C. Electromagnetic-guided neuroendoscopy in the pediatric population. J Neurosurg Pediatr. 2009; 3:325–330. PMID: 19338413.

18. Scholz M, Hardenack M, Konen W, Fricke B, von During M, Heuser L, et al. Navigation in neuroendoscopy. Minim Invasive Ther Allied Technol. 1999; 8:309–316.

19. Schroeder HW, Oertel J, Gaab MR. Incidence of complications in neuroendoscopic surgery. Childs Nerv Syst. 2004; 20:878–883. PMID: 15185113.

20. Schroeder HW, Wagner W, Tschiltschke W, Gaab MR. Frameless neuronavigation in intracranial endoscopic neurosurgery. J Neurosurg. 2001; 94:72–79. PMID: 11147902.

21. Sieśkiewicz A, Łysoń T, Mariak Z, Rogowski M. [Neuronavigation in transnasal endoscopic paranasal sinuses and cranial base surgery comparison of the optical and electromagnetic systems]. Otolaryngol Pol. 2009; 63:256–260. PMID: 19886532.
22. Teo C, Rahman S, Boop FA, Cherny B. Complications of endoscopic neurosurgery. Childs Nerv Syst. 1996; 12:248–253. discussion 253. PMID: 8737800.

23. Wagner W, Gaab MR, Schroeder HW, Sehl U, Tschiltschke W. Experiences with cranial neuronavigation in pediatric neurosurgery. Pediatr Neurosurg. 1999; 31:231–236. PMID: 10681676.

Fig. 1
A : Fiducial markers. B : Mayfield frame as pinning fixation system. C : The setting of classical optical neuronavigation (0 : patient's head, 1 : infra-red camera, 2 : navigation pointer, 3 : reference frame).

Fig. 3
A : A 8 cm sized interhemispheric multiloculated cystic lesion with hypogenesis of corpus callosum, right lateral ventricular dilatation on brain MRI (T2WI). B : Postoperative brain CT shows multiple pneumocephalus and decreased size of the cyst. C : Follow up brain MRI (T2WI) shows increased cyst compared with postoperative brain CT. D : Last follow up brain CT shows decreased cyst with inserted shunt proximal tip. T2WI : T2-weighted image

Fig. 4
A : A 6.5 cm sized cyst on right temporal lobe on brain CT. B : Last postoperative follow up brain CT shows that the cystic lesion disappeared completely.
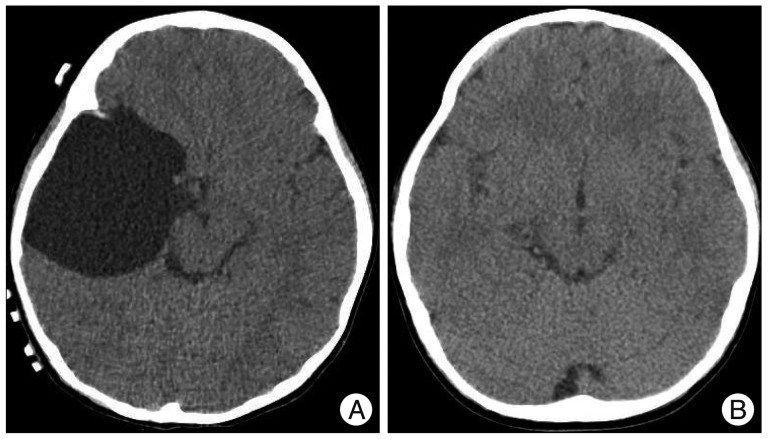
Fig. 5
A : A 8 cm sized cystic lesion on left lateral ventricle on brain MRI (T2WI). B : Postoperative brain CT shows pneumocephalus on frontal horn on both lateral ventricles. C : Last follow up brain MRI (FLAIR) show decreased cystic lesion. T2WI : T2-weighted image.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download