Abstract
Objective
The introduction and development of the embolic protecting device (EPD) has resulted in a decreased rate of stroke after carotid artery stenting (CAS). The authors performed a retrospective study to investigate the risk factors for developing large emboli after CAS which can lead to ischemic events.
Methods
A total of 35 consecutive patients who underwent CAS between January 2009 and March 2012 were included in this study. Patients were divided into two groups including those with small emboli (group A; grade 1, 2) and those with large emboli (group B; grade 3, 4). The size and number of emboli were assigned one of four grades (1=no clots, 2=1 or 2 small clots, 3=more than 3 small clots, 4=large clots) by microscopic observation of the EPD after CAS. We compared demographic characteristics, medical history, and angiographic findings of each group.
Results
Thirty-five patients underwent CAS, and technical success was achieved in all cases. Twenty-three patients were included in group A and 12 patients in group B. Our results demonstrated that advanced age [odds ratio (OR) 1.24; 95% confidence interval (CI) 1.01-1.52; p=0.044] and smoking (OR 42.06; CI 2.828-625.65, p=0.006) were independent risk factors for developing large emboli after CAS.
Carotid occlusive disease is one of the most frequently identified and treatable causes of ischemic stroke. Currently, carotid endarterectomy (CEA) and carotid artery stenting (CAS) are recognized as the two leading treatments of carotid atherosclerotic stenosis13). Although CEA is the gold standard for treatment of carotid artery stenosis, CAS has evolved as a potential alternative to CEA due to its minimal invasiveness6).
The introduction of the embolic protecting device (EPD) has resulted in a decreased rate of ischemic stroke after CAS5). Recently, however, several reports failed to show a benefit of using an EPD during CAS for reducing ischemic stroke. Wu et al.20) assigned 76 patients with carotid artery stenosis to undergo CAS procedures with or without an EPD. Their results showed that the incidence of newly detected ischemic lesions on magnetic resonance diffusion-weighted images (DWI) between the two groups were not significantly different. Furthermore, complications of EPD use such as difficult retrieval, vasospasm, and vessel dissection have called into question the efficacy of protecting devices13). Therefore, it seems necessary to identify whether the EPD use during CAS is valid or not. In this study, we digitized size and number of emboli captured by EPD during CAS, predict the risk factors for developing large emboli that may cause ischemic stroke.
A retrospective single-center review of 35 consecutive patients who underwent CAS under the protection of an EPD between January 2009 and March 2012 was conducted. The inclusion criteria for patients who underwent CAS were symptomatic carotid artery stenosis >50% or asymptomatic stenosis >70%. Patients who suffered acute cerebral infarction typically underwent CAS 3 weeks after the initial event. We reviewed patient characteristics, medical records, angiographic findings, postoperative DWI, and size and number of emboli captured by the EPD during the procedure.
Patients received oral aspirin (100 mg) and clopidogrel (75 mg) daily for a minimum of 7 days prior to the procedure. Stent placement was performed under local anesthesia by a neuroradiologist and a neurosurgeon. At the beginning of the procedure, patients received an intravenous bolus injection of 3000 U heparin. An intermittent bolus of 1000 U heparin was given at 1-hour intervals thereafter.
A 6 F Shuttle (Cordis, Miami, FL, USA) was placed in the common carotid artery. Activated coagulation time was not routinely monitored. Under roadmap guidance, the stenotic lesion was crossed using a 0.014 inch guidewire. An Angioguard (Cordis, Miami, FL, USA) as a EPD was subsequently positioned distal to the stenotic lesion. The EPD was advanced without the aid of pre-dilatation in all lesions. Pre-stenting dilatation with a balloon was subsequently performed within the stenotic lesion after placement of the EPD. The size of the balloon was chosen to be approximately 80% of the normal diameter of the distal internal carotid artery. We positioned the balloon covering the stenotic segment in a monorailed type and inflated the balloon gradually once in most cases while monitoring vital signs. We used Precise (Cordis, Miami, FL, USA) stents in each case. The size of stent was chosen as the diameter of just proximal to stenotic segment. Post-stenting balloon angioplasty was not routinely performed unless significant residual stenosis (>40%) was found on immediate post-stenting angiography. DWI was performed 1 day after stent placement in most patients.
Digital subtraction angiographic images were collected and analyzed retrospectively. Angiographic lesion characteristics were recorded and defined as follows :
- Rates of stenosis were measured using the North American Symptom Carotid Endarterectomy Trial criteria, with the distal internal carotid serving as the reference segment.
- Lesion length was defined as the distance between the start and end of the stenotic segment. Only portions with >50% stenosis were quantified.
- Ulceration of plaques was defined as a crater extending from the lumen into the stenotic plaque15).
- Calcification was noted as radiologic densities readily seen within the apparent vascular wall of the artery.
- Lateral carotid angle was measured as the angle between the distal common carotid artery and the proximal ICA (Fig. 1).
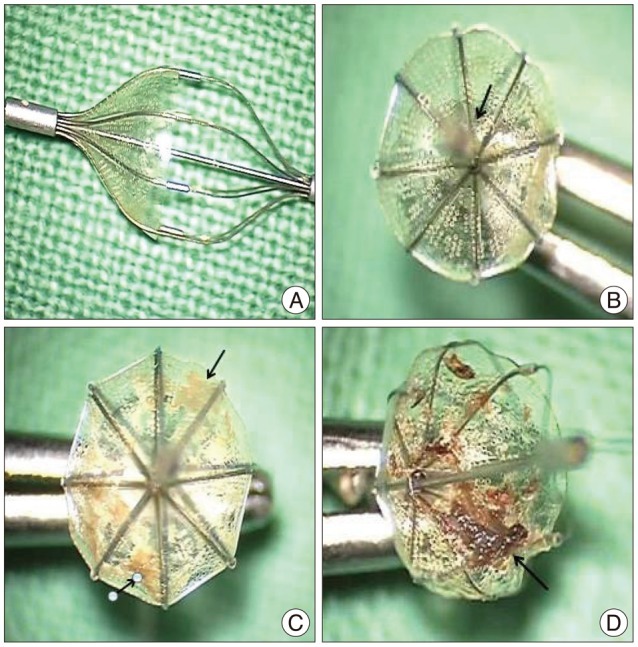
We used an EPD in all CAS procedures and digitized the captured emboli. The size and number of emboli were classified using four grades (1=no clots, 2=1 or 2 small clots, 3=more than 3 small clots, 4=large clots) by observation of the EPD after CAS using operating microscope (Möller 20-1000, Made in Germany) (Fig. 2). Large clots were defined as >2 mm in size. All patients were divided into two groups including patients with small emboli (group A) and patients with large emboli (group B). General characteristics, medical comorbidities including history of smoking, alcohol use, hypertension, diabetes, atrial fibrillation, other cardiac problems, and angiographic findings including rate of stenosis, lesion length, lateral carotid angle, ulceration, and calcification were compared between groups.
Data were analyzed using SAS (version 9.2, SAS Institute, Inc.). Continuous variables were analyzed using Wilcoxon rank-sum tests and categorical variables analyses were done using chi-squared tests and Fisher's exact tests. All p-values <0.05 were considered to be statistically significant.
During the study period, 35 patients were hospitalized for carotid artery occlusion, all of whom underwent CAS. Among them, 30 patients underwent post-operative DWI. During the CAS procedure, an EPD was used in all cases, each of which was successfully deployed with no EPD related complications. Emboli were detected in 17 of 35 patients.
Captured emboli were digitized and classified using 4 grades (group A : grades 1 and 2, group B : grades 3 and 4). A total of 23 patients were included in group A (grade 1 : 16 cases, grade 2 : 7 cases), and 12 patients were included in group B (grade 3 : 5 cases, grade 4 : 7 cases). Univariate logistic regression analysis of risk factors for large emboli during CAS in both groups are summarized in Table 1. Patients in groups A and B were similar with respect to mean age, sex, and pre-existing comorbidities. The mean ages at the time of intervention were 67.74 (group A) and 71.25 (group B) years. The majority of patients (78.3% of group A, 91.7% of group B) in both groups were male. Incidences of pre-morbid hypertension (69.6% versus 50%), diabetes (43.5% versus 58.3%), and atrial fibrillation (4.4% versus 8.3%) were similar in groups A and B, respectively. Pre-morbid medical conditions such as previous stroke (18.2% versus 25%), previous myocardial infarction (MI, 18.2% versus 8.3%), and hypercholesterolemia (4.4% versus 16.7%), as well as pre-operative cardiac morbidity such as MI (4.4% versus 8.3%), angina pectoris (26.1% versus 0%), arrhythmia (0% versus 8.3%), and heart failure (0% versus 0%) were not significantly different between groups A and B, respectively.
Patients in group B were more likely to smoke (13% versus 58.3%) than patients in group A (p=0.0106). Alcohol use (47.8% versus 58.3%) was not different between the two groups.
Twelve patients (52.2%) in group A and 8 patients (66.7%) in group B underwent intervention on the right ICA. Mean rates of stenosis were 78.96% for group A and 76.08% for group B. Measured lesion length was longer in group B (19.23±8.81 mm) than group A (13.93±6.44 mm), but this difference was not statistically significant. The lateral carotid angle (144.48±16.72° versus 148.25±19.0°) and presence of calcification (47.8% versus 75%) were not significantly different in groups A and B, respectively, but ulcerations (21.7% versus 66.7%) were a highly meaningful risk factor for large emboli (p=0.0160). Postoperative DWI signal change was seen in 9 patients (39.13%) in group A and 9 patients (75.0%) in group B.
Univariate analysis showed that smoking and plaque ulcerations were associated with an increased risk of forming large emboli during CAS. Although the length of the lesions in group B were much longer than that of group A, this difference was not statistically significant (Table 1). In addition to these three factors, age which seemed to be relatively associated was also included in the multivariate analysis (Table 2).
Multivariate analysis showed that age (p=0.0448) and smoking (p=0.0066) were independent predictors of the development of large emboli during the stenting procedure, whereas lesion length did not fulfill the statistical significance. Furthermore, while plaque ulceration was a significant factor on univariate analysis, it lost the significance on multivariate analysis.
Strokes most frequently result from acute cerebral ischemia, 20% of which are due to atherosclerotic occlusive disease of the carotid artery19). While CEA is considered to be the gold standard surgical treatment of carotid occlusive disease22), CAS is a valid alternative to CEA for experienced physicians treating patients with carotid artery stenosis due to the relative ease of placement and popularity of minimally invasive procedures8,10,21). One limitation of CAS is the potential for embolic stroke caused by atheroembolic material released from the carotid plaque during the procedure. In several studies which were largely performed without the use of any cerebral protection, stroke occurred in over 10% of patients7,14,18). Recently, EPDs have been more routinely used during CAS, and thromboembolic complications have been significantly reduced5,11). The clinical efficacy and safety of EPDs are still controversial, however, due to an increased risk of arterial vasospasm, thrombosis, and dissection4). Moreover, some studies have reported that CAS alone without cerebral protection is enough to treat patients who have symptomatic or asymptomatic carotid artery stenosis, and that the rate of ischemia is not significantly different from patients in which an EPD was used3,20).
While many researchers suggest that cerebral protection is necessary for preventing ischemic stroke based on DWI findings, no one has yet studied the risk factors for ischemia by examining the actual emboli captured by EPDs. We observed emboli microscopically after CAS and categorized patients into two groups based on the number and size of the emboli. The proximal middle cerebral artery (MCA) has a mean internal diameter of approximately 2.5 mm, and the distal MCA narrows to <2 mm16). Thus, emboli >2 mm in size could feasibly induce major cerebral infarction. Additionally, more than 3 small emboli (<2 mm in size) may be sufficient to cause obstruction of the distal MCA.
We identified advanced age and smoking as two risk factors significantly associated with the formation of emboli during carotid stenting. This study expanded on the existing knowledge of CAS-associated emboli and highlighted a unique opportunity for quality improvement in treatment of patients with carotid stenosis.
We hypothesized that patients with a history of smoking were more likely to have unstable plaques that were prone to distal embolization. Multiple studies have previously evaluated CAS-associated risk factors for peri-operative stroke. Maureen et al. evaluated 34 patients that underwent CAS found that new lesions were detected on DWI in 71% of patients. They also demonstrated that a history of coronary artery disease (CAD) was the only significant predictor of lesions seen on DWI. Smoking and personal history of hypertension, diabetes, or hyperlipidemia had no effect on the incidence of post-procedural stroke17). Conversely, a study at our institution showed smoking history as an independent risk factor for large emboli. CAD including myocardial ischemia and angina pectoris did not significantly contribute to the formation of emboli.
Some studies have reported that advanced age (>80 years) affects the incidence of post-procedural stroke. Gröschel et al.9) retrospectively reviewed records from 176 patients with carotid stenosis and found that advanced age, lesion length, and the presence of ulcerated lesions were independent risk factors for new lesions on DWI. Additional studies have highlighted the importance of long lesion length and the presence of ulcerative lesions. Sayeed et al.15) investigated angiography results of 421 patients who underwent CAS and found that lesions >15 mm in length are predictive of adverse outcomes. Additionally, Kastrup et al.12) identified that target lesion ulceration is associated with an increased incidence of CAS-associated ischemic stroke. We report similar results in the present study, in that patients with large emboli (group B) had longer lesions compared with patients with small emboli (group A) (19.23 mm versus 13.93 mm), though this difference was not statistically significant. The presence of ulcerated lesions seemed to correlate with large emboli on univariate logistic analysis (p=0.0160), though statistical significance was lost on multivariate analysis (p=0.1281).
Patients of advanced age, particularly those >80 years, often have more complex aortic arch morphology, arch calcification, and common carotid or ICA tortuosity than younger patients. These features can lead to poor outcomes by making the procedure itself more difficult, extending the procedure time, and damaging vessels that may make plaques more likely to form emboli1).
We expected that maneuvering through a longer, narrower region of stenosis would be more precarious than maneuvering through a shorter, wider lesion, though our results did not support it.
In our study, 51% of patients demonstrated evidence of postoperative, acute, cerebral microemboli on DWI. Bendszus et al.3) previously reported that among 100 interventional procedures performed, DWI showed new lesions in 23 patients. Our results showed a higher ischemic rate, though it is difficult to compare directly because our study was performed using a smaller sample size. In practice, many studies have revealed high rates of cerebral ischemia after procedure. Gröschel et al.9) reported that of 176 patients who had undergone protected CAS, 51% demonstrated new lesions on DWI. Likewise, Maureen et al. reported up to 70% of patients as having cerebral microemboli on DWI after CAS18).
We recognize that our study has several limitations. First, our data were analyzed retrospectively. In addition, the number of patients included in our study was rather small, which limits the statistical power to appropriately differentiate the relative importance of each risk factor studied. Finally, it was difficult to classify some cases that were grade 2 or 3 by microscopic observation of the EPD due to indistinct clot size or number.
The development of emboli is influenced by the vulnerable nature of atherosclerotic plaques and the degree of trauma applied to the endothelium during the CAS procedure. In our study, we investigated risk factors for destabilization of atherosclerotic plaques, making them more likely to induce cerebral infarction. Other anatomical factors such as aortic arch calcification, vessel tortuosity, and ostial involvement that can affect the development of emboli are currently being studied, and were not included in our analysis.
It is impossible to measure the degree of trauma that takes place during CAS objectively. It seems to be imperfect study as far as several anatomical variables are considered to the only factors that represent the degree of trauma. Furthermore, difference of proportion between rates of stenosis and balloon or stent size does influence the degree of trauma. As previously mentioned, however, the size of the balloon was chosen to be approximately 80% of the normal diameter of the distal internal carotid artery, and the stent was chosen as diameter of proximal part of stenotic segment, the rates of stenosis appeared to reflect the difference of proportion, instead.
Future studies in a large population are needed to identify peri-procedural risk factors including pre-operative symptoms, presence of contralateral stenosis, and other anatomical factors that were not analyzed in our study. In addition, analyzing whether new lesions detected on DWI are ipsilateral or contralateral to lesion would be useful.
CAS carries a known risk of post-procedure ischemic stroke. Our retrospective analysis of 35 patients showed that advanced age and smoking increased the number and size of emboli that developed during CAS. Although the use of EPDs is controversial, our results suggest that they may help to reduce the incidence of ischemic stroke after CAS in patients with risk factors for large emboli.
References
1. Bacharach JM, Slovut DP, Ricotta J, Sullivan TM. Octogenarians are not at increased risk for periprocedural stroke following carotid artery stenting. Ann Vasc Surg. 2010; 24:153–159. PMID: 19748765.

2. Baldi S, Zander T, Rabellino M, González G, Maynar M. Carotid artery stenting without angioplasty and cerebral protection : a single-center experience with up to 7 years' follow-up. AJNR Am J Neuroradiol. 2011; 32:759–763. PMID: 21349967.

3. Bendszus M, Koltzenburg M, Burger R, Warmuth-Metz M, Hofmann E, Solymosi L. Silent embolism in diagnostic cerebral angiography and neurointerventional procedures : a prospective study. Lancet. 1999; 354:1594–1597. PMID: 10560674.

4. Cardaioli P, Giordan M, Panfili M, Chioin R. Complication with an embolic protection device during carotid angioplasty. Catheter Cardiovasc Interv. 2004; 62:234–236. PMID: 15170718.

5. Castriota F, Cremonesi A, Manetti R, Liso A, Oshola K, Ricci E, et al. Impact of cerebral protection devices on early outcome of carotid stenting. J Endovasc Ther. 2002; 9:786–792. PMID: 12546579.

6. Chung J, Shin YS, Lim YC, Park SK. The clinical outcomes of 75 consecutive patients with cervical carotid artery stenosis treated by carotid artery stenting. J Korean Neurosurg Soc. 2009; 45:350–354. PMID: 19609418.

7. Diethrich EB, Ndiaye M, Reid DB. Stenting in the carotid artery : initial experience in 110 patients. J Endovasc Surg. 1996; 3:42–62. PMID: 8798126.
8. Dumont TM, Rughani AI. National trends in carotid artery revascularization surgery. J Neurosurg. 2012; 116:1251–1257. PMID: 22482791.

9. Gröschel K, Ernemann U, Schnaudigel S, Wasser K, Nägele T, Kastrup A. A risk score to predict ischemic lesions after protected carotid artery stenting. J Neurol Sci. 2008; 273:112–115. PMID: 18692206.

10. Gurm HS, Yadav JS, Fayad P, Katzen BT, Mishkel GJ, Bajwa TK, et al. Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med. 2008; 358:1572–1579. PMID: 18403765.

11. Kastrup A, Gröschel K, Krapf H, Brehm BR, Dichgans J, Schulz JB. Early outcome of carotid angioplasty and stenting with and without cerebral protection devices : a systematic review of the literature. Stroke. 2003; 34:813–819. PMID: 12624315.

12. Kastrup A, Gröschel K, Schnaudigel S, Nägele T, Schmidt F, Ernemann U. Target lesion ulceration and arch calcification are associated with increased incidence of carotid stenting-associated ischemic lesions in octogenarians. J Vasc Surg. 2008; 47:88–95. PMID: 18178458.

13. Lian X, Liu W, Li M, Lin M, Zhu S, Sun W, et al. Risk factors and complications associated with difficult retrieval of embolic protection devices in carotid artery stenting. Cardiovasc Intervent Radiol. 2012; 35:43–48. PMID: 21387123.

14. McDonnell CO, Fearn SJ, Baker SR, Goodman MA, Price D, Lawrence-Brown MM. Value of diffusion-weighted MRI during carotid angioplasty and stenting. Eur J Vasc Endovasc Surg. 2006; 32:46–50. PMID: 16546413.

15. Sayeed S, Stanziale SF, Wholey MH, Makaroun MS. Angiographic lesion characteristics can predict adverse outcomes after carotid artery stenting. J Vasc Surg. 2008; 47:81–87. PMID: 18178457.

16. Serrador JM, Picot PA, Rutt BK, Shoemaker JK, Bondar RL. MRI measures of middle cerebral artery diameter in conscious humans during simulated orthostasis. Stroke. 2000; 31:1672–1678. PMID: 10884472.

17. Tedesco MM, Coogan SM, Dalman RL, Haukoos JS, Lane B, Loh C, et al. Risk factors for developing postprocedural microemboli following carotid interventions. J Endovasc Ther. 2007; 14:561–567. PMID: 17696633.

18. Tedesco MM, Lee JT, Dalman RL, Lane B, Loh C, Haukoos JS, et al. Postprocedural microembolic events following carotid surgery and carotid angioplasty and stenting. J Vasc Surg. 2007; 46:244–250. PMID: 17600657.

19. Veith FJ, Amor M, Ohki T, Beebe HG, Bell PR, Bolia A, et al. Current status of carotid bifurcation angioplasty and stenting based on a consensus of opinion leaders. J Vasc Surg. 2001; 33(2 Suppl):S111–S116. PMID: 11174821.

20. Wu YM, Wong HF, Chen YL, Wong MC, Toh CH. Carotid stenting of asymptomatic and symptomatic carotid artery stenoses with and without the use of a distal embolic protection device. Acta Cardiol. 2011; 66:453–458. PMID: 21894801.

21. Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004; 351:1493–1501. PMID: 15470212.

22. Zarins CK. Carotid endarterectomy : the gold standard. J Endovasc Surg. 1996; 3:10–15. PMID: 8798120.
Fig. 2
Microscopic findings of the embolic protection devices after procedure. Arrows indicate the emboli captured. A : Grade 1. No emboli are visible. B : Grade 2. One small embolus is seen. C : Grade 3. Many clots not exceeding 3 mm are seen. D : Grade 4. Large clots over 3 mm are captured by the embolic protection device.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download