Abstract
Non-Hodgkin's lymphoma rarely originates from bone, and even more infrequently from a vertebral body. Lymphoblastic lymphoma is a rare type of non-Hodgkin's lymphoma, and results from an abnormality in adaptive immune cells. A 27-year-old man presented with a two-month history of night sweats, weight loss, and severe back pain. Radiological studies demonstrated an osteolytic lesion compressing the subarachnoid space at the T11 level. Posterolateral fusion with decompression was performed and a pathologic examination confirmed lymphoblastic lymphoma of the B-cell precursor type. To our knowledge, this is the first report of solitary lymphoblastic lymphoma from B-cell precursors in of the thoracic spine. Herein, we discuss the presenting symptoms and the management of this rare case of lymphoblastic lymphoma.
Primary bone lymphoma is an uncommon tumor that accounts for approximately 4-5% of extra-nodal lymphomas and less than 1% of all non-Hodgkin's lymphomas9). Furthermore, primary vertebral locations account for only 1.7% of all primary bone lymphomas, and the vast majority occur in short bones, with a predilection for the scapula, ileum, femur, and tibia11). Lymphoblastic lymphoma is a rare type of non-Hodgkin's lymphoma, and is the result of abnormality in adaptive immune cells, typically T-cells. To the best of our knowledge, this is the first report of solitary lymphoblastic lymphoma involving only thoracic spine. Here, we report a unique case of solitary lymphoblastic lymphoma of the B-cell precursor type involving only the thoracic spine. Surgical decompression and stabilization were essential to preserve function and maintain quality of life. We present a successful and requisite strategy for the management of this unique clinical presentation.
A 27-year-old man had progressively worsening back pain for 2 months. He had a history of mild back pain over the previous 2 years but the back pain had progressively worsened without any traumatic episode. The back pain worsened with activity, and he achieved relief by lying down. He also complained of night sweats and progressive weight loss of more than 10 kg over 4 months. A physical examination revealed no paresthesia or muscle weakness of the legs, no bowel or bladder symptoms, and the patient was able to straighten and raise his legs. Blood tests including erythrocyte sedimentation rate and C-reactive protein were within normal range. A computed tomography (CT) scan of the thoracolumbar spine showed lytic destruction in the body and right pedicle of T11. However, canal compromise by bony fragment was not detected (Fig. 1). Magnetic resonance imaging of the spine showed abnormally high signal changes in the T11 vertebral body and right pedicle with spinal cord compression by soft tissue extension (Fig. 2). Under a preliminary diagnosis of a primary bone tumor or metastasis, radionuclide bone scintigraphy (99m TC MDP) and positron emission tomography (PET)-CT were performed, but failed to depict an extraspinal lesion (Fig. 3). Cerebrospinal fluid examination revealed no abnormality. The patient then proceeded to surgery. Posterior decompression and fixation with instrumentation were performed. Histological specimen analysis findings were consistent with an aggressive lymphoblastic lymphoma of premature B-cell origin (Fig. 4). The tumor was CD10+ and CD99+ but negative for other markers. Postoperatively, marked pain relief was achieved and early mobilization while wearing a thoracolumbosacral orthosis was encouraged. The patient was transferred to our hematology and medical oncology department for chemo- and radiotherapy. He was performed 4 cycles of chemotherapy using Hyper CAVD regimen, followed by radiotherapy. At one year after surgery, he was pain free and able to return to full time work.
Lymphoma is a cancer of the lymphocytes, a type of sell that forms part of the immune system. Typically, it presents as a solid tumor of lymphoid cells. It can also affect other organs in which case it is referred to as extranodal lymphoma. The latest classification by the WHO (2008) lists 70 different forms of lymphoma divided in four broad groups3,5,14). The term lymphoma is used when the process is confined to a mass lesion with no or minimal evidence of peripheral blood and BM involvement3). Primary bone involvement at time of presentation is uncommon in non-Hodgkin lymphoma. The accepted definition of primary bone lymphoma is bone involvement without evidence of systemic involvement6). This form of non-Hodgkin's lymphoma is especially rare, and accounts for only 1% of all cases, and of these, primary vertebral locations account for just 1.7% of primary bone lymphomas4). Our patient presented with spinal compression from an osseous lesion consistent with an origin at the T11 vertebral body. No other origin of disseminated or extraspinal disease was observed by PET-CT or radionuclide bone scintigraphy. Primary bone lymphoma is often characterized by osteolytic defects, but these may be overlooked on plain radiographs. Due to its rarity, the true diagnosis is only established by histopathologic examination, and it is an essential to obtain tissue cores for histopathologic examination. Local pain and Type B symptoms, such as, generalized fatigue, night sweats, and weight loss are common1). When lymphoma involves the spine, it is more commonly found to be isolated in the epidural space due to secondary spread. Small case series of lymphoma with a spinal epidural origin have been reported, but these were primarily thoracolumbar in location and thought to result from an epidural, rather than a bony origin7,8). It is believed that primary epidural lymphomas may derive from normal lymphoid tissue in the epidural space12). Regardless of the spinal level or site of origin, patients with spinal lymphoma are at risk of neurological deterioration. The clinical manifestations of a compressive spinal mass may be pain, motor weakness, sensory deficits, and potential bowel or bladder dysfunction, and if left untreated, these may progress to paralysis. The treatment of these lesions is often multifactorial, and includes surgery, radiotherapy, and chemotherapy. Primary lymphoma of bone usually responds well to a combination of radio- and chemotherapy regimens, and an overall response rate of 94% and a 5-year survival rate better than that achieved by most other primary osseous malignancies have been reported2). Peng et al.10) also reported that combined chemotherapy and radiotherapy is the ideal treatment for primary non-Hodgkin's lymphoma of the spine, where as the survival is not influenced by the surgical or non-surgical treatment. In cases of severe pain or neurological deficits, however, early surgical decompression and stabilization is mandatory13). It is important that combined chemotherapy and radiotherapy followed by surgical decompression depending on individual priorities in the indications for operation on primary lymphoblastic lymphoma of spine with neurologic compression.
References
1. Anderson T, Chabner BA, Young RC, Berard CW, Garvin AJ, Simon RM, et al. Malignant lymphoma. 1. The histology and staging of 473 patients at the National Cancer Institute. Cancer. 1982; 50:2699–2707. PMID: 7139563.

2. Baar J, Burkes RL, Bell R, Blackstein ME, Fernandes B, Langer F. Primary non-Hodgkin's lymphoma of bone. A clinicopathologic study. Cancer. 1994; 73:1194–1199. PMID: 8313322.

3. Borowitz MJ, Chan JKC. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri S, Stein M, editors. B lymphoblastic leukaemia/lymphoma, not otherwise specified. WHO classification of tumors of haematopoietic and lymphoid tissues. 2008. ed 4. New York: Jon Wiley & Sons;p. 168–170.
4. Boukobza M, Mazel C, Touboul E. Primary vertebral and spinal epidural non-Hodgkin's lymphoma with spinal cord compression. Neuroradiology. 1996; 38:333–337. PMID: 8738091.

5. Esin S, Tarim E, Abali H, Kardes O, Kocer EN, Alkan O. Management of precursor B-lymphoblastic lymphoma/leukaemia of thoracic spine in a pregnancy presenting with acute paraplegia. J Obstet Gynaecol. 2012; 32:485–486. PMID: 22663326.

6. Farrés MT, Dock W, Augustin I, Windhager R, Riegler M, Eibenberger K, et al. [The radiologic clinical picture of primary bone lymphoma]. Rofo. 1993; 158:589–593. PMID: 8507852.
7. Hyun SJ, Kim YB, Yu H, Hong HJ. Central nervous system involvement of acute lymphoblastic leukemia. J Korean Neurosurg Soc. 2006; 40:54–57.
8. Lyons MK, O'Neill BP, Marsh WR, Kurtin PJ. Primary spinal epidural non-Hodgkin's lymphoma : report of eight patients and review of the literature. Neurosurgery. 1992; 30:675–680. PMID: 1584377.
9. Mulligan ME, McRae GA, Murphey MD. Imaging features of primary lymphoma of bone. AJR Am J Roentgenol. 1999; 173:1691–1697. PMID: 10584821.

10. Peng X, Wan Y, Chen Y, Chen L, He A, Liao W, et al. Primary non-Hodgkin's lymphoma of the spine with neurologic compression treated by radiotherapy and chemotherapy alone or combined with surgical decompression. Oncol Rep. 2009; 21:1269–1275. PMID: 19360303.

11. Rathmell AJ, Gospodarowicz MK, Sutcliffe SB, Clark RM. The Princess Margaret Hospital Lymphoma Group. Localized extradural lymphoma : survival, relapse pattern and functional outcome. Radiother Oncol. 1992; 24:14–20. PMID: 1620883.

12. Russel DS, Rubinstein LJ. Pathology of Tumours of the Nervous System. 1989. Baltimore: Williams and Wilkins.
13. Young RF, Post EM, King GA. Treatment of spinal epidural metastases. Randomized prospective comparison of laminectomy and radiotherapy. J Neurosurg. 1980; 53:741–748. PMID: 7441333.
14. Zheng JS, Wang M, Wan S, Zhou YQ, Yan M, Chen QF, et al. Isolated primary non-Hodgkin's lymphoma of the thoracic spine : a case report with a review of the literature. J Int Med Res. 2010; 38:1553–1560. PMID: 20926031.

Fig. 1
Computed tomography scans of the patient. Computed tomography scans show lytic destruction of vertebral body and right pedicle at T11.
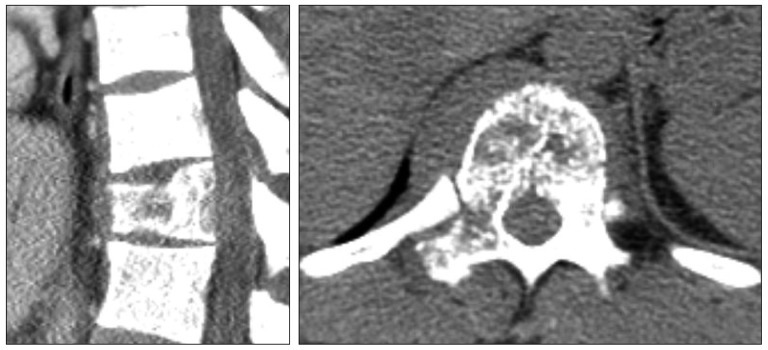
Fig. 2
Magnetic resonance images of the patient. T2-weighted sagittal magnetic resonance images reveal abnormally high signal intensity in the T11 vertebral body and spinal cord compression by soft tissue extension.

Fig. 3
Radionuclide bone scintigraphy and positron emission tomography. A : Radionuclide bone scintigraphy using MDP 99mTechnetium shows intense, uptake in the T11 vertebral body without systemic involvement. B : Positron emission tomography clearly depicts the hypermetabolic lesion at T11.
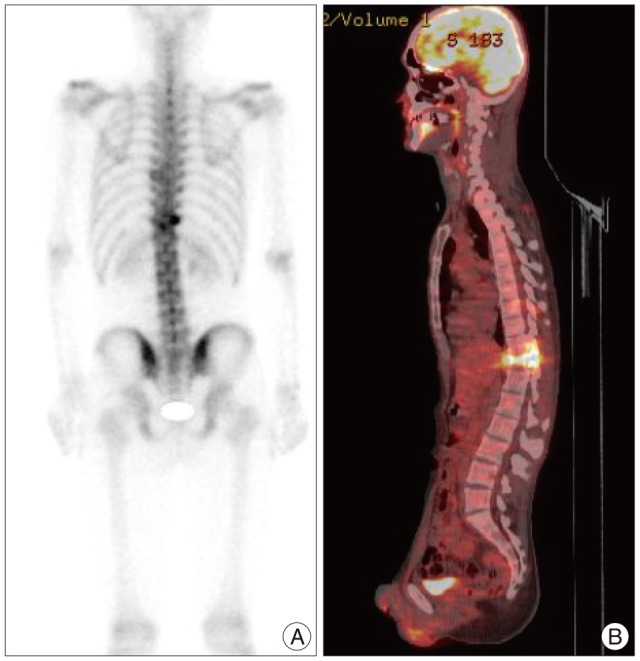
Fig. 4
Histopathological examination of the patient. A : On hematoxylin and eosin staining, biopsy material shows malignant small round cells infiltrating bone and soft tissue in low power field. B : In high power field, malignant small cells with scant cytoplasm observed fine chromatin, convoluted nuclear membrances. C and D : Immunohistochemical studies show positivity in CD10 (C) and CD99 (D). The tumor was compatible with malignant lymphoma, precursor B cell lineage.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download